Saphenous vein graft aneurysm is a rare complication after coronary artery bypass surgery. It is defined as a localized dilatation of the vessel to 1.5× the expected normal diameter. We report a case of 67-year-old man who presented with angina 23 years after coronary artery bypass graft. He was found to have a giant saphenous vein graft aneurysm to diagonal artery compressing the left internal mammary artery graft to the left anterior descending artery. The patient underwent aneurysm resection with satisfactory outcome.
The most recent review performed in 2010 reported 209 cases of saphenous vein graft (SVG) aneurysms since 1966 predominantly men with average age around 65 years. Giant SVG aneurysms are defined as abnormally expanded space >4 cm in diameter occupying the vascular structure. The purpose of this case report is to highlight a rare and lethal complication of saphenous vein graft after coronary artery bypass grafting (CABG).
Case Description
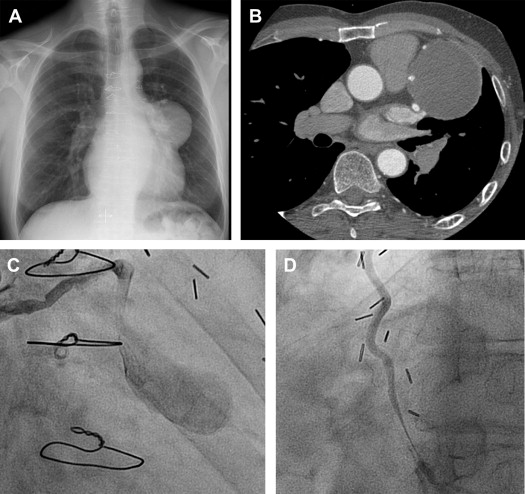
A 67-year-old presented with angina pectoris 22 years after coronary artery surgery. He had previously received an autologous long saphenous vein graft to distal right coronary artery, diagonal and a left internal mammary artery (LIMA) to the left anterior descending artery (LAD). A chest x-ray showed an abnormal opacity on the left side of the heart suggestive of an aneurysm ( Figure 1 ). Further evaluation with computed tomography showed a giant aneurysm measuring around 9 × 5 cm in size ( Figure 1 ). His angiogram revealed an aneurysm of long SVG to diagonal with compression of the LIMA to LAD ( Figure 1 ). He was referred for surgery. After the establishment of cardiopulmonary bypass, a giant aneurysm of the long SVG measuring 9 × 5 cm was identified. The SVG aneurysm was dissected from the LIMA where it was compressing it. The feeding SVG was detached from the aorta. The SVG aneurysm was opened and a large amount of thrombus was removed. A segment of SVG was grafted distal to the LIMA anastamosis. The patient came off bypass without any problem. The patient had a smooth postoperative recovery and remains symptom free 6 months after the surgery.
Comments
SVG aneurysm is a very rare complication of CABG with potential lethal complications. SVG aneurysms are classified as true and pseudoaneurysms. True aneurysm involves dilatation of the vessel whereby all 3 histological tissue wall layers are intact. Pseudoaneurysm are typically saccular, occur early in the postoperative period, and are near the sites of anastamosis. Kalimi et al reviewed 50 cases of SVG aneurysm. Thirty patients had true aneurysms, 17 had pseudoaneurysms, and the remaining 3 could not be categorized into either group. Many patients in the true aneurysm group were asymptomatic. In the pseudoaneurysm group, chest pain was the most common presenting complaint (29%). The timing of presentation after CABG was similar in both the groups, the true aneurysm group having a mean of 10 years and the pseudoaneurysm group 9.7 years. Ramirez et al in their review of 209 patients in 2010 reported chest pain as the most common presenting symptoms (43.5%), followed by incidental finding in 35.4% of the cases.
The cause of SVG aneurysm after CABG remains unclear from the published reports. Suggested causes include systemic hypertension, infection (mycotic), poor vein quality or varicosity at the time of the first operation, and poor handling of the vein. Atherosclerosis is an important underlying pathologic mechanism. Sahouri and Steele reported a giant aneurysm containing atherosclerotic plaque and focal calcification. Ferreira et al encountered a giant aneurysm of SVG that was filled with atheromatous tissue. Persistent hyperlipidemia after a bypass operation is also considered an important contributing factor to the formation of giant aneurysms.
The case that we report appears to be only the second case report of an SVG aneurysm compressing the LIMA to LAD graft. The origin of this condition is unclear, but it is possible that an adequate control of long-term hypertension and hyperlipidemia together with careful harvesting of the SVG and avoidance repairs of varicosity may reduce its incidence.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


