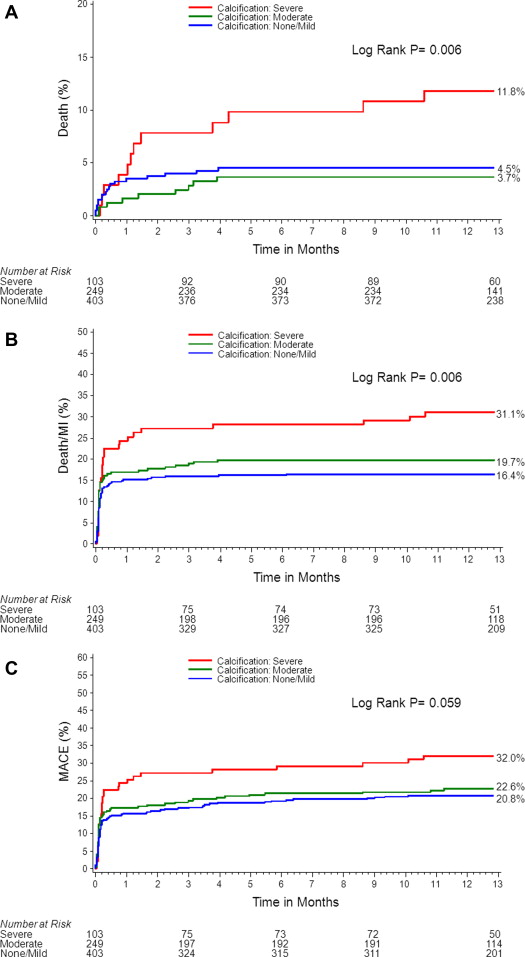
The treatment of calcified coronary lesions by percutaneous coronary intervention has been shown to be associated with poor outcomes and an increased rate of complications. However, the impact of coronary calcification in patients undergoing coronary artery bypass grafting (CABG) is unknown. A total of 755 patients presenting with acute coronary syndrome in the Acute Catheterization and Urgent Intervention Triage Strategy trial underwent CABG. Patients were divided into 3 groups according to the presence and extent of coronary calcifications (lesion level: severe, moderate, none to mild) as assessed by an independent angiographic core laboratory. Major ischemic and bleeding outcomes were assessed at 30 days and 1 year. Severe calcification was found in 103 patients (13.6%), moderate calcification in 249 patients (33.0%), and none-to-mild calcification in 403 patients (53.4%). The presence of severe calcification compared with moderate or none to mild was associated with a significantly higher unadjusted rate of death (11.8% vs 3.7% vs 4.5%, p = 0.006), death or myocardial infarction (MI; 31.1% vs 19.7% vs 16.4%, p = 0.006), and major adverse cardiac event (MACE; 32.0% vs 22.6% vs 20.8%, p = 0.059) at 1 year. By multivariate analysis, severe calcification (vs nonsevere calcification) was identified as an independent predictor of 1-year MACE (hazard ratio 1.49, 95% confidence interval 1.01 to 2.21, p = 0.04) and death or MI (hazard ratio 1.77, 95% confidence interval 1.18 to 2.66, p = 0.006). In conclusion, the presence of severe coronary calcification was associated with worse outcomes after CABG, including an increased risk of death. The presence of severe coronary calcification was identified as an independent predictor of MACE and death or MI 1 year after CABG.
Coronary artery disease involving heavily calcified lesions has been shown to be associated with worse short- and long-term outcomes after percutaneous coronary intervention. After surgical revascularization, several baseline patient characteristics such as age, peripheral vascular disease, low ejection fraction, elevated logistic EuroSCORE, and Parsonnet score have been identified as predictors of poor outcomes. However, to the best of our knowledge, the impact of the presence and severity of coronary calcification in patients treated with coronary artery bypass grafting (CABG) has not been investigated. Therefore, we sought to assess the prognostic impact of coronary artery calcification in patients undergoing CABG in the large-scale Acute Catheterization and Urgent Intervention Triage Strategy (ACUITY) trial.
Methods
The design of the ACUITY trial has been previously described. In brief, 13,819 patients with moderate and high-risk non–ST-segment elevation acute coronary syndrome undergoing an early invasive strategy were randomized to heparin (unfractionated or enoxaparin) plus a glycoprotein IIb/IIIa inhibitor, bivalirudin plus glycoprotein IIb/IIIa inhibitor, or bivalirudin alone. Angiography was performed in all patients within 72 hours of randomization. Depending on the coronary anatomy and the operator preference, patients then underwent percutaneous coronary intervention, CABG, or medical therapy. Patients were followed up for 1 year after randomization. A 5-day clopidogrel washout period was recommended before surgery.
The primary end points were 30-day rates of net adverse clinical events and the 30-day and 1-year rates of major adverse cardiac events (MACEs). MACE was defined as occurrence of death, myocardial infarction (MI), or unplanned ischemia-driven target vessel revascularization. Net adverse clinical event was defined as occurrence of death, MI, unplanned revascularization for ischemia, or clinically significant bleeding (ACUITY scale). Periprocedural MI diagnosis after CABG was defined by creatine phosphokinase (CPK)-MB (or CPK) ≥10 upper limit of normal within 24 hours of CABG and increased at least 50% over the most recent pre-CABG levels or any CPK-MB (or CPK) ≥5 upper limit of normal within 24 hours of CABG and increased at least 50% over the most recent pre-CABG levels and new significant (≥0.04 second) Q waves in ≥2 contiguous electrocardiographic leads. Once the enzymatic criteria for MI were met, a Q-wave MI was diagnosed if new pathologic Q waves developed in ≥2 electrocardiographic contiguous leads were adjudicated by the clinical events committee. An MI not meeting this definition was considered a non–Q-wave MI. MI results (periprocedural and spontaneous) were also reported at 72 hours, 30 days, and 1 year. Quantitative coronary angiography was performed by experienced core laboratory technicians blinded to randomization and clinical outcomes (Cardiovascular Research Foundation, New York, New York). Coronary calcifications were stratified visually into severe, moderate, and none to mild using readily apparent densities noted within the vascular wall at the stenosis level (diameter stenosis of ≥50% in all epicardial vessel of >1.5 mm diameter). Moderate lesion calcification was defined as radiopaque densities noted during the cardiac cycle involving only 1 side of the vascular wall, whereas severe lesion calcification was defined as radiopaque densities noted without cardiac motion before contrast injection generally involving both sides of the arterial wall. All major adverse events were adjudicated by an independent clinical events committee blinded to treatment assignment.
Binary variables are summarized as percentages or rate and were compared among groups with chi-square test. Continues variables are summarized as mean ± SD or median (Q1, Q3) as appropriate and were compared among groups with analysis of variance and Kruskal-Wallis test. Outcomes were analyzed using the Kaplan-Meier time-to-event method and compared using the log-rank test. Stepwise Cox multivariate regression analysis was performed with entry and exit criteria set at p ≤0.1 to assess the association between coronary calcification severity and clinical end points, after confirmation that the proportional hazards assumption was met. Variables included into the multivariate models were carefully selected to avoid overfitting of the model. For death, the following covariates were included: calcification severity (severe vs nonsevere), age, weight, and renal insufficiency at baseline. For the analysis evaluating independent predictors of death or MI and MACE, the following covariates were included: calcification severity (severe vs nonsevere), age, renal insufficiency at baseline, previous CABG, hypertension, baseline cardiac biomarker elevation, ST-segment deviation of ≥1 mm, male gender, insulin-treated diabetes, current smoker, previous MI, white blood cell count, and baseline hemoglobin. Statistical analyses were performed using SAS, version 9.2 (SAS Institute, Cary, North Carolina). A p value <0.05 was considered statistically significant.
Results
A total of 755 patients from the ACUITY trial presenting with acute coronary syndrome underwent CABG. Severe coronary calcification was found in 103 patients (13.6%), moderate calcification in 249 (33.0%), and none-to-mild calcification in 403 (53.4%).
Baseline clinical characteristics, angiographic findings, and treatment randomization of patients stratified by calcification severity are summarized in Table 1 . Patients with severe calcification were more likely to be older, weigh less, be smokers, have hypertension, and have renal insufficiency at baseline. Angiographically, they were more likely to have higher number of coronary lesions and higher Thrombolysis In Myocardial Infarction risk score. There were no differences among groups in the rates of patients with 3-vessel disease. The administration of thienopyridines before initial catheterization was more frequent in the none-to-mild calcification group.
| Variable | Severe, n = 103 (%) | Moderate, n = 249 (%) | None to Mild, n = 403 (%) | p |
|---|---|---|---|---|
| Age (yrs), median (IQR) | 68.0 (61–78) | 65.0 (58–72) | 61.0 (54–69) | <0.0001 |
| Men | 71/103 (68.9) | 183/249 (73.5) | 312/403 (77.4) | 0.17 |
| Weight (kg), median (IQR) | 81 (71–93) | 83.99 (73–98) | 87.0 (78–98) | 0.003 |
| Diabetes mellitus | 42/103 (40.8) | 78/248 (31.5) | 141/401 (35.2) | 0.24 |
| Insulin diabetes | 15/103 (14.6) | 22/248 (8.9) | 42/401 (10.5) | 0.28 |
| Hypertension | 72/103 (69.9) | 174/249 (69.9) | 237/403 (58.8) | 0.007 |
| Hyperlipidemia | 60/101 (59.4) | 131/243 (53.9) | 203/391 (51.9) | 0.40 |
| Current smoker | 20/103 (19.4) | 69/248 (27.8) | 128/402 (31.8) | 0.04 |
| Previous MI | 24/100 (24.0) | 78/246 (31.7) | 95/387 (24.5) | 0.11 |
| Previous percutaneous intervention | 20/103 (19.4) | 71/247 (28.7) | 113/400 (28.3) | 0.16 |
| Previous CABG | 4/103 (3.9) | 14/249 (5.6) | 16/401 (4.0) | 0.59 |
| Renal insufficiency (<60 ml/min) | 28/94 (29.8) | 50/236 (21.2) | 51/369 (13.8) | 0.0007 |
| Baseline cardiac biomarker elevation | 60/98 (61.2) | 165/229 (72.1) | 263/374 (70.3) | 0.13 |
| Baseline troponin elevation | 55/94 (58.5) | 150/221 (67.9) | 248/363 (68.3) | 0.18 |
| ST-segment deviation ≥1 mm | 52/103 (50.5) | 95/249 (38.2) | 161/403 (40.0) | 0.09 |
| Baseline cardiac biomarker elevation or ST-segment deviation | 82/100 (82.0) | 189/233 (81.1) | 308/381 (80.8) | 0.96 |
| Thrombolysis In Myocardial Infarction risk score | ||||
| Low (0–2) | 6/79 (7.6) | 12/214 (5.6) | 41/344 (11.9) | 0.04 |
| Intermediate (3–4) | 41/79 (51.9) | 119/214 (55.6) | 202/344 (58.7) | 0.49 |
| High (5–7) | 32/79 (40.5) | 83/214 (38.8) | 101/344 (29.4) | 0.03 |
| Number with 2-vessel coronary artery disease | 17/103 (16.5) | 71/249 (28.5) | 75/403 (18.6) | 0.005 |
| Number with 3-vessel coronary artery disease | 79/103 (76.7) | 165/249 (66.3) | 289/403 (71.7) | 0.11 |
| Lesions per patient (mean ± SD) | 6.70 ± 2.82 | 6.39 ± 2.86 | 5.79 ± 2.63 | 0.002 |
| Ejection fraction %, median (IQR) | 61.40 (53.80–67.80) | 63.55 (56.35–71.25) | 64.75 (55.00–72.30) | 0.11 |
| Ejection fraction <35% | 5/76 (6.6) | 5/192 (2.6) | 10/326 (3.1) | 0.24 |
| Postrandomization medication | ||||
| Bivalirudin | 62/103 (60.2) | 158/249 (63.5) | 246/403 (61.0) | 0.78 |
| Unfractionated heparin | 27/103 (26.2) | 62/249 (24.9) | 85/403 (21.1) | 0.38 |
| Enoxaparin | 12/103 (11.7) | 27/249 (10.8) | 55/403 (13.6) | 0.55 |
| GP IIb/IIIa inhibitor | 44/103 (42.7) | 85/249 (34.1) | 133/403 (33.0) | 0.18 |
| Aspirin | 101/103 (98.1) | 248/249 (99.6) | 399/403 (99.0) | 0.38 |
| Thienopyridine | 35/103 (34.0) | 77/249 (30.9) | 162/403 (40.2) | 0.049 |
| Number of grafts performed, median (IQR) | 4.00 (3.00–4.00) | 3.00 (3.00–4.00) | 3.00 (3.00–4.00) | 0.22 |
| Arterial conduits performed | 71/102 (69.6) | 177/246 (72.0) | 292/400 (73.0) | 0.79 |
| Concurrent procedures performed | 13/102 (12.7) | 34/247 (13.8) | 43/399 (10.8) | 0.51 |
| Aortic valve replacement | 2/13 (15.4) | 4/34 (11.8) | 5/43 (11.6) | 0.93 |
| Mitral valve replacement | 3/13 (23.1) | 2/34 (5.9) | 3/43 (7.0) | 0.15 |
| Mitral valve repair | 0/13 (0) | 4/34 (11.8) | 4/43 (9.3) | 0.44 |
| Defibrillator | 0/13 (0) | 3/34 (8.8) | 1/43 (2.3) | 0.27 |
As listed in Table 2 , the presence of severe coronary calcification was associated with a nonsignificant trend toward higher rates of net adverse clinical events, MACEs, death, and death or MI at 30 days. Thirty-day bleeding event rates are listed in Table 3 . CABG-related bleeding and CABG-related transfusions were similarly frequent in all 3 groups. Protocol non–CABG-related major bleeding and non–CABG-related transfusion rates were significantly more frequent in the severe calcification group compared with the 2 other groups.
| Variable | Coronary Calcification | p | |||||
|---|---|---|---|---|---|---|---|
| Severe (A) (n = 103) | Moderate (B) (n = 249) | None to Mild (C) (n = 403) | All | A vs B | A vs C | B vs C | |
| 30 days | |||||||
| Net adverse clinical events | 27.2 (28) | 20.5 (51) | 16.6 (67) | 0.06 | 0.22 | 0.02 | 0.21 |
| MACE | 25.2 (26) | 17.3 (43) | 15.6 (63) | 0.09 | 0.11 | 0.03 | 0.56 |
| Death | 5.8 (6) | 1.6 (4) | 3.5 (14) | 0.11 | 0.03 | 0.29 | 0.16 |
| Cardiac death | 4.9 (5) | 1.6 (4) | 3.5 (14) | 0.21 | 0.08 | 0.52 | 0.16 |
| Noncardiac death | 1.0 (1) | 0.0 (0) | 0.0 (0) | 0.04 | 0.12 | 0.049 | — |
| Death or MI | 25.2 (26) | 16.9 (42) | 15.2 (61) | 0.06 | 0.09 | 0.02 | 0.52 |
| MI | 21.4 (22) | 15.7 (39) | 13.3 (53) | 0.12 | 0.23 | 0.04 | 0.35 |
| Q wave | 5.9 (6) | 3.2 (8) | 4.5 (18) | 0.52 | 0.26 | 0.58 | 0.42 |
| Non–Q wave | 15.6 (16) | 12.5 (31) | 8.8 (35) | 0.09 | 0.46 | 0.04 | 0.12 |
| Periprocedural ≤24 h | 1.9 (2) | 4.0 (10) | 2.0 (8) | 0.26 | 0.33 | 0.98 | 0.12 |
| MI ≤72 h | 12.6 (13) | 11.6 (29) | 7.3 (29) | 0.09 | 0.83 | 0.08 | 0.056 |
| Unplanned revascularization | 0.0 (0) | 0.8 (2) | 1.5 (6) | 0.37 | 0.36 | 0.21 | 0.43 |
| Percutaneous intervention | 0.0 (0) | 0.8 (2) | 1.0 (4) | 0.60 | 0.36 | 0.31 | 0.80 |
| CABG | 0.0 (0) | 0.0 (0) | 0.5 (2) | 0.41 | — | 0.47 | 0.26 |
| 1 Yr | |||||||
| MACE | 32.0 (33) | 22.6 (56) | 20.8 (83) | 0.059 | 0.07 | 0.02 | 0.55 |
| Death | 11.8 (12) | 3.7 (9) | 4.5 (18) | 0.006 | 0.004 | 0.007 | 0.58 |
| Cardiac death | 5.9 (6) | 2.8 (7) | 3.7 (15) | 0.39 | 0.17 | 0.35 | 0.52 |
| Noncardiac death | 6.3 (6) | 0.8 (2) | 0.8 (3) | 0.0002 | 0.003 | 0.0004 | 0.95 |
| Death or MI | 31.1 (32) | 19.7 (49) | 16.4 (66) | 0.006 | 0.03 | 0.001 | 0.28 |
| MI | 22.5 (23) | 16.5 (41) | 13.8 (55) | 0.10 | 0.22 | 0.03 | 0.31 |
| Q wave | 5.9 (6) | 3.2 (8) | 4.5 (18) | 0.52 | 0.26 | 0.58 | 0.42 |
| Non–Q wave | 16.7 (17) | 13.7 (34) | 9.3 (37) | 0.06 | 0.49 | 0.03 | 0.08 |
| Unplanned revascularization | 1.1 (1) | 4.3 (10) | 5.8 (22) | 0.14 | 0.16 | 0.06 | 0.39 |
| Percutaneous intervention | 1.1 (1) | 4.3 (10) | 5.3 (20) | 0.21 | 0.16 | 0.08 | 0.55 |
| CABG | 0.0 (0) | 0.0 (0) | 0.5 (2) | 0.41 | — | 0.47 | 0.26 |
| Variable | Coronary Calcification | p | |||||
|---|---|---|---|---|---|---|---|
| Severe (A) (n = 103) | Moderate (B) (n = 249) | None to Mild (C) (n = 403) | All | A vs B | A vs C | B vs C | |
| CABG major bleeding | 51.5 (53) | 54.0 (134) | 54.3 (218) | 0.85 | 0.75 | 0.60 | 0.75 |
| CABG minor bleeding | 15.6 (16) | 14.9 (37) | 13.0 (52) | 0.73 | 0.86 | 0.51 | 0.53 |
| CABG-related blood product transfusion | 43.7 (45) | 43.9 (109) | 44.3 (178) | 0.96 | 0.91 | 0.95 | 0.77 |
| Non–CABG-related major bleeding | 5.9 (6) | 3.6 (9) | 1.5 (6) | 0.04 | 0.36 | 0.01 | 0.08 |
| Non–CABG-related minor bleeding | 9.7 (10) | 14.9 (37) | 12.5 (50) | 0.41 | 0.20 | 0.44 | 0.39 |
| TIMI non–CABG-related major bleeding | 2.9 (3) | 0.0 (0) | 0.5 (2) | 0.008 | 0.007 | 0.03 | 0.26 |
| TIMI non–CABG-related minor bleeding | 9.7 (10) | 8.0 (20) | 4.8 (19) | 0.10 | 0.64 | 0.06 | 0.09 |
| Non–CABG-related blood product transfusion | 5.9 (6) | 2.0 (5) | 0.7 (3) | 0.003 | 0.06 | 0.0005 | 0.16 |
The presence of severe calcification was associated with significantly higher 1-year rates of death (11.8% vs 3.7% vs 4.5%, p = 0.006), MACE (32.0% vs 22.6% vs 20.8%, p = 0.059), and death or MI (31.1% vs 19.7% vs 16.4%, p = 0.006) compared with moderate or none-to-mild calcifications, respectively ( Table 2 and Figure 1 ). Figure 2 shows cumulative event rates according to the impact of coronary calcification restricted to patients with 3-vessel disease.