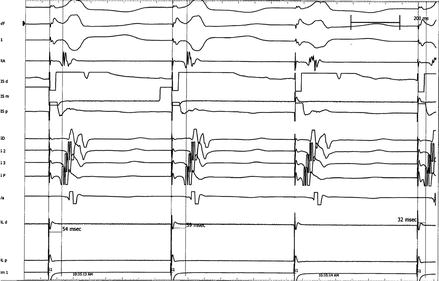
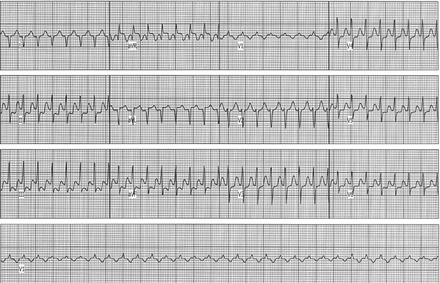
Figure 3.1
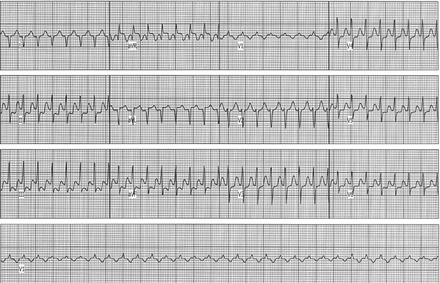
ECG of AVNRT. Notice retrograde P waves forming a pseudo S pattern in several leads
This short RP tachycardia involves a reentry mechanism within the AV node and is based on the concept of dual AV nodal physiology. The reentrant circuit is dependent on the presence of at least two functional pathways with differing refractoriness and conduction properties. Typical AVNRT, the most frequent form, uses the slow pathway for antegrade conduction, and the fast pathway for retrograde limb to complete the circuit and is classically triggered by an APC blocking in the fast pathway but conducting slowly down the slow pathway allowing retrograde recovery of the fast pathway to produce a closed loop (Fig. 3.2) [3, 4].
Figure 3.2
Diagram of dual pathway physiology within the AV node and initiation via an APC
The two pathways do not seem separable by pathologic examination but the characteristics are encoded within the cellular distribution, and the characteristics for electrophysiology properties are functional [4–6]. The differentiation of function within the AV node was originally discovered from analyzing atrial pacing data using progressively shorter atrial extrastimuli cycle lengths (A1-A2) and measuring the A-H conduction times, during which it was noted that a large “jump” of at least 50 ms occurred at a specific 10 ms decrement in A1-A2 cycle length after which the resumption of gradual normal decremental conduction would continue on a different slope (Fig. 3.3). This reproducible finding confirmed the functional presence of dual pathway physiology and provides the substrate for a reentry based tachycardia such as AVNRT. This mechanism also explains the surface ECG findings of an APC with sudden PR prolongation preceding initiation of a short RP tachycardia with evidence of retrograde P wave conduction. The intracardiac findings confirm a jump in AH interval meeting the dual pathway criteria with initiation of a short RP tachycardia.
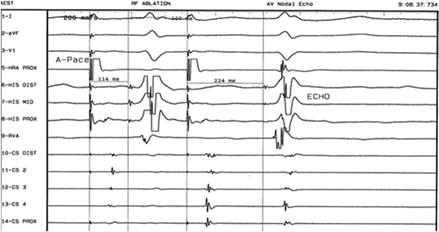
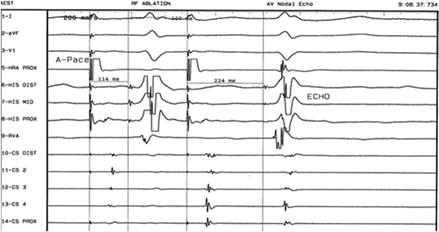
Figure 3.3
Paced atrial extrastimuli with subsequent “jump” in AH interval and one beat reentry. This is referred to as an echo
The atrial electrogram on the His catheter is earliest since the return limb in the typical form involves the anterior pathway located close to the anteroseptal region.
The fast and slow pathways are considered to anatomically located within the triangle of Koch during which the earliest retrograde conduction to the atrium is noted. In typical AVNRT, the earliest retrograde atrial activation EGM is noted in the apex of the triangle, and in the OS of the coronary sinus during the atypical form. It is important to note that not all cases of AVNRT demonstrate clear dual AV nodal physiology during baseline EP studies, since the “jump” is heavily influenced by timing and autonomic tone.
Clinical Presentation
Patients with AVNRT often present with a history of paroxysmal palpitations, that may be triggered after bending down to pickup a heavy object, or preceded by a sensation of single “skipped beats”. It is interesting to note that many adolescent patients instinctively perform their own vagal maneuvers to terminate the SVT including bearing down or less commonly, standing on their head terminating the tachycardia via vagal like mechanism. Adults may describe a history of palpitations during their teenage years, the frequency of which may have decreased for many years, only to return later in life. While the tachycardia cycle length may decrease in a subgroup of patients with age, the ability to tolerate the fast rates may not. Common symptoms include sudden onset and termination, sensation of racing or palpitations, chest heaviness or unusual sensation in neck and throat prompting a cough. While the SVT may last only minutes, it may be prolonged and incessant prompting an emergency room visit. Intravenous adenosine is often used in the pre-hospital and hospital setting with excellent success in terminating the tachycardia.
Clinical Management
There are three decision pathways: Observation, Pharmacologic, and Catheter ablation. The individual patient’s circumstances need to be included in the process. For example, a single episode of SVT and no history of symptoms may benefit from observation or event monitoring with no pharmacologic or invasive intervention. Catheter ablation is generally curative and is the preferred path for patients with recurrent episodes that are symptomatic, limited by possibility of having prolonged episodes requiring emergency services, and/or occupation that may increase patient risk for injury should he or she develop sustained SVT that is symptomatic. Pharmacologic management primarily rely on drugs such as beta receptor and calcium channel antagonists that modulate AV node function to reduce the probability of SVT events over long periods of time. The next level of pharmacologic intervention would include antiarrhythmics such as flecainide or propafenone, which concomitantly have a higher side effect profile.
Electrophysiology Study and Ablation
Several forms of AVNRT have been described during EP studies including slow-fast (typical) and fast-slow (atypical). The correct diagnosis is critical to determining if and where an RF ablation should be delivered. The goal is to eliminate the appropriate limb of the reentry circuit while minimizing risk to the normal conduction system. When performing the EP study for SVT, it is important to maintain a systematic approach to avoid missing key maneuvers and improving your diagnostic accuracy. We recommend that physicians customize and adopt a framework on which to approach all EP studies. The following is only an example of possible considerations during an EP study:
1.
Document baseline sinus rhythm, AH, HV intervals. Any preexcitation?, is the AV conduction normal?
2.
1:1 A-V conduction
3.
AV node function – Effective refractory periods using programmed stimulation
5.
1:1 V-A conduction: Is it concentric? Is it decremental?
7.
Attempt burst pacing and varying atrial and ventricular extrastimuli.
8.
Add agents such as isoproterenol or atropine to alter autonomic tone to increase the probability of inducing SVT.
In typical AVNRT, the ECG reveals a short RP narrow complex regular tachycardia in which the P wave is buried within the terminal segment of the QRS complex and not clearly visible. Intracardiac electrograms demonstrate that the earliest retrograde activation is often seen on the His Bundle electrode, though it may be occasionally seen earlier along the posterior septum (Fig. 3.5). The QA interval is relatively short. One must always consider the less probable presence of a left sided fast pathway.
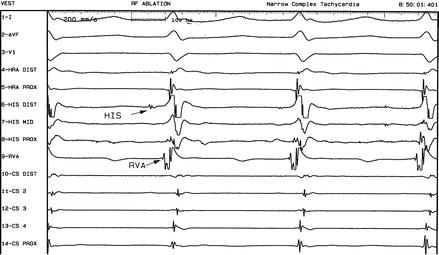
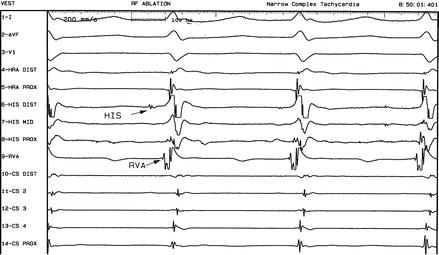
Figure 3.5
Atrioventricular nodal reentry tachycardia
Pacing maneuvers during tachycardia are powerful tools for correctly diagnosing the circuit. For example, rapid ventricular pacing causing dissociation between the atrium and ventricle provides a clue. In this setting, the atrial cycle length remains unchanged thus ruling out AVRT as the etiology of the ongoing tachycardia but does not rule out arrhythmias such as atrial tachycardia. Another maneuver during 1:1 conduction involves introducing single premature ventricular beats at a time during His refractoriness and determining if it resets the atrial activation. Parahisian pacing also aids in determining the presence of a concealed septal bypass tract [7, 8].
It is important to recognize that there is a small but real risk of damaging the AV node fast pathway causing high grade AV block that may be irreversible. Fluoroscopic views maximizing the distance between the anteroseptum and the posteroseptal region near the coronary sinus where the slow pathway is localized reduces risk. Additionally, 3D mapping in which the His bundle is carefully marked can reduce risk. During RF delivery, monitoring VA conduction during junctional beats as well as the A-H-V conduction during sinus will provide clues to unintended conduction system damage.
Atrial Tachycardia
Atrial tachycardias originate from cells depolarizing within the atria and function independently of the AV node conduction system and ventricle. The anatomic site of origin can be anywhere in the left and right atria. An atrial tachycardia may originate from one or more foci and presents on ECG as an SVT with evidence of p waves that may or may not have a fixed relationship to the QRS. The surface ECG usually reveals p waves with vectors different from the sinus node activation pattern (Figs. 3.6 and 3.7). Normal sinus rhythm presents with P waves that are positive in I, II, and negative in AVR. A tachycardia originating near the sinus node or from within the sinus tissue, it would appear similar to sinus activation pattern and the possibility of sinus node reentry should be considered. The atrial cycle length of atrial tachycardias are generally longer than atrial flutter cycle lengths that are often ~200–250 ms. The P wave morphology of atrial tachycardias often appear similar to sinus P waves versus peaked saw tooth pattern waves seen in atrial flutter. On occasion, we find that what appeared to be an atrial tachycardia on surface ECG was found to be an atypical atrial flutter during an EP study.
 < div class='tao-gold-member'>
< div class='tao-gold-member'>




Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree