TRANSSEPTAL CATHETERIZATION GUIDED BY TRANSTHORACIC AND TRANSESOPHAGEAL ECHOCARDIOGRAPHY
MATTHEW P. SMELLEY, BRADLEY P. KNIGHT
Since the introduction of transseptal puncture and catheterization (TSP) in 1959,1–7 the technique has evolved from a means of directly measuring left-sided cardiac pressures to a means of providing therapy for left-sided arrhythmias and mitral valve disease. Transseptal catheterization, however, is associated with a small risk of complications, and is not successful in every case. One review of 1279 transseptal punctures at a single center documented a success rate of 90% with a major complication rate of 1.3%, including cardiac tamponade (1.2%), systemic embolization (0.08%), and aortic perforation (0.08%).8 A second single-center experience of 278 procedures listed an overall success rate of 91% with a complication rate of 1.1% for aortic perforation, 3.2% for systemic embolization, and 0.7% for tamponade.9 In terms of short- and long-term outcomes up to 18 months, there was no difference among transseptal procedures performed for the diagnosis of valvular heart disease, catheter ablation of arrhythmias, and mitral valvuloplasty. Patients undergoing valvuloplasty had a higher chance of a residual atrial septal defect, but this occurrence did not affect long-term prognosis.10 These three studies used fluoroscopic landmarks alone and not echocardiography to perform the transseptal puncture.
In skilled hands, TSP can be performed successfully using only fluoroscopic landmarks for guidance. However, congenital and acquired anatomic variations and the potential for life-threatening complications has led to a demand for methods of directly visualizing the interatrial septum to improve the success rate in all cases and to avoid the chance of an unwanted event. Transthoracic (TTE), transesophageal (TEE), and intracardiac echocardiography (ICE) have been used to provide additional imaging during TSP. ICE catheterization provides direct visualization of the interatrial septum during TSP,11–14 but the universal use of an ICE catheter is problematic due to the high cost of the equipment and the need for technical training. With these limitations in mind, there remains a role for TTE and TEE guidance. This chapter will focus on the use of TTE and TEE for transseptal puncture. Specific references to 3-D TEE imaging will be made. The use of ICE is discussed in chapter 8.
Anatomy Pertinent to Transseptal Catheterization
The safest place to gain access to the left atrium (LA) from the right atrium (RA) is through the fossa oval is (FO). The FO is found in the posterior interatrial septum, and is surrounded by a muscular limbus. The anatomy of the FO and the immediate surrounding cardiac structures can vary based on congenital and acquired heart disease.
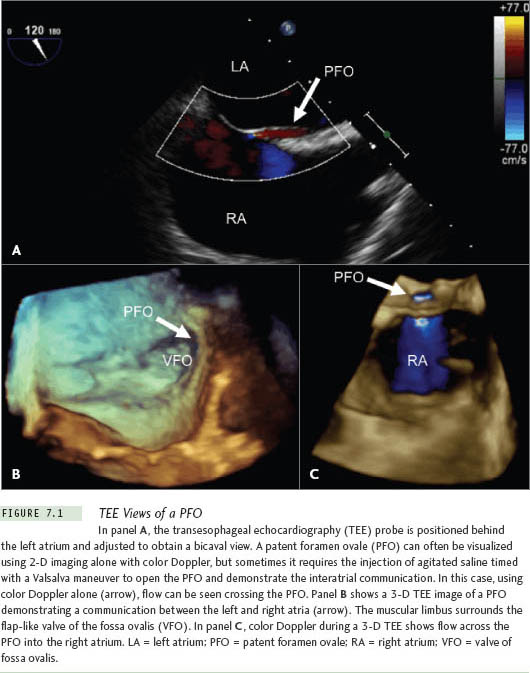
A patent foramen ovale (PFO) (Figure 7.1) can be found in the range of 25% to 30% of patients and allows direct access to the left atrium.15–17 During an autopsy study of 965 normal hearts, a PFO was found in 27% of patients. The incidence and size of the PFO did not vary significantly between genders. However, the incidence progressively declined with age, while the size of the PFO increased with age from a mean of 3.4 mm in the first decade of life to 5.8 mm in the tenth decade of life.15
Atrial septal aneurysms are typically defined as an oscillating aneurysmal dilatation of the septum with at least 10 mm to 15 mm of movement into either atrium during the cardiorespiratory cycle.16,17 The prevalence of these aneurysms varies depending upon the study technique, from 1% at autopsy,18 0.22% to 4.0% with echocardiography,16,17,19,20 and 4.9% during cardiac surgery.21 The presence of an aneurysm increases the risk of LA wall perforation during TSP,22 and, therefore, should be noted when using echocardiography at the beginning of the procedure. In diseased hearts, the normal anatomy can be distorted, potentially leading to an increased rate of complications if fluoroscopic landmarks are used alone. Patients with a dilated aortic root, an enlarged atria, prior cardiac surgery, or kyphoscoliosis may have a dysmorphic FO.
Echocardiography has the advantage over radiographic imaging by being able to image the soft tissue variations described for both congenital and acquired heart disease. Direct visualization of the FO provides reassurance to the operator, and may be associated with a reduction in the risk of complications, especially in patients with altered atrial anatomy.
Technique for Transseptal Puncture Using Supplemental Echocardiographic Guidance
In our laboratory, the majority of transseptal catheterizations are for LA ablation procedures, usually atrial fibrillation. These procedures are typically performed using intravenous sedation. For this reason, in our lab ICE is used more often than TEE to guide the procedure. However, endotracheal intubation and general anesthesia is occasionally necessary for patients who are obese, have a high-risk airway for sedation, have a history of being difficult to sedate, or request complete amnesia for the procedure. When general anesthesia is used, the procedure can be guided easily by TEE. With TEE guidance, the esophagus is intubated after anesthesia is induced, and the TEE probe is advanced into position behind the LA.
Ultrasound techniques supplement, but do not substitute for, standard fluoroscopic techniques. It is recommended that the physician follow standard methods and use ultrasound to confirm that the transseptal apparatus is properly positioned before puncturing the septum. Also, a survey of the cardiac anatomy should be performed using echocardiography to confirm the orientation of the septum in relationship to the aorta and posterior wall of the atria.
When the TSP is performed during an electrophysiology procedure, a His-bundle and coronary sinus (CS) catheter can be used to provide additional fluoroscopic landmarks and help make adjustments to the angulation of the left anterior oblique (LAO) and right anterior oblique (RAO) cameras. A quadripo-lar catheter positioned correctly over the His bundle can also approximate the noncoronary cusp of the aortic valve. It is this cusp of the aorta that is adjacent to the interatrial septum (Figure 7.2). A CS catheter can help define on fluoroscopy where the atrioventricular groove is located and mark the posterior-inferior border of the atrium. If the atrial and ventricular electrograms on the CS catheter are of similar size, then the catheter is within the body of the CS and not in a ventricular branch. The CS catheter then approximates the posterior left atrium and mitral valve.
In the LAO view, the His-bundle catheter should be pointed directly at the image intensifier along the septum. In the RAO view, the CS catheter is perpendicular to the image. In one study, the use of this RAO technique with a pigtail catheter in the aorta demonstrated a transseptal puncture success rate of 99% with a nonfatal complication rate of 2.8%.23 This success rate is considerably higher than the 90% to 91% success rates previously described using fluoroscopic landmarks alone.8,9 However, when using ultrasound to guide TSP, placement of a catheter in the aorta as a landmark is probably not necessary, and is not done in our laboratory.
The physician should be familiar with the transseptal apparatus. Various transseptal introducers combine different sheath lengths with their dilators. The typical Brock-enbrough needle is 71 cm in length with an arrow at the hub that points in the direction of the curve of the needle tip. Before starting the case, this relationship should be confirmed, and the needle should be advanced into the dilator. The needle flange and sidearm of the sheath should always have the same orientation. When the needle tip is withdrawn just into the dilator tip, there is usually a space between the dilator hub and needle flange of roughly 2 cm, or 2 fingerbreadths.
Many transseptal sheaths and dilators are available. The choice depends on the clinical circumstances, the desire to have or not to have a soft tip at the end of the sheath, and the operator’s familiarity with the system. After right femoral venous access is obtained, a 0.032-inch J wire should be positioned in the superior vena cava under fluoroscopic guidance. Over the J wire, the sheath and dilator should be advanced into the superior vena cava or left innominate vein. Care must be taken to always advance the apparatus over the wire to avoid perforation.24–26 Once in the superior vena cava, the J wire is removed, and the needle and stylet are advanced within 1 cm to 2 cm of the tip of the dilator. Next, the stylet is removed and the needle is flushed. In most patients, the transseptal punctures can be performed with a standard Brockenbrough needle. In patients with an enlarged RA, the needle can be bent to increase the radius of the curve to reach the atrial septum, or a different needle type with an increased curve radius can be used (ie, BRK-1 and BRK-2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


