INDICATIONS AND
CONTRAINDICATIONS OF
TRANSSEPTAL CATHETERIZATION
MICHAEL KÜHNE, HAKAN ORAL
Transseptal catheterization describes the passage of a cardiac catheter from the right atrium through the interatrial septum into the left atrium. Unless a patent foramen ovale is present, as is the case in 20% to 25% of the population, a transseptal needle is used to create a primary puncture of the interatrial septum.1,2 The primary puncture is followed by advancing a dilator and a sheath into the left atrium, allowing access to the left atrium with the mapping or ablation catheter. If more than one catheter is used simultaneously in the left atrium, two separate punctures of the septum can be performed (“double transseptal”) or two catheters are advanced through the same primary puncture. This chapter provides an overview of the current indications and contraindications of Trans-septal catheterization in electrophysiology.
Background
The technique of accessing the left atrium via the transseptal route was first described 50 years ago.3 Previously, the left atrium was accessed using several other methods that carried considerable procedural risks, such as the suprasternal approach through the great vessels, the posterior transthoracic technique (puncture of the left atrium lateral to the spine), the transbronchial approach, and the subxiphoid approach.4,5 Transseptal catheterization has been employed to provide access to the left atrium and left ventricle since the 1960s, but with the development of coronary angiography in the late 1960s and the 1970s, the retrograde aortic approach has been more frequently used to access the left ventricle. Therefore, until recently, invasive cardiologists only rarely had sufficient experience performing transseptal catheterization unless they were trained in high-volume centers where balloon mitral valvuloplasty was performed.6 In his textbook on cardiac catheterization, William Grossman once wrote that “the infrequency with which the procedure is currently needed has made it difficult for most laboratories to maintain operator expertise and to train cardiovascular fellows in transseptal puncture, and has given the procedure an aura of danger and intrigue.”7 However, over the last few years, there has been a resurgence of transseptal catheterization due to a dramatic increase in left atrial procedures for catheter ablation.
A number of clinical scenarios exist in which it may be useful to gain access to the left atrium for diagnostic or therapeutic indications. Since the introduction of transseptal catheterization, when the technique was primarily used to measure left atrial pressure, the indications for transseptal catheterization have changed markedly over the last 5 decades. A recent study from 33 centers reported that among 5520 transseptal catheterizations for catheter ablation of arrhythmias, 78% was performed to target atrial fibrillation, and transseptal catheterization was successfully performed in 99%. The primary reason for inability to perform transseptal catheterization was abnormal anatomy of the interatrial septum.8
Indications
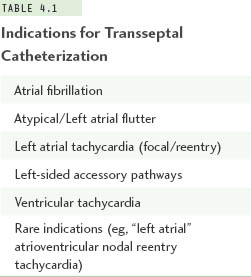
More than 10 years have passed since a landmark study described a technique targeting ectopic beats arising from the pulmonary veins to eliminate triggers for atrial fibrillation using radiofrequency catheter ablation.9 After refinements of this technique in many clinical studies in recent years, catheter ablation of atrial fibrillation has become widely available. Left atrial ablations targeting atrial fibrillation are now the most frequent indication for transseptal catheterization. However, a number of other clinical situations in the management of patients with cardiac arrhythmias require access to the left atrium, and this is most frequently achieved via the transseptal route. Table 4.1 summarizes current indications for transseptal catheterization in cardiac electrophysiology.
Atrial Fibrillation
There are different approaches to managing patients with atrial fibrillation non-pharmacologically. However, unless a patient undergoes surgical treatment of atrial fibrillation (Maze procedure) or a surgical technique such as epicardial radiofrequency ablation (AtriCure Inc, West Chester, OH),10 the arrhythmia is targeted endocardially with an ablation catheter for energy delivery, currently radiofrequency energy in most cases. Although some ablation strategies applied in the 1990s were limited to the right atrium, the significance of the left atrium and the pulmonary veins was soon recognized.11 Therefore catheter-based treatment strategies targeting atrial fibrillation all have in common that they require access to the left atrium. This is achieved by transseptal catheterization.
If more than 1 catheter is used in the left atrium at the same time, 2 separate punctures of the interatrial septum can be performed (double transseptal). Alternatively, 2 catheters can be passed through the same primary puncture of the septum. There are no specific recommendations to use single or double transseptal technique, but some operators prefer a single puncture in case the first puncture is difficult.
Repeat procedures to treat recurrences of atrial fibrillation or occurrences of other arrhythmias, such as left atrial flutters, may be necessary in some patients.12 When performing these procedures, the interatrial septum can be distorted, thickened, or fibrotic due to the development of scar tissue in the area of the previous puncture. The changes in the architecture of the interatrial septum can be quite significant in some patients, making repeat transseptal catheterization more challenging. More pressure may be required to puncture the septum due to the fibrotic changes; the typical drop of the catheter into the fossa ovalis may be more difficult to appreciate; and tenting of the interatrial septum may be absent. In these cases, intracardiac ultrasound may be particularly helpful. Data on the safety and efficacy of repeat transseptal catheterization is relatively scarce. Transseptal puncture for repeat transseptal catheterization may be necessary in some patients in whom the first left atrial procedure had been performed through a patent foramen ovale.13
When transseptal catheterization appears difficult due to fibrotic changes, novel approaches such as radiofrequency energy delivery via the transseptal needle or a dedicated radiofrequency transseptal system (Baylis Medical, Montreal, Ontario, Canada) may be indicated to successfully puncture the interatrial septum.14,15
Left Atrial Tachycardia and Flutter
Primary atrial tachycardias may be observed in approximately 10% of patients presenting with paroxysmal supraventricular tachycardia (and no previous left atrial procedures). Some of these atrial tachycardias may originate from the left atrium, and transseptal access may be necessary to map and ablate them.
Left atrial tachycardia or flutter may also develop after left atrial ablation of atrial fibrillation.16 Approximately half of these arrhythmias may be transient and not require any interventional therapy. However, in the remaining patients repeat transseptal catheterization often is necessary to eliminate these tachycardias.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


