ATRIAL SYNCHRONOUS HIS-BUNDLE PACING
Case presented by:
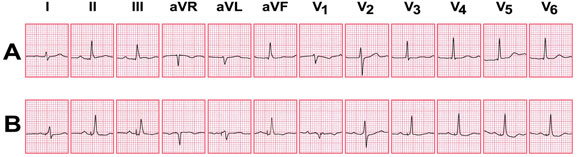
A 60-year-old patient with nonischemic cardiomyopathy (left ventricular ejection fraction [LVEF] 45%) required permanent pacemaker implantation for intermittent complete heart block. The following ECGs were recorded prior to and after pacemaker implant (Figure 65.1A and B, respectively).
Figure 65.1. ECGs recorded during sinus rhythm (A) and after pacemaker implant (B).
Question No. 1: The ECGs in Figure 65.1 demonstrate:
A.Atrial synchronous right ventricular (RV) pacing with ventricular fusion.
B.Atrial synchronous biventricular pacing.
C.Atrial synchronous direct His-bundle pacing.
D.Para-Hisian pacing.
Discussion
Biventricular pacing results in a QRS complex > 120 ms, which is distinctly different from the intrinsic (unpaced) QRS complex. Biventricular pacing can, in some cases, result in a QRS complex narrower than during intrinsic rhythm, but only when the unpaced QRS is > 120 ms and almost always in the presence of left bundle branch block (LBBB). Typically, the paced QRS shows a positive deflection in V1, reflecting capture of the left ventricle (LV), compared to a negative deflection seen in most cases of RV pacing.
Ventricular fusion occurs in the presence of intact conduction, when the programmed atrioventricular (AV) interval is similar to the intrinsic AV interval. In true ventricular fusion, the ventricular pacing stimulus lies at the beginning of the QRS complex, and the ventricles are excited simultaneously by intrinsic conduction through the His-Purkinje system as well as the ventricular pacing site. In such cases, the resulting QRS is never identical to the unpaced QRS.
On occasion, the ventricular pacing spike may be detected after the initiation of the QRS complex, as a result of it falling in the blanking period or due to sensing failure. The resultant QRS is identical to the unpaced QRS, because the ventricular stimulus has occurred when the ventricle is refractory and has not contributed to ventricular depolarization. This has been termed pseudofusion.
In the above example, the paced AV interval is shorter than the intrinsic AV interval, yet the resultant QRS is identical to intrinsic rhythm; fusion is ruled out. Since the ventricular stimulus clearly lies at the beginning of the QRS, pseudofusion is also ruled out.
Direct or selective His-bundle pacing (SHBP) is arguably the most physiological form of ventricular pacing since both ventricles are activated via the His-Purkinje system, if the His-Purkinje system is intact. RV pacing has been shown to induce electrical and mechanical dyssynchrony and is associated with worse outcomes in patients with heart failure. It should be avoided in the presence of left ventricular dysfunction. SHBP does not induce electrical dyssynchrony and may be the preferred pacing mode in patients with an intact His-Purkinje system, although this has not been assessed in randomized trials.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree