A PATIENT WITH NYHA CLASS II, WIDE QRS, AND LOW EF
Case presented by:
A 67-year-old man with anterior myocardial infarction (MI) 3 years ago is currently in NYHA class II with normal sinus rhythm (NSR), left bundle branch block (LBBB; QRS duration 164 ms) on the ECG, and an ejection fraction (EF) of 28%. The patient is receiving a beta-blocker, an ACE-inhibitor, and a low-dose diuretic.
A.Dual-chamber pacemaker.
B.Cardiac resynchronization therapy with defibrillator (CRT-D).
C.Implantable cardioverter-defibrillator (ICD).
D.Start an angiotensin II receptor blocker (ARB).
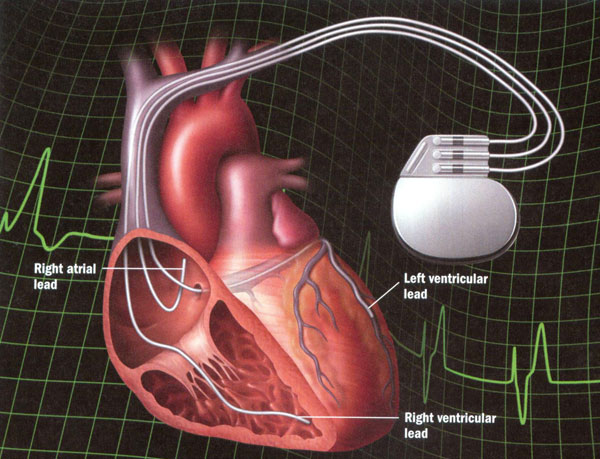
Following a significant MI, the heart undergoes adverse remodeling with cardiac enlargement and dilatation of the left ventricle with increase in the left ventricular (LV) end-diastolic pressure and reduction in the left ventricular ejection fraction (LVEF). This dysfunctional process is attenuated by beta-blocker and ACE-inhibitor therapy, but adverse remodeling may continue in some patients with the development of overt heart failure despite maximal medical management. Beginning in 2001, CRT was introduced for the treatment of patients with advanced NYHA class III/IV heart failure. With atrial synchronized biventricular pacing involving transvenous catheter electrodes in the right atrium, in the coronary vein for LV pacing, and in the right ventricular (RV) apex for nearly simultaneous RV pacing (Figure 61.1), approximately 70% of patients achieve significant improvement in LV function with increase in the LVEF and reduction in heart failure (reverse remodeling). Two major randomized trials substantiated the clinical improvement with CRT in patients with advanced heart failure, wide QRS complex, and low EF,1,2 and AHA/ACC guidelines were established for this therapy in these patients with heart failure on optimal pharmacological management.
Figure 61.1. CRT with leads positioned in the right atrium, the right ventricle, and a coronary vein that overlies the left ventricle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree