NARROW-COMPLEX TACHYCARDIA WITH FEATURES SUGGESTING MULTIPLE TACHYCARDIA MECHANISMS–THE IMPORTANCE OF ELECTROPHYSIOLOGY FUNDAMENTALS
Case presented by:
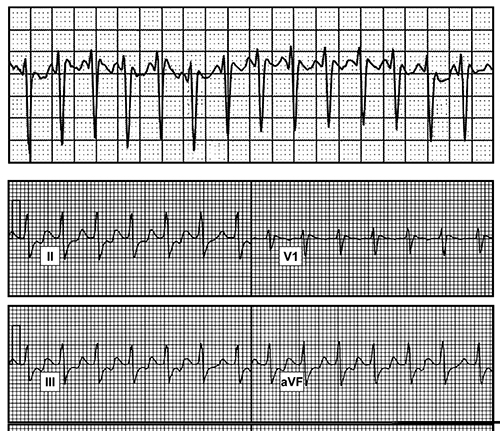
A 52-year-old woman without medical history presented with sustained palpitations provoking near-syncope. Diagnostic cardiac evaluation including electrocardiography and echocardiography were entirely normal, and event monitoring revealed narrow-complex tachycardia (Figure 6.1, top panel). Medical and interventional options were discussed and the patient opted for invasive evaluation. At electrophysiology (EP) study, the patient spontaneously developed tachycardia with similar cycle length (CL) and morphology (see Figure 6.1, bottom panel).
Figure 6.1. Top panel: Holter monitor recording showing narrow-complex tachycardia. Bottom panel: ECG recorded during EP study showing ECG leads II, III, aVF, and V1.
Question No. 1: Which of the following supraventricular tachycardia (SVT) mechanisms is likely?
A.Atrioventricular node reentry tachycardia (AVNRT).
B.Atrial tachycardia (AT).
C.Orthodromic reentry tachycardia (ORT).
D.All of the above.
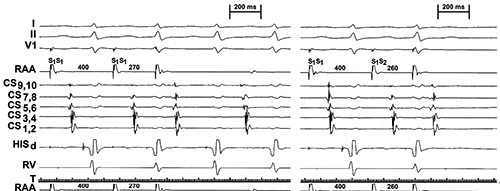
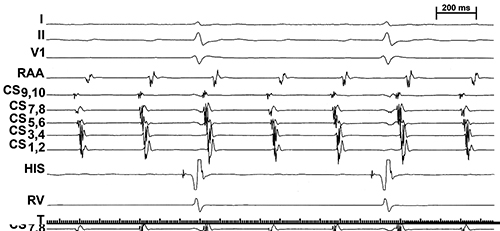
Baseline intervals included AH 150 ms and HV 55 ms at sinus CL 780 ms. During programmed atrial stimulation at a basic drive of 400 ms atrial extrastmulation at 270 ms reproducibly induced the tachycardia (first beat shown; Figure 6.2, left panel). A 10-ms decrement in the atrial extrastimulus coupling interval resulted in inability to induce the tachycardia (see Figure 6.2, right panel).
Figure 6.2. Recordings shown from top to bottom are Electrocardiographic leads I, II, V1 and right atrial appendage (RAA), coronary sinus (CS) proximal to distal, distal His Bundle (HISd), and right ventricle (RV).
Question No. 2: Which of the following tachycardia mechanisms is least likely?
A.Atrioventricular (AV) node reentry.
B.Atrial tachycardia.
C.Orthodromic reentry tachycardia.
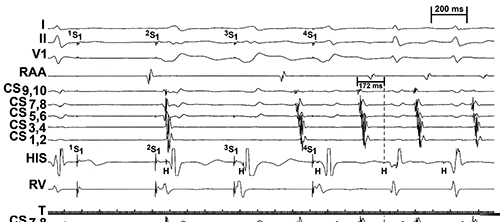
Fixed CL ventricular pacing during EP study is depicted in Figure 6.3.
Figure 6.3. Fixed CL ventricular pacing. Tracings are similar to Figure 6.2.
Question No. 3: What can be inferred about the general tachycardia mechanism?
A.Retrograde conduction is critical to the tachycardia initiation.
B.Tachycardia is spontaneously induced during sinus rhythm and is independent of V pacing.
C.AT is eliminated as a mechanism of tachycardia.
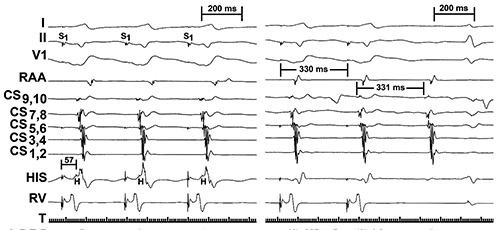
During sinus rhythm, long ventricular pacing drives (pacing cycle length [PCL] 320 ms) were required to demonstrate 1:1 retrograde conduction (Figure 6.4, left panel); the tachycardia exhibited slight variability in CL, though with fixed mechanism–ventricular overdrive pacing at 330 ms (tachycardia cycle length [TCL] 354 ms) is shown (see Figure 6.4, right panel).
Figure 6.4. Ventricular pacing at cycle l (left panel) and ventricular overdrive pacing during tachycardia (right panel). Tracings are similar to Figure 6.2.
Question No. 4: What do the results of overdrive pacing demonstrate?
A.AT is the likely mechanism.
B.Entrainment response suggests AV node dependent tachycardia as the mechanism.
C.Overdrive pacing fails to entrain the tachycardia.
During sustained tachycardia the phenomenon in Figure 6.5 was observed.
Figure 6.5. Advanced heart block during tachycardia. Tracings similar to Figure 6.2.
Question No. 5: Which mechanism of tachycardia is ruled out?
A.Atrial tachycardia.
B.Orthodromic reentry tachycardia.
C.Atrioventricular node reentry.
Discussion
The case presented illustrates several fundamental electrophysiologic properties that must be recognized in order to properly diagnose SVT.
One of the most critical pieces of information is a clinical recording of the arrhythmia (see Figure 6.1, upper panel). The Holter monitor demonstrates a narrow-complex tachycardia with unclear P-wave morphology, but the arrhythmia induced at EP study was of similar CL and the P waves were more easily discernable now with 12 leads available for scrutiny (see Figure 6.1, lower panel–ECG leads II, III, aVF, and V1 shown). The narrow QRS preceded by a His potential diagnoses supraventricular origin, and the P waves can be seen to have an inverted morphology in leads II, III, and aVF
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree