CARDIAC RESYNCHRONIZATION THERAPY
Case presented by:
A 77-year-old African-American male with history of diabetes mellitus, gout, hypertension, and mild chronic renal insufficiency was diagnosed with dilated cardiomyopathy in March 2002. His echocardiogram revealed left ventricular (LV) ejection fraction (EF) of 10% to 15%, LV end-diastolic dimension (LVEDD) of 80 mm, and LV end-systolic dimension (LVESD) of 73 mm. He had several heart failure (HF) admissions in the ensuing months and remained in New York Heart Association (NYHA) class III despite optimal medical therapy (OPT). In July 2002, he received a biventricular pacemaker due to the presence of left bundle branch block (LBBB) with a QRS duration of 190 ms. Over the following weeks, he improved symptomatically to NYHA class II. A repeat echocardiogram the following year demonstrated improvement of his LVEF and dimensions (LVEF 20%, LVEDD 56 mm, LVESD 51 mm). His most recent echocardiograms (in 2005 and 2009) demonstrated gradual improvement of his LVEF to 35% and 55%, respectively (LVEDD 51 mm, LVESD 38 mm). He has been clinically stable over the past 8 years and has not had any HF admissions over the past 3 years.
Question No. 1: Which of the following is true?
A.Cardiomyopathy and HF are associated with ventricular conduction delay.
B.Delayed electrical activation of left ventricle (LV) leads to abnormal pump efficiency.
C.Cardiac resynchronization therapy (CRT) can correct mechanical dyssynchrony in many patients.
D.All of the above are true.
Discussion
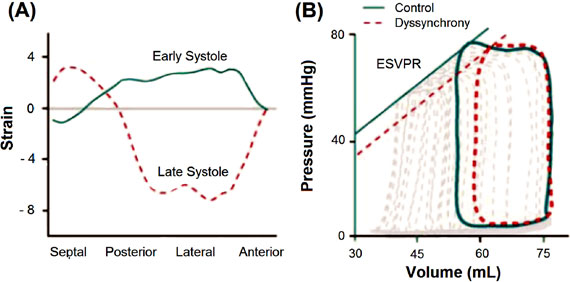
Cardiomyopathy and HF have been commonly associated with ventricular conduction delays such as LBBB. LBBB typically results in regionally delayed electrical activation in the posterolateral LV wall. The early activation of the septum results in early systolic contraction that is unopposed due to the lack of simultaneous contraction of the LV free wall. Therefore, the lateral wall stretches in response to septal contraction, delaying the rise of LV pressure. Similarly, the lateral wall is activated (in late-systole) and reaches its peak force when the septum is relaxed (stretching this region), which could occur even after aortic valve closure (Figure 57.1A). Therefore, this delayed electrical activation of the LV results in abnormal myocardial shortening and pump efficiency,1–3 which has led to the term mechanical dyssynchrony. LV dyssynchrony decreases cardiac output as this shifts the end-systolic pressure-volume relationship to the right, decreasing stroke volume and increasing LV end-systolic volume and wall stress (see Figure 57.1B).1,3 Biventricular pacemakers or CRT were developed to correct LV mechanical dyssynchrony found in many patients with HF and ventricular conduction delays, principally LBBB. Over the past decade more than 9000 patients have been studied as part of randomized clinical trials, which have demonstrated the benefits of CRT (Table 57.1).4
Figure 57.1. A: Plot of instantaneous circumferential strain at different regions across a short-axis section of the mid-LV in a dyssynchronous heart during early (solid line) and late (dashed line) systole.3 This illustrates that septal wall strain increases while the posterior and lateral strain stretches in early systole. In contrast, the posterolateral wall strain increases, resulting in septal stretch in late-systole. (Reproduced from Park et al with permission.1) B: LV pressure-volume loops in dyssynchrony.1 LV dyssynchrony decreases net cardiac output as the end-systolic pressure-volume relationship shifts to the right, with a reduction of stroke volume (loop width) and increase in end-systolic volume. (Reproduced from Byrne et al with permission.3)
The Multicenter InSync Randomized Clinical Evaluation (MIRACLE) trial5 was one of the first landmark studies to demonstrate the clinical benefits of CRT in NYHA class III and IV HF. This trial demonstrated that CRT increased LVEF (+4.6% vs –0.2%, p < 0.001) and reduced QRS duration (–20 ms, p < 0.001), LVEDD (–3.5 mm, p < 0.001) and area of mitral regurgitation (–2.7 cm2, p < 0.001) when compared to OPT. Consequently, functional capacity and quality of life (QOL) improved significantly in the majority of subjects. Furthermore, death or hospitalization for HF was significantly reduced with CRT alone (24.4% vs 15.7%, p = 0.02). Our patient received a CRT pacemaker (CRT-P) in 2002 based on the results of this trial and because the benefits of CRT with an implantable cardioverter-defibrillator (ICD) in NYHA class III and IV patients were unproven at that time.
The following year, the MIRACLE-ICD trial6 compared for the first time ICD alone versus CRT plus ICD (CRT-D) in high-risk subjects for sudden cardiac death, LVEF < 35%, QRS > 130 ms and NYHA class III and IV HF. This trial demonstrated that CRT-D significantly improved QOL and functional class, peak oxygen consumption by 1.1 mL/kg/min (p = 0.04), and increased treadmill exercise duration by 56 seconds (p < 0.001) when compared to ICD alone. Interestingly, no difference was found in 6-minute walk distance, LV size or function, HF status, survival, or hospitalization. However, this trial had the smallest population size (see Table 57.1) and most likely was underpowered to find statistical difference in these variables.
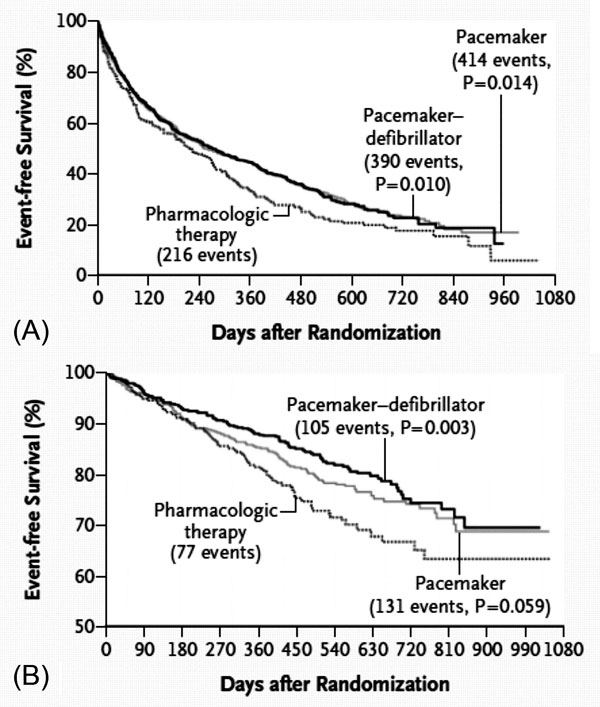
In 2004, the Comparison of Medical Therapy, Pacing and Defibrillation in HF (COMPANION) study7 compared the outcomes between medical therapy, CRT-P and CRT-D in more than 1500 patients with ischemic and nonischemic cardiomyopathy class III or IV HF, LVEF < 35% and ventricular conduction delay (QRS > 120 ms). This study demonstrated that both CRT-P and CRT-D reduced the composite of death or hospitalization for any cause by 20% (primary end point, hazard ratios (HRs) 0.81 and 0.80, p = 0.014 and p = 0.01, respectively), decreased the risk of death from or hospitalization for HF by 34% in CRT-P and 40% in CRT-D group (combined end point, p < 0.002 and p = 0.001, respectively) and reduced death from any cause (secondary end point) by 24% in CRT-P (p = 0.059) and by 36% in CRT-D group (p = 0.003) when compared to OPT (Figure 57.2). The trial was terminated prematurely due to the large clinical benefits from CRT-P and CRT-D. Subgroup analysis demonstrated that QRS > 148 ms predicted benefit for all end points. Similarly to MIRACLE,5 the COMPANION trial confirmed improvement in NYHA class, QOL and 6-minute walk distance compared to OPT.
Figure 57.2. Kaplan–Meier estimates of primary (A) and secondary end points (B) at 3 years from COMPANION study.7 Primary end point includes death from or hospitalization for any cause. Secondary end point includes death from any causes. (Reproduced from Bristow et al with permission.7)
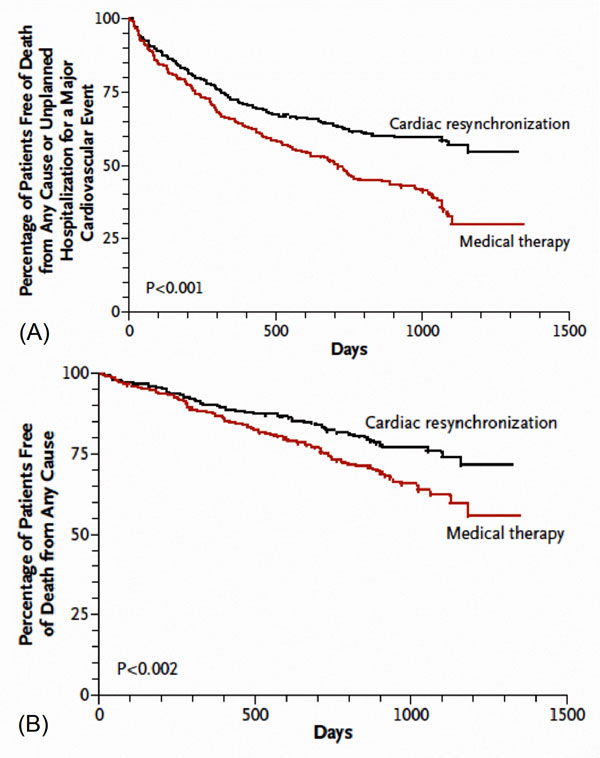
The Cardiac Resynchronization in Heart Failure (CARE-HF) study8 compared CRT-P versus OPT in patients with HF class III and IV, LVEF < 35% and QRS > 120 ms. This was the first trial that required LV dyssynchrony as inclusion criteria for QRS duration between 120 and 149 ms. Death from any cause or hospitalization for a cardiovascular event (primary end point) significantly favored the CRT-P group (39% vs 55%, HR 0.63; p < 0.001) (Figure 57.3). Furthermore, CRT-P decreased pro-B-type natriuretic peptide by 1122 pg/ml (confidence interval [CI] –1815 to –429, p < 0.002), interventricular mechanical delay by 21 ms, LV end-systolic volume index by 26 ml/m2 (CI –3.15 to –20.4, p < 0.001) and area of mitral regurgitation by 0.042 cm2 (CI –0.070 to –0.014, p = 0.003), whereas it increased LVEF by 6.9% (CI 5.6 to 8.1, p < 0.001) and improved NYHA class HF (2.7 ± 0.9 vs 2.1 ± 1, p < 0.001) and QOL. Importantly, only 7% of the CRT-P group (29 out of 402 subjects) had sudden cardiac death, which could have been presumably prevented by the addition of a defibrillator.
Figure 57.3. Kaplan–Meier estimates of the time to the primary end point (A) and secondary end point (B) in CRT from CARE-HF trial.8 Primary end point includes death from any cause or unplanned hospitalization for a major cardiovascular event. Secondary end point consists of death from any cause. (Reproduced from Cleland et al with permission.8)
A meta-analysis of CRT trials9 with more than 9000 patients showed that biventricular pacing in appropriately selected patients results in an average 3% increase in LVEF and increase in NYHA functional class by 1, while it decreased hospitalization and all-cause mortality by 37% and 22%, respectively.
Most recently, the REVERSE10 and MADIT-CRT11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree