T-WAVE OVERSENSING AND IMPLANTABLE CARDIOVERTER-DEFIBRILLATOR SHOCKS
Case presented by:
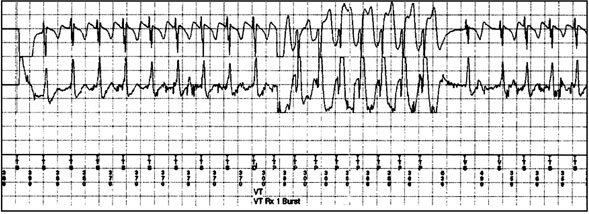
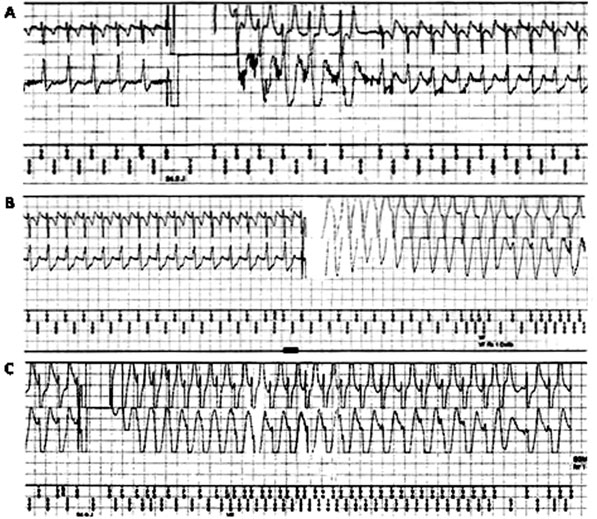
A 65-year-old male was diagnosed to have dilated cardiomyopathy in 2000. He had presented with a history of syncope at the time of diagnosis. Coronary angiography had revealed normal coronaries. He had also undergone electrophysiology study in which ventricular tachycardia (VT) was induced; however, details of the procedure were not available. Subsequently, he had undergone single-chamber implantable cardioverter-defibrillator (ICD) implantation in 2000. The defibrillation test and R-wave details at the time of initial implant were not available. We saw him in 2008 when the generator had reached near-end of service. He was NYHA class II on an optimal dose of beta-blockers and angiotensin-converting enzyme (ACE) inhibitors. A repeat echocardiogram revealed left ventricular ejection fraction of 26%. He underwent ICD replacement (Entrust D154VRC, Medtronic Inc., Minneapolis, MN, USA). The previous lead (Medtronic Sprint 6942, a 65-cm, passive fixation, integrated, bipolar dual-coil lead) was retained. The R wave at the time of ICD replacement was 5 mV. Pacing and shock impedance were within normal range. Sensitivity was kept at the nominal 0.3 mV. Detection was programmed to 2 zones—VT cut-off was 150 bpm and ventricular fibrillation (VF) cut-off was 188 bpm. Antitachycardia pacing (ATP) during charging was programmed “on,” thereby meaning one burst of ATP therapy would be delivered during charging for therapy in the VF zone (if cycle length is < 240 ms). Wavelet was programmed to “monitor,” meaning the device will classify each beat in the tachycardia zone as supraventricular or ventricular but will not play a role in the delivery of therapy. The supraventricular tachycardia (SVT) limit was kept at 320 ms. In mid-2009, he received a cluster of shocks while bicycling furiously. He did not have presyncope/syncope symptoms at that time. Figure 56.1 shows the initial electrograms (EGM) when the device detected tachycardia and the first sequence of ATP was delivered; Figure 56.2 shows the EGMs after the first shock (Figure 56.2A), the second shock (Figure 56.2B), and the final shock (Figure 56.2C).
Question No. 1: Was the therapy appropriate?
Question No. 2: What happened after the second shock?
Question No. 3: What are the measures that can be taken?
Question No. 4: What type of internal and external noise can cause inappropriate shock?
Figure 56.1. From top to bottom: Near-field EGM, far-field EGM, and marker channel. The initial part shows tachycardia at a cycle length of 370 ms. The wavelet suggested SVT. The far-field EGM was similar to the far-field EGM at the time of interrogation. Since the VT/SVT enhancements were not programmed “on,” the device interpreted the rhythm as VT (wavelet was programmed to “monitor”).
Figure 56.2. From top to bottom in each panel: Near-field EGM, far-field EGM, and marker channel. A: The initial EGM distortion quickly decreases with only mild broadening of EGM after the initial few beats. There is no oversensing of T wave. Sinus tachycardia, probably perpetuated by the shock, persists at the same cycle length of 370 ms. B: The distortion of the EGM is gross with T-wave oversensing. The distortion is so much that the EGM saturates the channel. Sinus tachycardia persists. C: The distortion of the EGM is even greater.
T-wave oversensing can lead to inappropriate shocks. T waves are identified by the device as R waves and delivery of shock on T waves can induce VF. If this happens on the last shock, the consequences can be serious and can result in mortality.12 Appropriate use of enhancements for better SVT/VT discrimination and ATP therapy can reduce the number of inappropriate and appropriate shocks and also reduce the risk for post-shock T-wave oversensing.
The size of the T wave relative to the R wave influences the choice of remedy. The presence of a good-sized R wave with a good R-to-T-wave ratio suggests that T-wave oversensing will be amenable to several measures like alteration of sensitivity, threshold start, and delay decay. However, a small R wave would indicate that insertion of a separate pace/sense lead would be required to solve the problem of T-wave oversensing. The lead and device implanted may also influence the remedy. In this case, the presence of an integrated bipolar lead was probably responsible for the distortion of EGMs post shock.
Correct Answers
1. Was the therapy appropriate?
Answer: The patient was cycling at the time of receiving shocks. He did not have any symptoms of presyncope. He received a cluster of shocks. All these features suggest that the therapy may have been inappropriate. Moreover, the far-field EGM during the initial detection had a good wavelet match score and was similar on manual analysis to the far-field EGM recorded at the time of interrogation. The interval plot suggested that there was a gradual increase in heart rate prior to detection. These features suggest that the patient received the initial ATP therapies for sinus tachycardia.
2. What happened after the second shock?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree