ANOMALOUS CORONARY ARTERY AND VENTRICULAR ARRHYTHMIAS
Case presented by:
A 13-year-old male suddenly collapsed while running quarter-mile sprints in gym class at school and rapidly became pulseless and apneic. Cardiopulmonary resuscitation (CPR) was initiated at the scene and 911 was called. Emergency medical personnel arrived and identified ventricular fibrillation (VF) (Figure 48.1), which responded to epinephrine, atropine, and external defibrillation with return of spontaneous circulation and sinus rhythm. He was intubated in the field and transported to a local emergency department for stabilization.
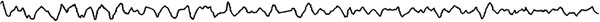
Figure 48.1 ECG demonstrating patient’s VF.
A.Aortic valve stenosis.
B.Coarctation of the aorta.
C.Congenital coronary artery abnormalities.
D.Ventricular septal defect with pulmonary vascular disease.
The patient was started on dopamine for blood pressure support, and his first 12-lead ECG demonstrated probable sinus tachycardia with wide-complex QRS diagnosed as right bundle branch block (RBBB) (Figure 48.2).
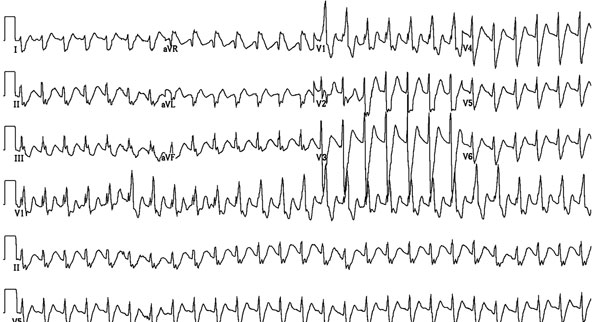
Figure 48.2 Probable sinus tachycardia with wide-complex QRS.
He was transported to a children’s medical center for further evaluation and, during transport, developed nonsustained ventricular tachycardia (VT) initially responsive to a lidocaine infusion. Transthoracic echocardiography showed significant global left ventricular (LV) hypokinesis (ejection fraction 30%) and an anomalous left coronary artery. From a short-axis view, two-dimensional imaging identified anomalous aortic origin of the left coronary artery from the right sinus of Valsalva (Figure 48.3) with an interarterial course between the aorta and the pulmonary artery (PA). The initial course of the anomalous coronary was intramural within the anterior aortic wall.
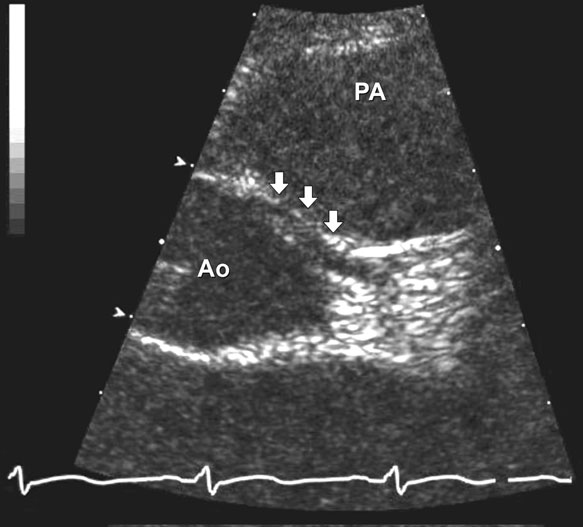
The intramural anomalous coronary course is frequently best appreciated by color Doppler and was clearly seen in this patient using this technique (Figure 48.4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


