AN ECG OF EARLY REPOLARIZATION
Case presented by:
A 39-year-old gentleman presented with 3 noctural episodes of syncope and resuscitated cardiac arrest due to documented ventricular fibrillation (VF). He received multiple external defibrillations for recurrent VF unresponsive to antiarrhythmic drugs early during hospitalization. Coronary angiography and echocardiography were normal. Baseline PR interval and QTc were normal. No electrocardiographic (ECG) signs of Brugada syndrome were present at baseline and post flecainide challenge. Diagnostic electrophysiology (EP) study was normal for baseline intervals without inducible ventricular arrhythmias.

Figure 44.1 Baseline 12-lead ECG.
Question No. 1: The ECG is suggestive of
A.Short QT Syndrome.
B.Isoproterenol will be helpful in controlling VF episodes.
C.None of the above.
Discussion
The baseline ECG showed >0.1mV J-point elevation with terminal QRS notch/slur in the inferior leads suggestive of abnormal early repolarization (ER) pattern (Figure 44.2).
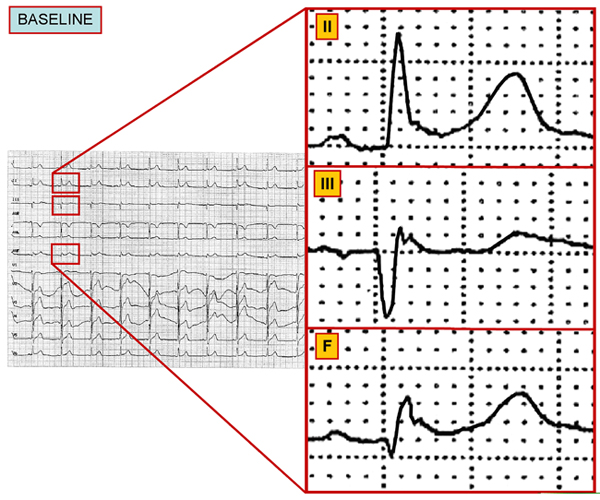
Figure 44.2 Baseline ECG highlighting the leads with slur and notch.
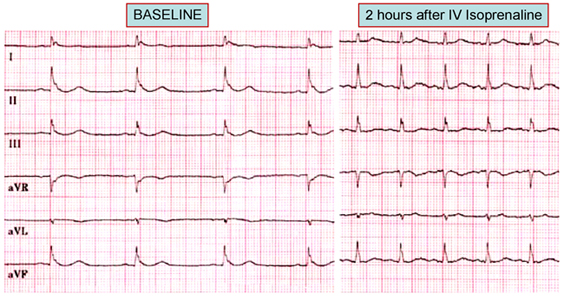
Early in-hospital course was turbulent with recurrent uncontrollable VF. A continuous isoproterenol infusion was initiated and found to be effective in controlling recurrent VF. The abnormal ER pattern on the 12-lead ECG subsided.
Several drugs have been tested in VF storm. Isoprenaline has been the most effective in controlling VF storm (Figure 44.3). The infusion of isoproterenol can successfully manage electrical storms (>2 VF episodes per 24 hours), and can sometimes be used as a life-saving therapy. Sedation, parenteral amiodarone, and quinidine have also been effectively used. The arrhythmogenicity of ER syndrome is thought to be related to heterogeneity of action potentials (spike-and-dome morphology in epicardial tissue) across the ventricular wall at the end of phase 1. Any perturbation in the balance of currents may amplify the disparity in voltage gradient and precipitate local reentries and polymorphic ventricular arrhythmias, providing both the trigger and substrate of VF. Disappearance of abnormal ER and normalization of ECG following isoproterenol infusion is thought to be secondary to increase in ICa-L current, thereby decreasing electrical gradient and homogenizing action potential durations and, possibly, increasing the heart rate.1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


