SHORT QT SYNDROME
Case presented by:
A 35-year-old white man presented to the emergency department with an episode of syncope during exertion. He was previously healthy except for an episode of paroxysmal atrial fibrillation (AF) at the age of 25. He denied syncope prior to this episode but had frequent palpitations lasting for several minutes attributed to episodes of paroxysmal AF. He was not on any medications and his family history is significant for a brother who died suddenly at age of 3 months and father who died at age 39 due to sudden cardiac death (SCD). Autopsy of the father did not reveal any structural heart disease. His ECG is shown in Figure 41.1. He was admitted to the hospital for further workup and monitored on telemetry. He had frequent premature ventricular complexes (PVCs) on telemetry monitor and a couple of short-lived episodes of self-terminating polymorphic ventricular tachycardia (VT).
Question No. 1: What is the diagnosis?
A.Catecholaminergic polymorphic VT.
B.Idiopathic ventricular fibrillation (VF)—J wave syndrome.
C.Hyperkalemia.
D.Short QT syndrome (SQTS).
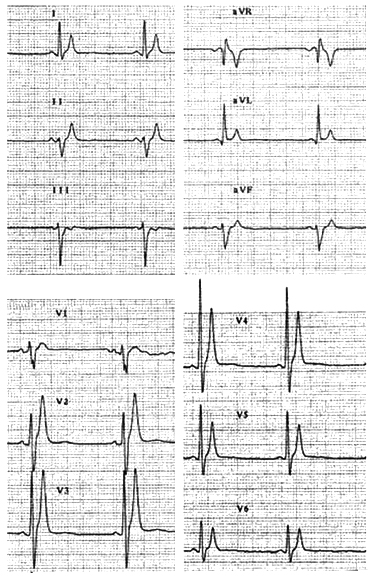
Figure 41.1 ECG of SQTS Proband. HR 52 bpm, QT 280 ms.
Further workup including Echocardiographic stress test did not reveal any evidence of structural heart disease. Results of signal-averaged ECG, heart rate (HR) variability and QT dispersion were within normal limits. Patient did not have any electrolyte abnormalities to explain persistently short QT interval. During stress testing, the QT interval abbreviated but failed to prolong to normal values upon recovery.
ECG obtained as a screening of family members revealed that the patient’s 31-year-old sister and her 6-year-old son had similar ECG pattern showing extremely short QT intervals. The 6-year-old had an episode of aborted SCD at age 8 months.
On electrophysiologic study of the proband, both AF and VF were readily inducible using programmed atrial or ventricular stimulation. An implantable cardioverter-defibrillator (ICD) was implanted and the patient experienced 2 appropriate shocks during the first year of follow-up.
Question No. 2: What QT interval on ECG will qualify as short QT interval?
A.400 ms at HR of 60 bpm.
B.360 ms at HR of 90 bpm.
C.300 ms at HR of 120 bpm.
D.280 ms at HR of 53 bpm.
Question No. 3: The SQTS is characterized by
A.Tall peaked T waves.
B.Gain of function mutations in potassium channel genes.
C.Loss of function mutations in calcium channel genes.
D.All of the above.
Question No. 4: What is the cellular basis for development of arrhythmias in the SQT1 form of SQTS?
A.An increase in transmural dispersion of repolarization (TDR).
B.An increase in IKr.
C.A decrease in effective refractory period (ERP).
D.None of the above.
E.All of the above.
Question No. 5: What drug is generally effective in prolonging the QT interval in SQT1 patients?
A.Quinidine.
B.Dofetilide.
C.Amiodarone.
D.Sotalol.
Discussion
Short QT syndrome
The SQTS is an inherited syndrome characterized by a QTc ≤360 ms and high incidence of VT/VF in infants, children and young adults. It is a genetically heterogeneous disease, and thus far, mutations of 6 different genes encoding cardiac ion channels have been identified in familial or sporadic cases. Gain-of-function mutations in KCNH2, KCNQ1, and KCNJ2 genes encoding for the rapidly and slowly activating potassium channel currents (IKr and IKs) and the inward rectifier potassium channel current (IK1) give rise to the SQT1, SQT2, and SQT3 forms of SQTS. Loss of function mutations in CACNA1c, CACNB2b, and CACNA2D1 genes encoding the α1, β, and α2δ subunits of cardiac L-type calcium channels is also responsible for SQTS. These clinical phenotypes, characterized by a clinical entity consisting of a combined Brugada-like ST-segment elevation and short QT intervals, have been designated SQT4, SQT5, and SQT6. In addition to an abbreviated QT interval, SQTS is characterized by the appearance of tall peaked and often symmetrical T waves in the ECG. The augmented Tpeak-Tend interval associated with this electrocardiographic feature of the syndrome suggests that TDR is significantly increased.
Studies employing the left ventricular wedge model of the SQTS have provided evidence in support of the hypothesis that an increase in outward repolarizing current can preferentially abbreviate the epicardial action potential, thus increasing TDR and creating the substrate for reentry.1 In addition to this augmented spatial dispersion of repolarization, arrhythmogenesis in SQTS is facilitated by the abbreviated ERP.
Diagnosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


