LQTS
Case presented by:
M.T. is a sibling of a patient who has been recently diagnosed with long QT syndrome (LQTS) following an episode of syncope during swimming. M.T. is a 16-year-old male and has not experienced any episodes of syncope in the past. His corrected QT interval (QTc) is within the normal range (420–440 ms on 3 consecutive ECGs). However, genetic testing reveals that he is a carrier of his brother’s LQTS-causing (S349W) mutation, which is located in the transmembrane region of the KCNQ1 (LQT1) channel.
Question No. 1: What therapy would you recommend to M.T. in light of the genetic diagnosis?
A.Avoid intense physical activity and QT-prolonging drugs and careful follow-up without medical therapy.
B.Beta-blocker therapy.
C.Left cardiac sympathetic innervations (LSCD).
D.Implantable cardioverter-defibrillator (ICD).
The hereditary LQTS is a familial disorder in which most affected family members have delayed ventricular repolarization manifest on the ECG as QT prolongation. This genetic channelopathy has variable penetrance with affected individuals having an increased propensity to syncope, polymorphous ventricular tachycardia (torsades de pointes), and sudden arrhythmic death. The estimated overt prevalence of this disorder is in the range of about 1:5,000 subjects. However, the prevalence of LQTS patients with overt or subclinical disorders is likely to be considerably greater than the currently estimated prevalence.1
Clinically, LQTS is identified by abnormal QT interval prolongation on the ECG. The QT prolongation may arise from either a decrease in repolarizing potassium currents or an inappropriate late entry of sodium into the myocyte. Most commonly, QT prolongation is produced by delayed repolarization due to mutations in the α-subunit of ion channels involving either the slowly (IKs; KCNQ1; LQT1) or rapidly (IKr; KCNH2; LQT2) acting repolarizing cardiac potassium currents.1 Mutations of the sodium-channel protein are less frequent and are associated with prolonged depolarization due to a small persistent inward “leak” in cardiac sodium (Na+) current INa (SCN5A; LQT3). To date, more than 600 mutations have been identified in 13 different LQTS genes, with the LQT1–3 making up approximately 95% of identified genotyped cases.1
Genotype–phenotype studies of LQTS have provided new insights into risk mechanisms, the electrocardiographic features, and the long-term clinical course associated with this inherited disorder. For example, each of the 3 major genotypes (LQT 1–3) has a distinctive T-wave repolarization pattern on the ECG. These include typical broad-based T waves in LQT1 patients, bifid T waves in LQT2 patients, and late-onset peaked T waves in LQT3 patients (Figure 40.1).
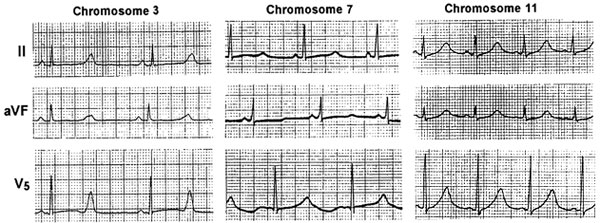
Figure 40.1 T-wave morphology by LQTS genotype: LQT1—right panel (QTc = 570 ms); LQT2—middle panel (QTc = 583 ms); and LQT3—left panel (QTc = 573 ms). (Reprinted with permission.1)
The diagnosis of LQTS relies mainly on ECG findings and clinical history. An accurate measurement of the QT interval is essential for the diagnosis of LQTS. The QT interval should be determined as a mean value derived from at least 3 to 5 cardiac cycles (heart beats), and is measured from the beginning of the earliest onset of the QRS complex to the end of the T wave. The QT interval is usually corrected for heart rate using Bazett’s formula (QTc = QT/RR0.5 with all intervals in seconds), which remains the standard for clinical use. In general, QTc is considered as prolonged if >450 ms and >470 ms in adult men and women, respectively.1 When marked QTc prolongation is present, the diagnosis is straightforward. For less clear cases, a scoring system has been introduced that takes into account ECG findings, prior symptoms, and family history.1
Genetic testing for LQTS has recently emerged as an additional important diagnostic and clinical tool. It should be noted that currently a genetic test can be expected to capture approximately three-fourth of phenotypically affected LQTS individuals, whereas a negative genetic test in a subject with clinical LQTS (ie, genotype negative/phenotype positive LQTS) provides no basis for removing the diagnosis.1 However, a positive genetic test may influence treatment decisions and may identify relatives with concealed LQTS, since approximately 25% of individuals with genetically proven LQTS have a nondiagnostic QTc.1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


