INTERFASCICULAR REENTRANT VENTRICULAR TACHYCARDIA
Case presented by:
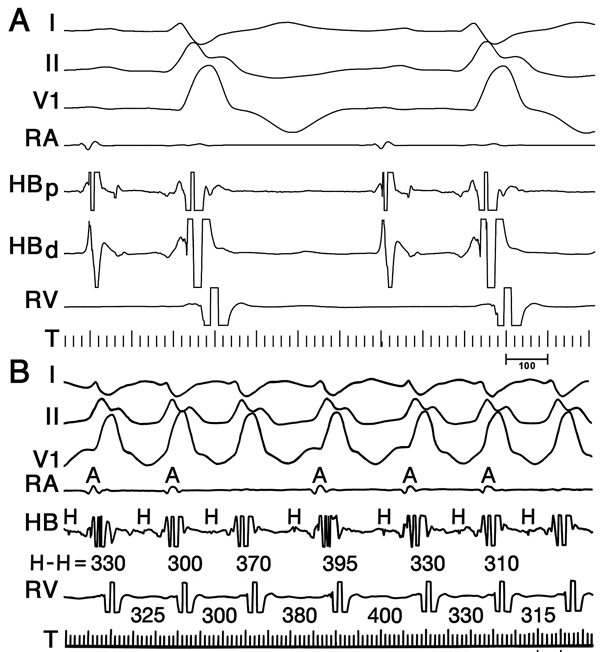
A 72-year-old woman with an ischemic cardiomyopathy (left ventricular ejection fraction (LVEF) 15%) received multiple implantable defibrillator shocks for sustained monomorphic ventricular tachycardia (VT) despite amiodarone therapy. Electrophysiologic studies revealed an HV interval of 70 ms during sinus rhythm and inducible bundle branch reentry (BBR) VT with a left bundle branch block (LBBB) pattern (cycle length 330 ms). Immediately after successful right bundle branch (RBB) ablation, multiple runs of nonsustained tachycardia occurred during sinus rhythm (ie, right bundle branch block [RBBB] with rightward axis, Figure 39.1). A His-bundle potential preceded each QRS complex, and the HV interval, which prolonged to 120 ms after the RBB ablation, shortened to 70 ms during the VT (Figures 39.1 and 39.2). Changes in HH intervals preceded and dictated subsequent VV intervals (see Figure 39.2).
Question No. 1: What is the mechanism of this tachycardia?
A.Monomorphic “scar-related” VT.
B.Atrioventricular nodal reentrant tachycardia (AVNRT) with AV dissociation.
C.Atriofascicular reentrant tachycardia.
D.Interfascicular reentrant VT.
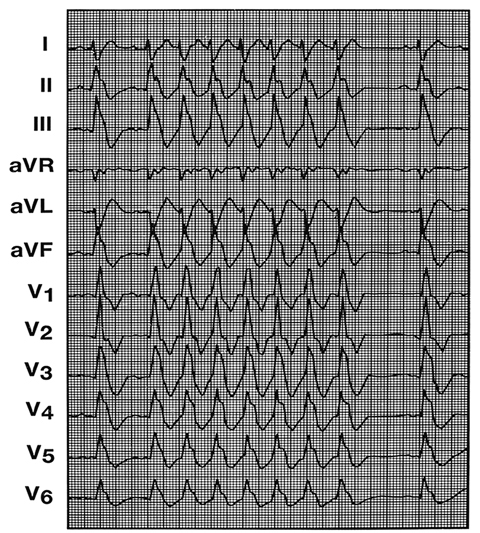
Figure 39.1. 12-lead ECG showing an identical QRS morphology during sinus rhythm (first and last beats) and during spontaneous, nonsustained interfascicular reentry after the RBB ablation. The QRS exhibits an RBBB and rightward axis, so the (left) ventricle is activated by way of the left anterior fascicle during sinus rhythm and during tachycardia. (Reproduced from Blanck et al1 with permission from John Wiley and Sons.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


