MAGNETIC RESONANCE IMAGING IN VENTRICULAR TACHYCARDIA
Case presented by:
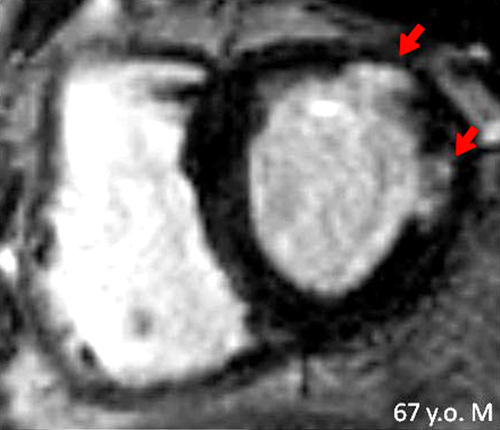
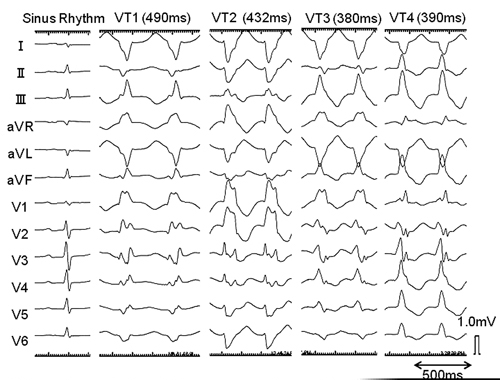
A 67-year-old man with history of coronary artery disease and normal ejection fraction (EF, 55%) post-coronary artery bypass graft surgery presented with recurrent episodes of sustained monomorphic ventricular tachycardia (VT) at a rate of 120 bpm. He complained of palpitations, but had no dizziness or syncope. After failure of multiple antiarrhythmic agents including amiodarone, the patient was referred for catheter ablation. Cardiac magnetic resonance imaging (CMR) was performed prior to VT ablation. Late gadolinium-enhanced (LGE) CMR demonstrated anterolateral scar in the left ventricle (LV) (Figure 37.1). During electrophysiology (EP) study, 4 distinct VT morphologies including the clinical VT (VT1) were easily inducible with programmed ventricular stimulation from the right ventricular apex (RVA, Figure 37.2). All VT morphologies were terminable by overdrive pacing.
A.All induced VTs (VT1–4) are scar-related and their exit sites are likely to be identified epicardially.
B.All induced VTs (VT1–4) are scar-related and their exit sites are likely to be identified endocardially.
C.All induced VTs except VT4 are scar-related and the exit sites of VT1, VT2, and VT3 are likely to be identified endocardially.
D.None of the induced VTs are scar-related and the exit site locations of the induced VTs are not predictable without mapping.
Discussion
All VTs were reproducibly induced by single- or double-extra stimulations from the RVA, and all were terminable by overdrive pacing. Additionally, the patient has history of remote myocardial infarction. These findings strongly suggest that the mechanism underlying all of the induced VTs is reentry. 12-lead ECG demonstrated 4 different wide QRS complex tachycardias with right bundle branch block, negative R wave in leads I and aVL, and rS pattern in lead II, except VT3, which demonstrated a positive R wave in the inferior leads. The QRS morphologies of these VTs are consistent with exit sites in the anterolateral myocardial region in the LV.1 This is consistent with the scar location on LGE-CMR (see Figure 37.1). Berruezo et al2 described ECG characteristics suggestive of VTs with epicardial exit sites. Epicardial VTs generally exhibit a pseudo-delta wave and long intrinsicoid deflection time. These ECG characteristics are likely due to the intramyocardial conduction delay from the epicardium to the endocardium. The ECG characteristics of the 4 induced VT morphologies in our patient do not meet the criteria that typically identify epicardial VTs. Endocardial scar location on LGE-CMR with ≤ 75% of scar transmurality (with respect to full wall thickness) also supports an endocardial exit site.
A.Concealed entrainment during tachycardia.
B.Postpacing interval (PPI) similar to VT cycle length (CL).
C.Perfect pace map or good pace map during sinus rhythm.
D.Scar size and location on LGE-CMR.
Discussion
The significance of fractionated and isolated delayed potentials as characteristic electrograms (EGMs) often observed in critical sites for scar-related VT has been demonstrated.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


