IDIOPATHIC LEFT VENTRICULAR TACHYCARDIA
Case presented by:
A 51-year-old woman admitted for palpitations was found to have a wide-complex tachycardia (Figure 33 B.1). Sinus rhythm was restored medically and diagnostic cardiac workup included repeat ECG, serial cardiac enzymes, echocardiogram, and cardiac catheterization, all of which were normal.
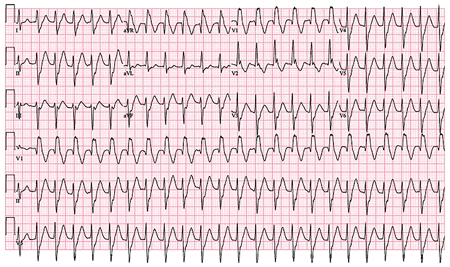
Figure 33 B.1. Patient’s ECG at presentation.
Question No. 1: The ECG in Figure 33 B.1 shows:
A.Supraventricular tachycardia (SVT) with right bundle branch block (RBBB) aberrant conduction.
B.Idiopathic left ventricular (LV) tachycardia.
C.Antidromic tachycardia involving a left-sided accessory pathway.
D.Bundle branch reentry.
Medical therapy effectively suppressed her tachycardia until a recurrence 1 year later that necessitated repeat hospitalization for severe palpitations and light-headedness. Invasive electrophysiology (EP) study and radiofrequency ablation were recommended. Baseline measurements in sinus rhythm included AH 89 ms and HV 55 ms, but tachycardia was not inducible.
A.If dual atrioventricular (AV) node physiology and/or single AV nodal echoes are seen, AV node reentry is the tachycardia mechanism.
B.Ventricular pacing to identify the retrograde activation sequence will identify the tachycardia mechanism.
C.A multipolar catheter positioned along the posterior septum or catheter mapping in that region can suggest the diagnosis.
D.The tachycardia mechanism cannot be determined without induction.
Question No. 3: Which of the following is correct about an ablation approach?
A.The tachycardia cannot be ablated without induction; the study should be aborted.
B.Empiric right bundle ablation is indicated.
C.Pacemapping will be associated with a 12/12-lead match at the successful ablation site.
D.A linear lesion delivered to transect sites along the posterior fascicle exhibiting Purkinje potentials can prevent tachycardia recurrence.
Discussion
Q1: The patient’s ECG demonstrates a wide-complex tachycardia with RBBB-like morphology and left-superior axis. In the absence of structural heart disease, the presumptive diagnosis is idiopathic posterior fascicular left ventricular tachycardia (ILVT). AV dissociation is apparent, confirming the diagnosis of ventricular tachycardia (VT). Other relevant features include increased velocity of the intrinsicoid deflection, ie, sharpness of the initial QRS deflection, suggesting involvement of the His-Purkinje system. The posterior fascicle serves as a critical structure within the reentrant circuit, and earliest endocardial activation during VT is commonly seen in the ventricular septum,1–3 leading to relatively narrow QRS. Other features include absence of characteristics associated with VT of myocardial origin, such as QRS duration <140 ms and time from onset of R to nadir of S <100 ms.
Aberrantly conducted beats conform to the morphology of true bundle branch blocks. The QRS morphology does not indicate the typical features of RBBB other than initial positive upstroke in V1. In fact, the QRS is significantly different than typical RBBB with an initial Q wave in V1 followed by an Rsr’ seen best in V2 and rS pattern in V5 and V6. Axis deviation from normal is not an expected feature of RBBB, though fascicular blocks can be seen with aberrancy. Reentrant tachycardia with antegrade conduction over an accessory pathway and retrograde conduction over the AV node (antidromic tachycardia) would be expected to exhibit 1:1 AV association. The identification of AV dissociation eliminates any form of SVT, including accessory pathway-mediated tachycardia.
Idiopathic LV tachycardia involves the Purkinje network of the left bundle branch system to support reentry. VT occurs in the absence of ostensible conduction disease and usually in the setting of structural normality, distinguishing idiopathic VT from bundle branch reentry and interfascicular reentry.
Q2: Dual AV node physiology would not necessarily be an unexpected finding as the majority of patients who present for EP study will have dual antegrade or retrograde AV nodal pathways, but this alone, and/or even if AV nodal echoes are seen, does not confirm a diagnosis of AV node reentry. Slow-pathway ablation is not indicated, particularly with the ECG features indicating VT. Similarly, ventricular pacing will likely demonstrate retrograde conduction over the fast AV nodal pathway if VA conduction is present, and will not provide insight to guide ablation because a retrogradely conducting accessory pathway does not participate in the tachycardia. The normal HV interval in sinus rhythm also makes antegrade accessory pathway conduction unlikely.
The tachycardia circuit of ILVT has been deduced through observations made during VT and sinus rhythm (Figure 33 B.2). In sinus, Purkinje potential (P2) recordings preceding ventricular activation demonstrate normal proximal-to-distal activation of the posterior fascicle, as in the example shown in Figure 33 B.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


