EVALUATING TRANSIENT-LOSS OF CONSCIOUSNESS AND SUSPECTED NEURALLY MEDIATED REFLEX SYNCOPE
Case presented by:
A 37-year-old otherwise healthy woman presented to the syncope/arrhythmia clinic having been referred for consultation after a spell of transient-loss of consciousness (T-LOC). The most recent episode occurred at work. She is employed doing computer-based design and had been facing a major product deadline. The T-LOC occurred with no apparent warning; however in retrospect, she recalled she had been standing beside her desk looking at graphics and remembered feeling warm and noting nonspecific gastrointestinal upset. Witnesses found her collapsed on the floor beside her desk. They noted some “jerky movements” of her arms after her collapse, and estimated that she was unresponsive for < 1 minute. Thereafter, she responded when her name was called. Co-workers reported her to be sweaty, and it was evident that she had sustained a minor laceration on her forehead and had lost bladder control.
An emergency medical team arrived within a few minutes, and the patient was taken to a nearby emergency department (ED). Apart from documenting the episode history summarized above, the patient’s past medical history revealed “one or two faints” as a child, but none in the last 25 years. The family history was unremarkable, and the patient was taking only nutritional supplements with no known cardioactive potential. In the ED, she was normotensive, alert, and fully oriented, with a normal physical examination. An ECG was obtained (Figure 3.1). Basic blood chemistry was normal. Due to the laceration, computed tomography of the head was undertaken and was normal.
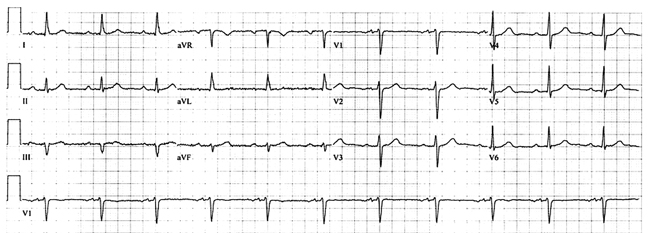
Figure 3.1. Baseline 12-lead ECG in the ED.
A.Yes.
B.No.
Did the Patient Suffer a “True” Syncope Episode?
The diagnostic evaluation of a patient who presents with an apparent T-LOC should begin by first not assuming that the episode was true “syncope.” Syncope is defined as the temporary loss of consciousness due to transient diminution of cerebral nutrient flow, most often the result of transient hypotension. The assessment should be initiated with broad consideration of the range of possible causes for real (eg, seizures and concussion) or seemingly real (eg, narcolepsy and certain psychogenic disturbances) T-LOC1 (Table 3.1). Syncope is only one of several possibilities. Consequently, the correct answer to Question #1 is: No.
Table 3.1. Pathophysiology of Various Causes of Real or Seemingly Real T-LOC
| Condition | Pathophysiology |
| Syncope | Transient self-terminating insufficiency of cerebral nutrient perfusion. |
| Concussion | Head trauma with consequent cerebral dysfunction of variable duration. |
| Epilepsy | Primary electrical disturbance of cerebral function. |
| Intoxication | Self-terminating depression of cerebral function by excess of specific agent (eg, alcohol, psychotropic drugs). |
| Metabolic | Self-terminating depression of cerebral function by metabolic disturbance (eg, hypoglycemia). |
| Psychogenic pseudosyncope, cataplexy | Not true T-LOC, mechanisms unknown. |
T-LOC, transient-loss of consciousness.
It is evident that “syncope” cannot occur in the absence of true loss of consciousness, and the latter can only be determined from the medical history obtained from the patient and/or witnesses to the episode(s). In this context, loss of consciousness implies not only loss of awareness and appropriate responsiveness to external stimuli, but also loss of postural tone. As a result, if standing, the fainter falls down; if seated, he or she slumps over. Occasionally, however, syncope may occur when the patient is supine or prone (ie, loss of postural tone is not readily apparent); such cases suggest that a hemodynamically compromising tachy- or bradyarrhythmia has occurred.
If the history indicates that there has not been clear-cut loss of consciousness associated with the “spell”, then “true” syncope is excluded. On the other hand, one can be misled. Due to lack of recall, cognitive impairment (especially in elderly “fallers”), or embarrassment, the patient may deny having lost consciousness. Reports from witnesses are often essential. Often, however, despite best efforts, it may not be possible to distinguish a faint from other conditions (eg, an accidental fall).
It is not unusual for patients to report having a sensation that “syncope” is imminent but that full T-LOC does not evolve at that time; this circumstance (which may be termed, “near-syncope”) is often described as “dizziness” or “lightheadedness.” However, these latter complaints (especially in the elderly) are nonspecific; while they may be due to an ill-defined functional cerebral disturbance triggered by a less severe transient hypotension than that needed to cause a complete faint, they may also be due to other less well-defined conditions (especially in elderly individuals). Distinguishing transient functional disturbances of cerebral function due to modest degrees of cerebral hypoperfusion, from lightheadedness or dizziness of nonspecific origin is often difficult and requires considerable attention to a detailed description of the events. One key differentiating point is that near-syncope is usually associated with a “dimming” or “graying out of vision,” whereas that is not the case with less-specific complaints.
The timing of events surrounding an apparent syncope is notoriously unreliable; most fainters and witnesses are incapable of assessing the passage of time accurately. Nonetheless, true syncope tends to be characterized by a relatively abrupt onset, perhaps within 10 to 20 seconds of warning symptoms.
A spontaneous, complete, and prompt recovery from the faint excludes a number of nonsyncope conditions that may cause T-LOC, but which do not self-terminate promptly or require medical intervention in order to reverse. Examples include coma, states of intoxication, and stroke (which may cause loss of consciousness in some instances). On the other hand, in certain forms of syncope, particularly the vasovagal faint (VVS), recovery, while rapid, may be accompanied by fatigue and a general sense of diminished energy for a lengthy period of time (often hours in duration).
Cerebral hypoperfusion differentiates “true syncope” from T-LOC due to trauma (eg, concussion), seizures (epilepsy), intoxications, or metabolic disturbances. Both trauma and epilepsy may lead to loss of consciousness with complete and spontaneous recovery, but their origins are not inadequacy of cerebral perfusion (see Table 3.1). With regard to differentiating syncope from epilepsy, the aspect that causes most confusion is abnormal motor activity. “Jerky movements” of the arms and legs for a brief period of time is not unusual in syncope and may be incorrectly interpreted as epilepsy. However, unlike typical epilepsy, jerky movements during a faint are of shorter duration, tend to occur after collapse rather than before, and do not have tonic-clonic features. On the other hand, bladder and, less often, bowel incontinence is relatively common in syncope and should not be used to suggest that a seizure had occurred.
A.Echocardiogram.
B.Electrophysiologic study.
C.48-hour Holter monitor recording.
D.Implantation of an insertable loop recorder (ILR).
E.Reassurance that this was a “benign faint,” and no specific treatment is required.
Initial Evaluation
Among patients in whom T-LOC is deemed to be due to “true” syncope, the next step is thorough evaluation of the underlying cause (Figure 3.2). The goal should be to determine the cause of syncope with sufficient confidence to provide a reliable assessment of prognosis, recurrence risk, and treatment options.1
A well-considered initial evaluation alone should permit an experienced physician to determine, with a high level of confidence, the cause of syncope in a large proportion of patients (perhaps 40% to 50%). As a rule, the initial evaluation begins with a comprehensive medical history including detailed description of symptomatic events (recognizing that often elderly patients and those with cognitive impairment may not remember or accurately relate crucial details, while in other cases, patients may not volunteer information because of risk of losing jobs, avocations, or driving privileges) and physical examination. Additionally, several additional components are crucial: (1) assessment of known comorbidities (eg, diabetic neuropathy); (2) documentation of concomitant drug therapy (including recent dose changes); and (3) family medical history.
Among the most important factors to identify in the patient with suspected syncope is whether he/she has a history of or physical findings suggesting presence of underlying structural heart disease. In this regard, the inclusion of an echocardiogram as part of the initial evaluation of suspected syncope patients can be valuable. The presence of heart disease is an independent predictor of a “cardiac cause” for syncope (ie, a primary arrhythmic cause or a cause based on a structural cardiac abnormality leading to a transient hemodynamic disturbance), with a sensitivity of 95% and a specificity of 45%; by contrast, the absence of heart disease excludes a cardiac cause of syncope in 97% of the patients.
Syncope in conjunction with exertion raises special concerns. In particular, if the faint occurs in “full flight,” one must consider the possibility of structural and/or dynamic heart lesions producing a relatively “fixed” cardiac output in the setting of vascular dilatation (eg, severe aortic or mitral valvular stenosis, hypertrophic cardiomyopathy) or arrhythmia-prone states such as myocardial ischemia or right ventricular cardiomyopathy. However, syncope during or shortly following exercise (even moderate exertion such as climbing stairs) can also occur in patients with severe autonomic dysfunction (eg, pure autonomic failure) in whom vascular control is unable to maintain adequate cerebral perfusion pressure. In addition, on rare occasions syncope occurs shortly after exertion as a consequence of a neurally mediated reflex faint (ie, a postexercise variant of VVS).
In regard to Question #2, given the circumstances, an echocardiogram is the best choice at this point of the evaluation in order to exclude structural heart disease; it proved to be entirely normal. In regard to the other choices, an electrophysiologic study (EPS) is usually reserved for patients with known structural heart disease or symptoms suggesting a paroxysmal tachycardia. Neither is the case. Holter monitoring is usually limited to 24 to 72 hours duration, and has almost no chance of capturing a spontaneous syncope recurrence as the events are so rare in this patient. An ILR might be considered; there is evidence suggesting that they may be cost-effective when used at an early stage. However, placement of such devices in the ED is not yet standard practice, although it may become more common in the future.
Question No. 3: The next best step in this patient’s assessment is:
A.Admit to a cardiology telemetry unit.
B.Admit to neurology.
C.Discharge with follow-up by internal medicine next week.
D.Discharge to a rapid-access syncope/falls clinic.
Does Management Require Admission to Hospital?
After the ED or urgent care physician has concluded that “syncope” was the most likely cause of T-LOC, a decision must be made as to whether the affected individual needs in-hospital evaluation or can be referred to an outpatient syncope evaluation clinic. In general, the issue that determines the answer to this question is an estimate of one or more of the following:
- the individual’s immediate risk (usually measured as < 1 week) of a fatal event or potential for physical injury (eg, risk of falling);
- the patient’s ability to care for him/herself; and
- whether appropriate treatment inherently requires in-hospital initiation (eg, antiarrhythmic drugs, device implantation, surgery, transfusions, etc.).
In instances when the etiology of syncope is known with certainty after initial clinical evaluation, the need for hospitalization depends in part on the immediate risk posed by the underlying problem, in addition to the treatment proposed.2,3 Thus, for example, patients with syncope accompanying complete heart block, ventricular tachycardia, acute aortic dissection, or pulmonary embolism should be admitted to the hospital and preferably to an ECG-monitored unit. On the other hand, most vasovagal fainters can be sent home after careful discussion of the nature of the problem and simple preventive maneuvers (eg, hydration, avoidance of hot crowded environments, etc.); syncope evaluation clinic follow-up suffices in most of these cases.
The following breakdowns provide an overview of common circumstances for which hospitalization is recommended or, conversely, is usually not needed.
Patients at High Risk
Several markers identify syncope patients who should be considered for in-hospital evaluation. Syncope associated with symptoms suggestive of acute myocardial ischemia or acute aortic dissection, signs, or biochemical evidence (ie, elevated brain natriuretic peptide [BNP]) of congestive heart failure, and/or suspicion of hemodynamically concerning underlying structural heart disease (eg, valvular aortic stenosis, pulmonary hypertension) have the highest immediate mortality risk. At similar high risk are patients with certain ECG abnormalities, including high-grade atrioventricular (AV) block, cardiac pauses > 3 seconds, preexcitation syndromes (eg, Wolff-Parkinson-White syndrome), or suspected ventricular tachycardia including torsades de pointes (ie, marked QT interval prolongation). Patients with syncope during exercise, and syncope causing motor vehicle or major work accidents or severe injury should also be evaluated in the hospital.
Patients at Intermediate Risk
Syncope associated with age > 50 years, history of structural heart disease but without signs of active consequences of disease, certain ECG abnormalities (eg, bundle-branch block, Q waves), family history of sudden death, cardiac devices without evidence of dysfunction, symptoms not consistent with vasovagal or reflex-mediated syncope and physician’s judgment that a cardiac syncope is possible constitute the patient group with intermediate risk for adverse outcome.
At present, guidelines for management of intermediate-risk cases are ill-defined. However, an ED-based observation unit may be useful initially; if there are no particularly worrisome physical examination, x-ray, ECG, or biochemical findings after 4 to 6 hours, the patient could be managed without hospital admission. These patients should be referred to and promptly seen (typically < 72 hours) in a syncope evaluation clinic.
Patients at Low Risk
Patients in this group typically have no evidence of structural heart disease and have a normal baseline ECG. The syncope is considered of a “relatively benign” nature in terms of mortality risk (although falls and injury risk remain a concern). As a rule, syncope in these cases is of neurally mediated reflex or orthostatic cause. However, rarer conditions that are more worrisome may present with a normal ECG; these include long-QT syndromes and preexcitation syndromes (in which the ECG abnormality is not always evident), Brugada syndrome and other less well-defined channelopathies.
Low-risk patients can generally be stabilized in the ED or clinic. Most can be reassured regarding immediate mortality risk, but early further assessment in a “syncope/falls” clinic is recommended.
In regard to our patient, there is no evidence of structural heart disease and her ECG is normal. Additionally, there is neither a worrisome past medical history nor a problematic family history. Finally, although perhaps not absolutely “classical” in terms of her presentation, the patient’s history of her most current collapse is suggestive of a neurally mediated (vasovagal) reflex faint. Consequently, we can reasonably conclude that she is in the “low-risk” group; in-hospital cardiac telemetry is not needed, and she is certainly not going to be optimally served in a neurology unit. Discharge from the ED with an appointment in the very near future (preferably ≤ 72 hours) to a syncope clinic (sometimes referred to as a syncope management unit [SMU]) is the appropriate next step. This referral was arranged from the ED, and in the interim the patient was asked to avoid driving or other potentially hazardous activities.
Syncope Management Units
SMUs have been advocated as a means of enhancing the management process for syncope patients while reducing cost.1–3 In most institutions that have SMUs, it is in reality a “virtual unit” that operates as a diagnostic and treatment consortium comprising one or more of several key medical specialties (usually cardiac electrophysiology (EP), neurology, general medicine, and geriatrics). In some hospitals (principally in Italy), the SMU may be a physical space, incorporating an observation unit and possibly an outpatient facility.
One of the objectives of establishing an SMU is to help solve the problem of too many low- and intermediate-risk syncope patients being admitted to hospital where they often are submitted to unneeded expensive diagnostic tests. In this regard, supportive evidence from two randomized trials is summarized in Table 3.2.
Table 3.2. Randomized Studies Assessing the Contribution of SMUs to Syncope Evaluation
| Study | Location | Principal outcomes |
| SEEDS | USA, single center | Diagnosis of cause of syncope increased from 10% with usual care to 67% with SMU; hospital admission was reduced from 98% to 43% with SMU; length of patient-hospital days was reduced by > 50% for SMU. |
| EGSYS | Italy, multicenter | Compared outcomes of 745 patients managed with SMU to 929 patients managed with usual care. In SMU patients, hospitalizations were fewer (39% vs 47%), in-hospital stay was shorter (about 1 day), fewer tests were performed per patient (2.6 vs 3.4), and cost per patient, and mean cost per diagnosis were approximately 20% lower. |
EGSYS, Evaluation of Guidelines in Syncope Study; SEEDS, Syncope Evaluation in the Emergency Department Study; SMU, syncope management units.
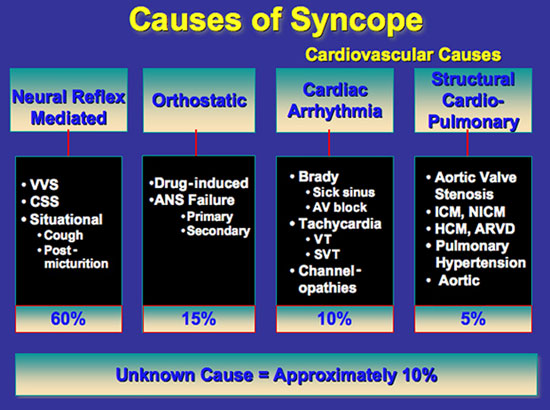
Possible Causes of Syncope
Syncope itself is not a sufficient diagnosis; in fact, syncope is better considered as a “syndrome” with many possible etiologies. Only after the correct cause is determined can one expect to make an accurate assessment of the patient’s prognosis and initiate an effective therapy strategy. There are 3 relatively common variations of neurally mediated reflex syncope: vasovagal syncope (VVS, also often termed the “common faint”), carotid sinus syndrome (CSS), and the so-called “situational faints.” The principal pathophysiological mechanism of these faints is the triggering of a neural reflex resulting in both hypotension due to vaso- and veno-dilation (including the splanchnic bed) and an inappropriate chronotropic response (occasionally resulting in severe bradycardia or asystole, but at other times causing a “relative” bradycardia in which the heart rate is less than expected for the degree of hypotension). Both vascular dilatation and/or bradycardia may diminish arterial pressure sufficiently (below cerebrovascular autoregulatory capability) to compromise perfusion to the brain, thereby causing syncope; however, the contribution of each of these two factors to systemic hypotension and cerebral hypoperfusion may vary considerably among patients and probably even within patients at different times.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


