IDENTIFYING EXTRA PULMONARY VEIN TRIGGERS FOR AF INITIATION
Case presented by:
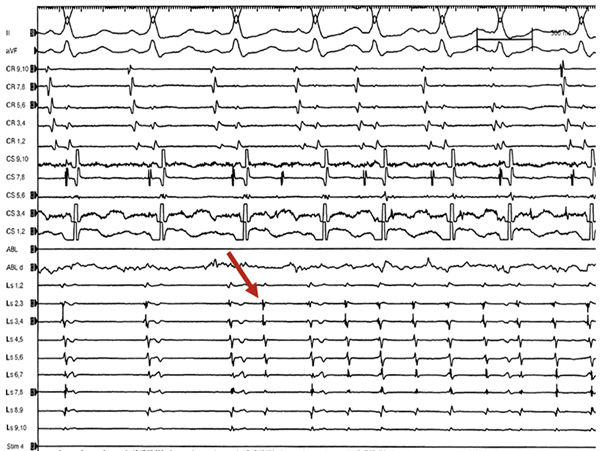
A 51-year-old female patient with essential hypertension and preserved left ventricular ejection fraction presented for atrial fibrillation (AF) ablation after a previous failed ablation for paroxysmal AF. After left atrial instrumentation was achieved by double transseptal puncture, the circular mapping catheter was placed in all 4 pulmonary vein (PV) antrum and along the posterior wall of the left atrium. All 4 PVs and the posterior wall did not regain conduction and were isolated. Challenge test with high dose of isoproterenol (up to 30 mcg/min for 15 minutes) showed no reconnection between the left atrium and the PVs. Firing from the left atrial appendage (LAA) was triggered by isoproterenol infusion at 30 mcg/min.
Question No. 1: Based on history and the electrograms (EGMs) showed in Figure 26.1, what should be done in a patient with paroxysmal AF undergoing a redo procedure with all PVs isolated and evidence of extra PV triggers
A.All demonstrated extra PV triggers should be ignored and the procedure aborted.
B.Demonstrated extra PV triggers that are initiating tachycardia or AF should be ablated.
C.Isolation of the superior vena cava should be performed.
D.All the above.
E.None of the above.
Discussion
Pulmonary vein antrum isolation (PVAI) is one of the most utilized techniques to achieve PV disconnection. Our approach is guided by a circular mapping catheter and by intracardiac echocardiography (ICE), along with the empirical isolation of the superior vena cava in either paroxysmal or nonparoxysmal patients.1–4 Specifically, in patients with paroxysmal AF, the PV antra and the portion of the posterior wall contained within the PV area are targeted during the procedures with exit block as the end point.1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


