PERMANENT JUNCTIONAL RECIPROCATING TACHYCARDIA
Case presented by:
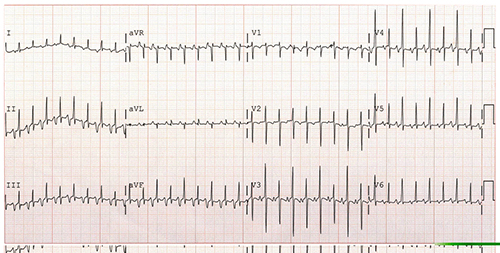
A 4-year-old male presents with a history of nausea and vomiting for a day. His parents note that he also has been complaining of his “heart hurting,” and they have noticed a decrease in his activity level over the past couple of weeks. On examination, he is tachycardic with hepatomegaly and splenomegaly. A chest x-ray demonstrates an enlarged cardiac silhouette. An ECG and echocardiogram are performed. The echocardiogram demonstrates a dilated left ventricle (LV) with markedly reduced systolic function. The ECG is shown in Figure 14.1.
Figure 14.1. Standard 12-lead ECG of the patient.
Question No. 1: The rhythm shown in Figure 14.1 is consistent with the following diagnoses except:
A.Atrial tachycardia (AT)
B.Permanent junctional reciprocating tachycardia (PJRT)
C.Typical atrioventricular nodal reentry tachycardia (AVNRT)
In typical AVNRT, the antegrade limb of the circuit is the slow pathway of the atrioventricular (AV) node and the retrograde limb is the fast pathway. Hence, atrial depolarization occurs almost simultaneous with ventricular depolarization. The larger voltage generated by the ventricles obscures the voltage generated by the atria, and P waves are not usually seen on a surface 12-lead ECG. In Figure 14.1, the T waves are not normal in their appearance. There is a P wave fused with the terminal portion of the T wave. This indicates that atrial depolarization is occurring closer in time to ventricular repolarization and not ventricular depolarization.1 This is a long RP tachycardia, which may represent an AT or a pathway-mediated tachycardia, but it is not consistent with typical AVNRT.
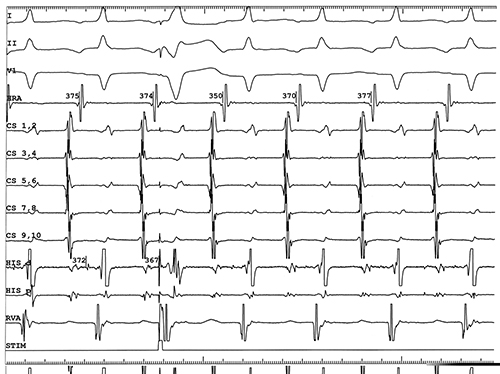
Figure 14.2. Intracardiac tracing of tachycardia. The sweep speed was 100 mm/s. Surface leads I, II, and V1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree