Average intrapleural pressure measured in patients submitted to pulmonary lobectomy and managed with a traditional device and with a regulated-pressure device (Thopaz). In these cases, the traditional system was not on suction, and Thopaz pressure was set at −2 cmH2O. By using the traditional system, wide oscillations of intrapleural pressure were evident with prolonged periods of positive values (>0 cmH2O). By using the regulated pressure system, intrapleural pressure was maintained stable at the preset value with minimal oscillations.
To simplify terminology and understanding of the ‘active drainage’, the situation where a sub-atmospheric pressure is created by an external suction device has been defined as ‘external suction applied’. In all other cases (previously referred as ‘water seal’), the definition ‘no external suction applied’ has been proposed.
Another important definition is the distinction between regulated (variable) suction and unregulated (fixed) suction. Regulated suction is a form of active drainage obtained through the application of an external source of suction capable of modifying its level of suction (negative pressure) in response to the feedback coming from the pleural space. In other words, the suction source applied to the chest drainage system is capable of varying its activity to maintain a preset value of pressure. As a consequence, these systems can be best described as suction when needed by the patient and non-suction when not (Figure 18.2). Non-regulated or fixed suction is a form of active drainage provided by an external source of suction not capable of varying its level based on the intrapleural pressure level (i.e. wall suction).
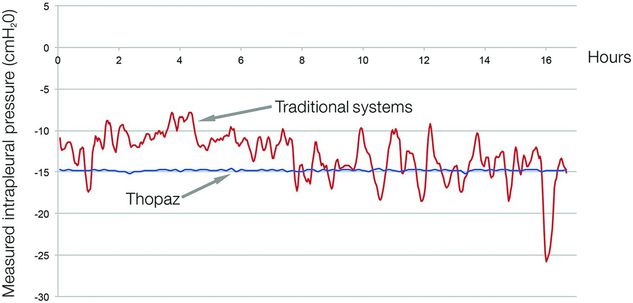
Average intrapleural pressure measured in patients undergoing pulmonary lobectomy and managed with a traditional device and with a regulated-pressure device (Thopaz). In these cases, both systems were placed on suction at −15 cmH2O. By using the traditional system, wide oscillations of intrapleural pressure were evident despite the suction, whereas by using the regulated pressure system, the intrapleural pressure was maintained stable at the preset value.
Electronic drainage systems
Some companies have recently produced and commercialized chest drainage systems with built in electronics able to measure air flow.
There are several experiences already published in the medical literature reporting on the clinical characteristics and benefits of these novel devices.
In summary, the main features of the commercially available digitalized chest drainage systems are the following:
1. Objective measurement of air leak, which improves reproducibility and interobserver agreement
2. Graphical display of trends of airflow, which assists in chest tube management
3. Recording of data for later export, retrospective analysis and medico-legal purposes
4. Compact, light and portable design
5. Built-in pump, no need to attach to chest wall for suction
6. Provide regulated, variable suction to generate a stable intrapleural negative pressure (Figures 18.1 and 18.2)
7. Intelligent systems, which work only when needed to mantain preset negative levels in the presence of air leak (suction when needed, non-suction when not)
8. Unaffected by gravity and the position of the system relative to the patient
One the most important studies about digital systems is the one published from the Salamanca group[8]. They found a high inter-observer variability among staff surgeons in deciding when to remove a chest tube when using a traditional device. On the other hand, the inter-observer agreement was almost perfect when a digital system was used to assess air leak. The main reason explaining the difference is the availability of objective data about air leak upon which to base the decision on whether to remove the chest tube.
The objective unequivocal quantification of the air leak is likely the most important factor explaining the clinical benefits found in two randomized clinical trials comparing digital versus traditional devices[9,10].
Cerfolio and colleagues[9] found that patients connected to a digital system had a shorter duration of chest tube (0.8 days less) and hospital stay (0.7 days less) than those connected to a traditional device. One interesting aspect of this study was the crossover of patients with an air leak on both devices, which made it possible to correlate the readings obtained from both systems.
The authors were able to find a certain linear correlation between the median airflow measured by the digital device and the intensity of the bubbling.
The other randomized trial showing the efficacy of digital systems over traditional ones was the one published by our group[10]. Only lobectomy patients were included in the study, with 160 patients randomized into two groups. The group connected to a digital system had a significantly shorter duration of chest tube placement, which resulted in a reduced hospital stay of about 1 day. Consequently, we were able to find a cost reduction of about 500 euros per patient. Additionally, 51% of patients with the digital drainage device had their chest tube removed by the second post-operative day compared to only 12% of those with the analog device. One of the most important aspects of this study was the use of a standardized fast-track chest tube removal protocol, taking advantage of the objective information about air leak recorded in the system. We did not rely on instantaneous assessment of air leak anymore but rather on average values of air leak, expressed in ml/min, recorded during the last 3–6 hours.
Both of these randomized trials were conducted using a system, called Digivent, no longer available on the market.
Pleural pressure
Some new electronic chest drainage systems are not only able to measure the airflow but also the pleural pressure. Little is known about the influence of the pleural pressure on the duration of air leak and even less on the importance of it to the recovery of the lung after surgery.
A recent paper combining patients from Ancona and Mayo Clinics has shown that the differential pressure (difference between minimum pressure and maximum pressure) calculated from measurements taken during the 6 post-operative hours following lobectomy was associated with the duration of air leak and the risk of a PAL[11].
Patients with an airflow greater than 50 ml/min and a differential pressure greater than 10 cmH2O have a risk of PAL > 72 hours as high as 52%.
This work may have clinical implications insofar as by modifying the differential pressure (narrowing the ‘swing’ between maximum and minimum pressure), there may be the possibility to influence the duration of air leak.
These findings were derived from data recorded by using the Digivent system, which is no longer available on the market. That system featured separate flow and pressure sensors located at the canister level, which allowed for influence by external factors such as siphoning effects and positioning of the patient.
New systems, such as the Thopaz (Medela Healthcare, Switzerland), provide more sophisticated data and clinical results. They feature a pressure sensor that measure the intrapleural pressure of the chest and contain an intelligent algorithm that controls the pump, meaning they are capable of reacting to the feedback coming from the sensor. The airflow is accurately measured (with 1% error rate) by the activity of the pump to maintain a preset level of pressure. In a sealed environment and in the case of no air leak, the pump function ceases to work once the preset negative pressure is reached, turning the system into a non-suction device. Nevertheless, it never stops measuring and recording pressure data. In the absence of air leak, Thopaz will simply observe and record the pressure of the intrapleural space.
One of the great potential advantages of regulated suction devices (i.e. Thopaz) is the capability to maintain a stable pressure even in the case of air leak with minimal variability in the range of 0.1 cmH2O (Figure 18.3). Furthermore, when the preset pressure is at or below −8 cmH2O and there is no air leak, the device works passively, as a one-way valve, only monitoring and recording the pleural pressure driven by the patient himself or herself (Figure 18.4).
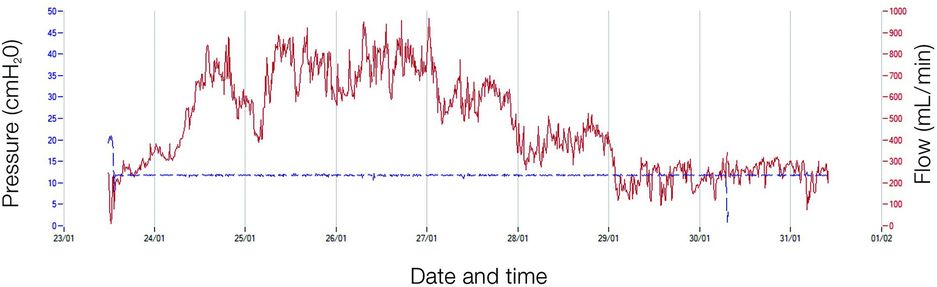
Airflow–pleural pressure graph downloaded from a regulated-pressure chest drainage system in a patient undergoing pulmonary lobectomy. The red line represents airflow, and the blue line the pleural pressure recorded at the chest. In this patient there was a prolonged period of air leak. The device worked to maintain the pleural pressure stable at the preset value without oscillations in spite of the airflow.
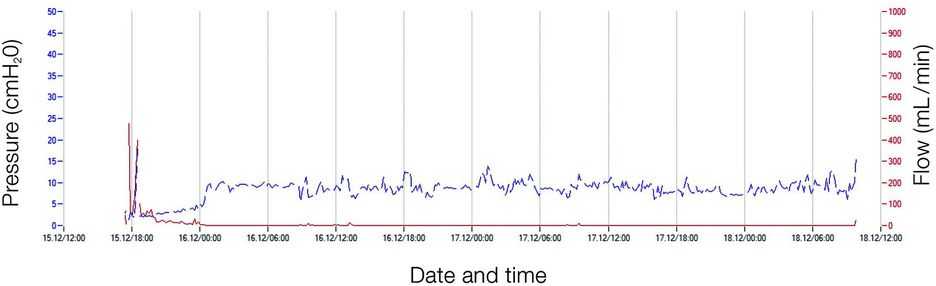
Airflow–pleural pressure graph downloaded from a regulated-pressure chest drainage system (Thopaz) in a patient undergoing pulmonary lobectomy. The red line represents airflow, and the blue line the pleural pressure recorded at the chest. There was an initial period of a few hours with some air leak and in which the pleural pressure was maintained stable at −2 cmH2O (which was the preset value in this case). Once the airflow stopped, the patient stabilized his own pleural pressure within physiological values. The device simply observed without exerting any suction.
What you set in the device is what you really get inside the pleural space. In contrast to a traditional chest drainage system, the oscillations around the preset value are minimal (Figure 18.1), which may contribute to reducing the duration of air leak, according to the aforementioned paper[11]
The introduction of these types of novel electronic chest drainage systems in clinical practice has been shown to be effective and safe. In a previous investigation, Pompili and colleagues[12] used propensity score case-matched analysis to compare the first consecutive 51 lobectomy patients managed with Thopaz with 51 counterparts managed with a traditional device.
Patients managed with Thopaz had chest tube durations approximately 2 days shorter and hospital stays 1.5 days shorter, with a consequent saving of approximately 750 euros per patient.
Moreover, compared to patients managed with a traditional system, those connected to the novel electronic device had a consistently shorter duration of chest tube since the very first cases. The ‘learning curve’ sloped down for the first 40 patients before reaching a plateau, when the maximum benefit of the electronic device was evident.
Modern chest drain devices, which are able to apply regulated suction to maintain the preset intrapleural pressure, represent the ideal instruments to reliably assess the effect of different levels of negative pressure on the duration of air leak. They may overcome the main limitation of previous trials using traditional devices and comparing suction versus no suction: the impossibility of controlling whether the preset level of suction was indeed maintained inside the chest.
In this regard, we[13] recently compared the effect of different levels of pleural pressure on the duration of air leak under controlled conditions by using a regulated chest drainage system (Thopaz). One hundred patients undergoing pulmonary lobectomy were randomized to receive two different types of chest drainage management: group 1, regulated individualized suction mode, with different pressure levels depending on the type of lobectomy and ranging from −11 to −20 cmH2O based on a previous investigation[7]; group 2, regulated seal mode (−2 cmH2O). At this low level of suction, the system works only to compensate the occurrence of values more positive than −2 cmH2O in case of air leak. Otherwise, it works passively as a regulated, non-suction device. We found that the average air leak duration and the number of patients with PAL were similar between the groups, showing that a regulated seal is as effective and safe as regulated suction in managing chest tubes following lobectomy. Although this experience can be refined with the application of different levels of suction or different endpoints, it will contribute to set the basis for future investigation on active pleural management based on regulated pleural pressure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


