Pectus excavatum.
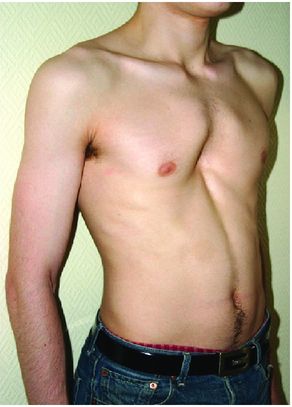
The deformity is usually noted soon after birth or in early childhood and often becomes more marked during the period of rapid growth in puberty. It may be symmetrical or asymmetrical and sometimes associated with scoliosis or kyphoscoliosis. If asymmetrical, the depression is usually more marked on the right, and the sternum is rotated rightward and angled posteriorly[1,2].
There are several hypotheses behind the development of pectus excavatum. These include intrauterine external pressure, muscular imbalance, thickened substernal ligament and, most commonly accepted, (in some cases asymmetrical) sternocostal cartilage overgrowth. In some cases the ultrastructural and biochemical studies of cartilage from affected patients revealed decreased level of zinc and increased level of magnesium and calcium[4]. Given the association with Marfan syndrome and similar phenotypes and the familial nature of some cases of pectus, it is likely that there is an important genetic component.
The affected individuals seek medical attention due to embarrassment over the appearance, exertional dyspnea, poor stamina, pain and occasionally palpitation. Apart from the depression of the lower sternum, a typical posture of a tall, thin patient with a ‘pot-belly’, forward, drifted shoulders and flaring of the costal margin is often seen. Severe scoliosis with a Cobb angle1 of more than 15° and usually rightward curvature between the fourth and ninth thoracic vertebrae is found in approximately 15% of patients.
Patients often develop nipple and, in females, breast asymmetry. A systolic murmur might be present in severe cases due to compression of the heart and mitral regurgitation secondary to valve prolapse. Echocardiographical studies revealed mitral valve prolapse in 18–65% of patients with severe deformity and compression of the ventricle in up to 95% of patients during exercise, with significant reduction of prolapse and ventricular compression after correction of the deformity[5,6]. Pulmonary function tests may show a moderate restrictive pattern with a reduced forced vital capacity. Interestingly, despite subjective improvement of patients post-operatively, some patients do not show significant improvement in pulmonary function tests[7]. However, there is some evidence showing that correction of pectus excavatum can have a positive impact on cardiac function during exercise[8,9].
The psychological impact of the deformity on patients cannot be underestimated. Patients are often teased by their peers and siblings or overprotected by parents. This leads to avoidance of swimming, sports and situations when the shirt would be removed in front of others. Lower self-esteem and social anxiety are frequent consequences.
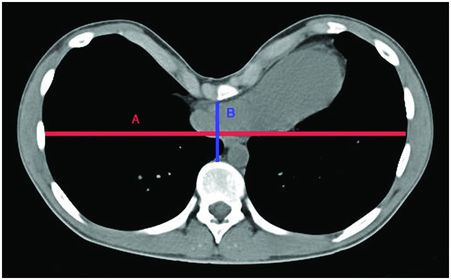
Several radiological indexes were developed to objectively measure the severity of pectus deformity. The most commonly used Haller (pectus) index is a ratio between transverse chest diameter (A) and distance from the posterior aspect of the sternum to the anterior surface of the spine (B) at the level of the deepest part of the deformity (Figure 21.2). The diameters are taken from axial computed tomography or lateral and postero-anterior chest radiographs. This ratio for normal individuals is around 2.5, and it is more than 3.2 in patients with severe pectus excavatum[10].
Treatment
Open repair
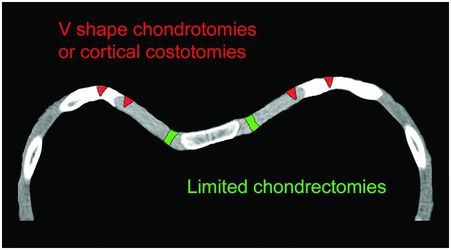
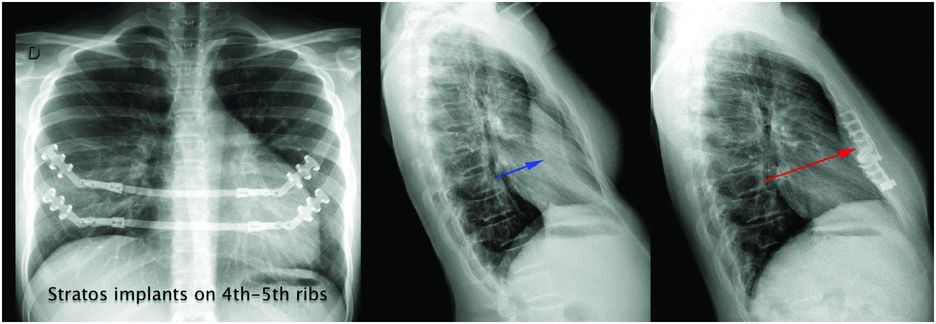
The first surgical repair with resection of rib cartilages was attempted by Meyer in 1911, but his operation did not improve the deformity. German surgeon Sauerbruch is credited with the first successful repair in 1913, and the ‘Sauerbruch procedure’ comprises bilateral resection of the third to fifth costal cartilages, sternal osteotomy and external traction of the sternum for 6 weeks after the operation. Mark Ravitch in 1949 further developed the open repair. The main feature of the original ‘Ravitch procedure’ (Figure 21.3) was an intra-perichondrial resection of the abnormal costal cartilages, perichondrial repair, resection of the xiphisternal junction, release of substernal ligament, transverse cuneiform osteotomy of sternum and its fixation in a corrected position with Kischner wires or sutures[11]. Modifications were made by different surgeons to prevent possible complications, the most important modifications being more limited cartilage resection with preservation of lateral and medial cartilage to retain the growing centres and mobility of sternocostal joints, use of metal struts for stabilization of the sternum to prevent recurrence of deformity and use of Marlex mesh to avoid second operation for removal of strut, which is usually performed about 1 year after correction (Figure 21.4)[12].
Titanium implants maintaining the correction and cardiopulmonary decompression.
In the sternal turnover technique, the cartilages are resected, and the sternum is mobilized and rotated by 180°. This procedure was popular in Japan, but a high incidence of osteonecrosis and fistula formation in 46% of patients precluded widespread use of this technique[13].
Minimally invasive repair (MIRPE)
Donald Nuss introduced a less invasive procedure for correction in 1998[14]. Cartilage resections, sternal osteotomy and liberation are not required. The correction of deformity is achieved by the placement of a semi-customized stainless steel curved bar which moves the sternum to the correct position, leading to cartilage remodelling over time (Figure 21.5). The bar is inserted via relatively small lateral incisions through a tunnel created between the pericardium and maximal sternal depression. Once in place, the bar is turned over by 180° with the convexity pointing anteriorly and secured with lateral stabilizers. There is a potential risk of injury to the heart, so thoracoscopic guidance was added to the original operation to decrease such a risk. The bar is usually removed after 3 years[15]. In some cases, two or more bars may be needed.
Front and lateral chest X-rays of a Nuss bar in place.
Complications and results of surgery
There is a spectrum of possible complications either early or late after repair. The obvious complications include pain, infection, seroma, bleeding, haemothorax and pneumothorax, atelectasis, pneumonia, injury to the heart and great vessels, liver injury, residual deformity, recurrence of deformity, allergy to metals, dislodgement or fracture of the substernal bars, pericarditis, keloid formation and psychological problems. The more specific complications include floating sternum due to extensive resection of costal cartilages and liberation of the sternum, acquired restrictive thoracic dystrophy (acquired Jeune’s syndrome) due to injury to the growing centres of costal cartilages in children, sternal necrosis, acquired scoliosis secondary to biomechanical forces after minimally invasive repair of asymmetrical forms and acquired pectus carinatum due to overcorrection, especially in patients with connective tissue disorders. There are also unfortunate cases of asymmetry and retarded growth of the breasts due to injury of developing breast tissue as a result of poorly placed skin incisions in pre-pubescent girls[16]. This complication must, of course, be considered and avoided.
Despite the aforementioned complications, the results of open and minimally invasive procedures are very good, with minimal recurrence and patient satisfaction around led 95%. Although there are no randomized, controlled trials comparing the Ravitch and Nuss procedures, a recent meta-analysis of prospective and retrospective studies showed no significant differences in the overall complication rate in both procedures[17].
However, rates of re-operation for bar migration, persistent deformity, pneumothorax and haemothorax were significantly higher with the Nuss procedure. Duration of surgery was significantly longer by 70 minutes for the Ravitch procedure. There was no difference in length of hospital stay, time to ambulation or patient satisfaction[18].
Specific considerations
Age of repair
Pectus excavatum is often noticed early after birth, but it may not be evident till later in childhood. It tends to progress to at least mid-teens. The timing of corrective surgery remains a matter of debate. Earlier repair has the potential advantage of flexibility of the chest and a lower risk of costal flaring developing. Psychological and physiological impacts may also be minimized if repair is performed before commencing school. The development of an acquired restrictive thoracic defect in the original Ravitch cohort discouraged early repair with a recommendation not to operate before the age of 8. An increasing age of repair is seen in large paediatric registries, in which the mean age for operation has increased to 14 years[19]. This is challenged by some, who state that the Ravitch procedure can be performed safely in patients from 3 years of age if the medial and lateral fourths of costal cartilages are spared.
The situation is different in patients with Marfan and other connective tissue disorders due to a higher risk of recurrence or acquired pectus carinatum. In these patients, it is recommended to perform the operation after the patient is fully grown. Operation should also consider the needs of other problems that these patients may have, for example, surgery for aortic disease.
In general, the Ravitch procedure is the preferred option for fully grown adults due to the less compliant chest wall and risk of costal flaring (which may be treated at the same time if already present), although recently published data show good mid-term results with the Nuss procedure if more than one bar is used for correction[20]. Consequently, in the future there may be more use of the Nuss in older patients[21].
Symmetry of deformity
Asymmetry of chest deformity usually develops or progresses during growth of a child and is thus more common in adolescents and adults. The Ravitch procedure is usually preferred for asymmetrical forms, although specific techniques of morphology-tailored bar shaping for correction by Nuss procedure also provide good results[22,23].
Incision
Two small lateral chest incisions are generally used in the Nuss procedure, which gives excellent cosmetic results. Horizontal or vertical incisions can be used in the Ravitch procedure. The advantage of a vertical incision is of an easier approach to deformed cartilages with shorter length of scar. In contrast, sub-pectoral transverse incisions allow better access to inferior costal flaring and an easier positioning of bars, which can also be removed through the lateral parts of the same incision. Submammary incisions are cosmetic and also allow combined or staged breast augmentation or reconstruction. It is essential that the incision is placed appropriately to avoid injury to breast tissue.
Resuscitation
With new procedures, new issues develop. The bar in the Nuss procedure requires a modified approach if cardiopulmonary resuscitation is required. It is argued that the bar prevents effective chest compression. Chest depressions should be performed with higher force, and early chest opening or bar removal should be considered if soon after surgery. Anterior and posterior placement of defibrillation pads is also necessary to provide effective defibrillation[24].
Internal mammary artery injury and patency
There is risk of direct injury to mammary arteries during dissection in both the open and Nuss procedure, which can have implications if future coronary artery bypass grafting is required. Interestingly, recent data show that even without direct injury, the bar in the Nuss procedure compromises flow in the mammary artery by pressure against the sternum in 44% of patients, usually with bilateral mammary occlusion[25].
Cardiac surgery and pectus excavatum
Congenital and acquired cardiac diseases in patients with pectus excavatum present challenges during cardiac surgery. These include exposure, positioning the sternal retractor, harvesting the mammary artery, aortic cannulation and difficulty in closing the chest. Simultaneous repair is advantageous in that it avoids two operations but also due to an early improvement in right ventricular function[26]. A modified Ravitch procedure is an option but is time-consuming and requires additional dissection and cartilage resections. So, recently, several authors have advocated an ‘open Nuss’ technique, easy to perform under visual control, before closing the sternotomy[27,28].
Multidisciplinary approach
Due to the complexity of problems in some patients, advice and cooperation with other specialities are of great importance to allow optimal timing and results of corrective surgery. These include paediatricians, physiotherapists, orthopaedic surgeons, plastic surgeons, cardiologists, cardiac surgeons, geneticists and psychotherapists.
Pectus carinatum (Pigeon chest)
Pectus carinatum is characterized by an anterior projection of the sternum with adjacent anterior ribs and represents nearly 10% of all congenital chest wall abnormalities. A geographical difference is described. One of the author’s personal experiences is that this is 15–20% in Europe and up to 50% in parts of South America. The shape of the deformity has a similar shape to the keel of a ship, hence the Latin word ‘carinatum’. It usually develops between 11 and 15 years of age, and its aetiology is thought to be similar to pectus excavatum. It is associated with scoliosis in approximately 15% of patients and with an increased incidence of congenital heart disease especially in Marfan patients.
Two types are included in this category according to the affected part and shape of the sternum and to a different aetiology: pectus carinatum of vertical type (chondrogladiolar or ‘chicken breast’; Figure 21.6A) and pectus arcuatum (chondromanubrial or ‘pouter pigeon breast’ or Currarino-Silverman syndrome) sometimes associated with an excavatum shape of the lower sternum (Figure 21.6B).
The pectus carinatum type is the most frequent, occurring in about 90% of all cases. The sternum projects anteriorly to a point corresponding to the bottom of the sternal body with the xiphoid process and the adjacent lower cartilages angling posteriorly and a slightly concave shape of the anterior ribs laterally. One-third of patients have an asymmetrical form with anterior displacement of usually the lateral part of the sternum and anterior ribs on only one side leading to rotation of the sternum. The Haller index is measured in the same way as described for pectus excavatum and is usually less than 1.9. The aetiology is similar to pectus excavatum due to an excessive length of sternocostal cartilages, mainly in the middle and lower parts of the deformity[1,2].
Pectus arcuatum is the least common type, occurring in about 10% of all carinatum deformities, with a relative anterior protrusion of the angle of Louis and second and third costal cartilages (sometimes described as ‘horn of Steer’) associated with an inferior depression of the lower part of the sternum in some cases. In this case, there is a premature fusion of the manubrium and segmental pieces of the sternum, leading to a characteristic short and broad flat bone without cartilage at the manubriosternal junction.
Presentation is usually with embarrassment over appearance, breathing difficulties and pain when lying prone or inadvertently bumping into objects. Many patients avoid swimming and sports activity with similar psychological consequences as pectus excavatum. Severe forms have an impact on pulmonary function with a restrictive pattern and also impaired diaphragmatic function at exercise due to diaphragmatic flattening. Some patients report improvement of breathing difficulties after operation, although objective evidence for this improvement is equivocal.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree