■ A 65-cm 4-Fr angled catheter (e.g., Kumpe®) is advanced through the sheath and, under digital subtraction roadmapping guidance, directs the hydrophilic guidewire into the ipsilateral internal iliac artery (FIG 2). The catheter is then advanced securely into either the anterior or posterior divisions. The C-arm gantry is positioned at approximately 30 degrees contralateral anterior-oblique for optimal visualization during this maneuver. With access secured, the 6-Fr sheath is then advanced over the 4-Fr catheter into the proximal internal iliac artery.
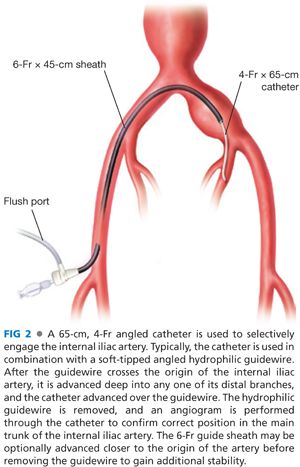
■ A selective internal iliac arteriogram is obtained through the 6-Fr sheath, and the angle catheter is retracted to the first bifurcation of the internal iliac artery. Typically, distal access is maintained with the wire during this maneuver.
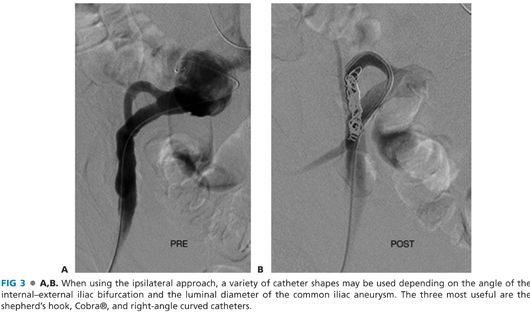
■ [Alternate technique] Depending on anatomic considerations (e.g., tortuosity, iliac bifurcation angle, internal iliac branch anatomy, etc.), ipsilateral access may be feasible. In this case, a 25-cm, 6-Fr sheath is advanced from the ipsilateral femoral artery. A 4- or 5-Fr appropriately shaped catheter (curve or reverse curve) directs the hydrophilic guidewire into the internal iliac artery (FIG 3). If a shepherd’s hook catheter type is employed, the hook may be reformed either in the iliac aneurysm or in the aorta, depending on their respective luminal diameters. The ipsilateral approach is more demanding technically and is not recommended when concomitant internal iliac aneurysm embolization is also indicated.
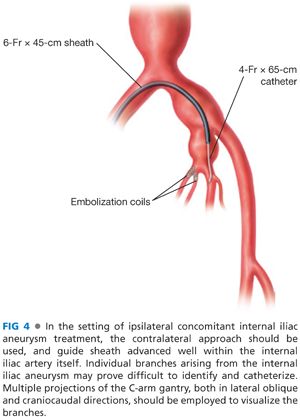
■ Size-appropriate platinum occlusion coils are deployed through the 4-Fr catheter into the main internal iliac artery trunk, with care taken to avoid placement or distal migration into arborizing branches or reflux back into the main iliac circulation. Alternative vascular occlusion devices may also be used for internal iliac embolization, including hydrogel coils and nitinol mesh (e.g., Amplatzer®) plugs. Interval arteriograms are obtained using small volume hand injections through the sheath or catheter to guide deployment and confirm positioning. Complete occlusion of the target artery during deployment is not necessary or even desirable. Following subsequent endograft deployment over the internal iliac artery orifice, in the absence of antegrade flow, the extensive surface area of the coils induces rapid thrombosis following reversal of anticoagulation at the end of the procedure. Usually less than five coils will suffice to ultimately induce complete occlusion.
■ [Alternate technique] The presence of an internal iliac aneurysm, either with or without an associated proximal common iliac aneurysm, deserves special consideration. In these situations, more extensive embolization of the internal iliac circulation will be necessary to prevent retrograde (type II) endoleak. Individual internal iliac branches must be separately embolized at the initial procedure (FIG 4). If left untreated, due to collateral pelvic flow, these branches unfortunately remain patent following endograft deployment, severely limiting options for secondary procedures. Complete branch vessel embolization can be time consuming and tedious, due to the sheer number, anatomy and sizes of the branches that must be occluded, requiring patience, expert catheter and guidewire skills, and excellent intraoperative imaging.
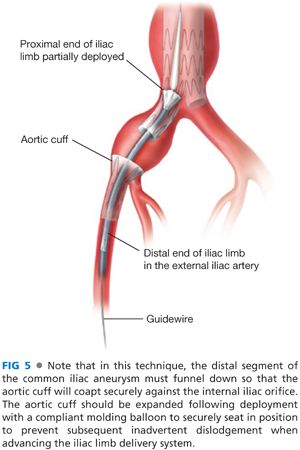
■ [Alternate technique] When the common iliac aneurysm tapers to a funnel near the iliac bifurcation, the so-called sleeve technique may be employed to occlude the adjacent internal iliac artery. In this method an appropriately sized aortic cuff is deployed into the distal common iliac artery and over the internal iliac artery origin. The distal end of this cuff is partially extended into the external iliac artery. The iliac limb is next passed through the aortic cuff and deployed normally from its proximal landing zone and into the external iliac artery 20 mm distal to the aortic cuff (FIG 5). The putative benefit of this technique is avoidance of potential atheroembolization that may occur during standard coil occlusion techniques from catheter manipulation, which some speculate is the cause of ischemic complications following internal iliac artery occlusion.
■ Following internal iliac occlusion, subsequent aneurysm exclusion procedures vary as functions of landing zone and aneurysm anatomy. Endograft deployment nearly always follows management of the internal iliac artery in some form or another. In the typical scenario, following internal iliac embolization, the endograft positioning and deployment proceeds in the standard fashion except for extension of the ipsilateral distal landing zone beyond the iliac bifurcation to the external iliac artery. At least 20 mm of purchase into the external iliac artery is recommended.
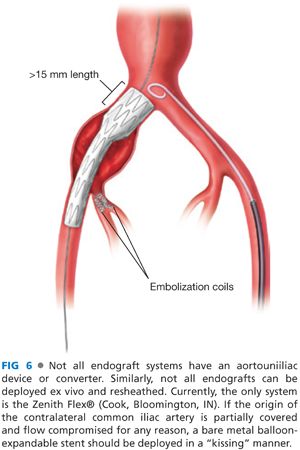
■ In the unusual case of an isolated common iliac aneurysm without aortic involvement, with a proximal uninvolved segment at least 20 mm in diameter and 15 mm in length, a short endograft may be deployed to bridge the proximal common and external iliac arteries.2 Device options for this approach include either the “off-label” deployment of an aortouniiliac converter graft or placement of a flared or “bell bottom” iliac endograft limb that has been previously deployed, reversed, and reloaded into the delivery sheath at the back table (way off-label). These adaptations are often necessary because although nonaneurysmal, the common iliac artery is still too large to securely seat the proximal end of most iliac limbs. To obtain a satisfactory proximal seal, the distal flared segment, commonly available in diameters up to 24 mm, is deployed proximally by simply reversing the limb in the sheath (FIG 6).
ENDOVASCULAR COMMON ILIAC ARTERY ANEURYSM REPAIR WITH INTERNAL ILIAC PRESERVATION
■ These techniques specifically pertain to common iliac aneurysms without an associated ipsilateral internal iliac aneurysm. In cases of an internal iliac aneurysm (see exception below), preservation methods are not possible and selective branch occlusion (see above) and endovascular exclusion are necessary.
■ Indications for internal iliac artery preservation may include the following:
■ Routine revascularization as procedural preference
■ The presence of contralateral internal iliac occlusion
■ Active patient with concern/potential for buttock claudication
■ Diabetic with diseased ipsilateral deep femoral artery (reduced potential collateral supply)
■ Prior thoracic endograft repair (concern regarding anterior spinal artery collateral flow arising from the internal iliac circulation and potential for postoperative paraplegia)
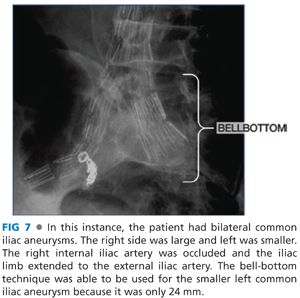
■ The simplest internal iliac preservation technique involves deployment of flared or so-called bell-bottom devices. Although anecdotally applied to larger aneurysms, conventionally, this technique is limited to common iliac artery aneurysms with 24-mm or shorter diameter distal landing zones. As an off-label modification of this technique, for common iliac aneurysms with larger or poorly defined distal landing zones, the maximal diameter flared iliac limb is intentionally deployed approximately 2 cm proximal to the internal iliac artery orifice. An aortic extension cuff without a proximal uncovered stent (typically 28 mm) is then deployed halfway into the unsecured iliac limb and flared out into the distal aneurysm, essentially creating a larger landing zone than that conventionally available (FIG 7). Although strictly speaking, cuff deployment is essentially in the aneurysm itself; late outcomes from these procedures appear favorable, with a low reported incidence of migration or type Ib endoleak.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


