Type
Cause
Respiratory drive
Pharmacological
Drug overdose, anesthesia
Congenital
Central hypoventilation syndrome
Acquired
Cerebrovascular accident
Neuromuscular
Cervical spinal cord injury
Trauma
Chronic inflammatory demyelinating polyneuropathy
Guillain–Barré syndrome
Anterior horn disease
Poliomyelitis
Phrenic nerve injury
Trauma, cardiac surgery
Muscles of respiration
Pharmacological
Neuromuscular blocks
Congenital
Hypophosphatemia
Acquired
Kyphoscoliosis, trauma
Rib cage
Decreased mobility
Alt. Pleura
Extrapulmonary restriction
Pneumothorax, pleural effusion
Airway
Upper airway obstruction
Epiglottitis, foreign body
Lower airway obstruction
Asthma
Increase in dead space
Increased ventilation/perfusion ratio
Emphysema
Decreased ventilation/perfusion ratio
Acute respiratory distress syndrome
General pulmonary hypoperfusion
Hypovolemia, cardiogenic shock
Localized hypoperfusion
Thromboembolism
Physiopathology
There are five physiopathological mechanisms that can alter the homeostasis of gases and lead to respiratory insufficiency: (1) an alteration in the alveolar ventilation and pulmonary perfusion ratio (V/Q ratio); (2) a shunt (short circuit); (3) hypoventilation; (4) an alteration in the diffusion of gases in the alveolocapillary membrane; and (5) a decrease in the concentration of inhaled oxygen. The three most important are the V/Q ratio, hypoventilation, and a shunt, with a decrease in inhaled O2 being considered a minor clinical implication of acute respiratory insufficiency.
Ventilation/Perfusion Alterations
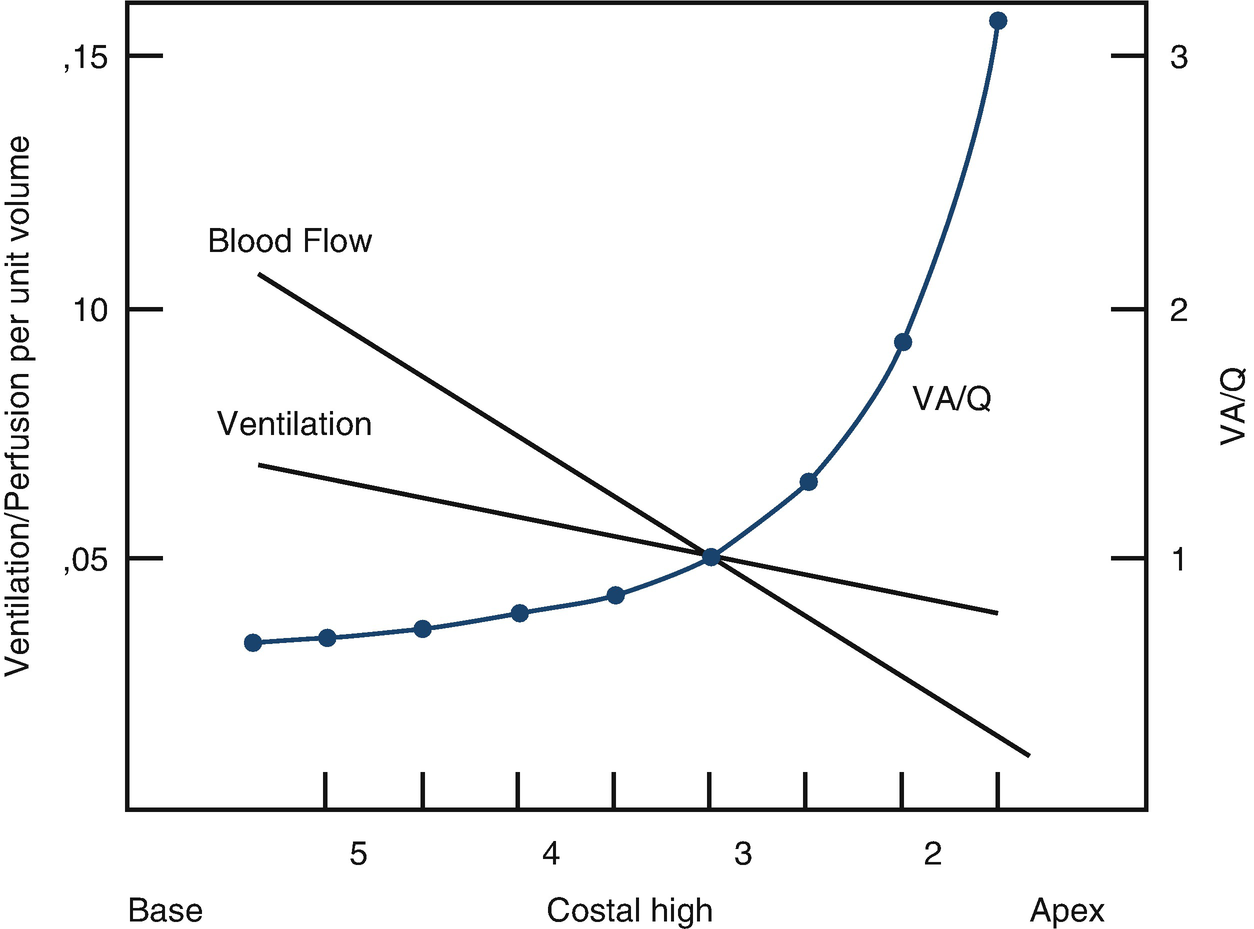
Ventilation distribution, blood flow, and ventilation/perfusion (V/Q) ratio
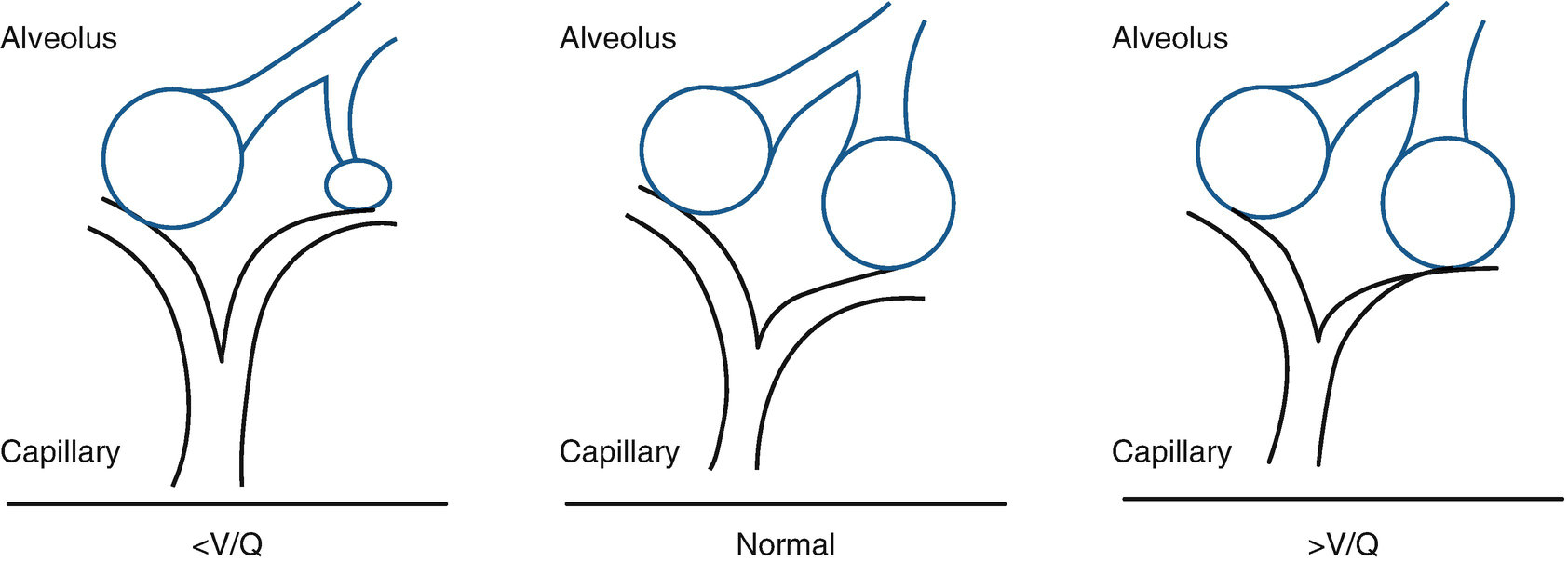
Ventilation/perfusion alteration
In a person who is breathing spontaneously, there are compensatory mechanisms to correct hypoxia and/or hypercarbia. In the context of hypoxemia, pulmonary vascular vasoconstriction consists of the alveolar units with better V/Q ratios an excluding those that are poorly ventilated, while the increase in VA as a response to hypoxia prevents an increase in PcO2, including lowering it to below normal levels.
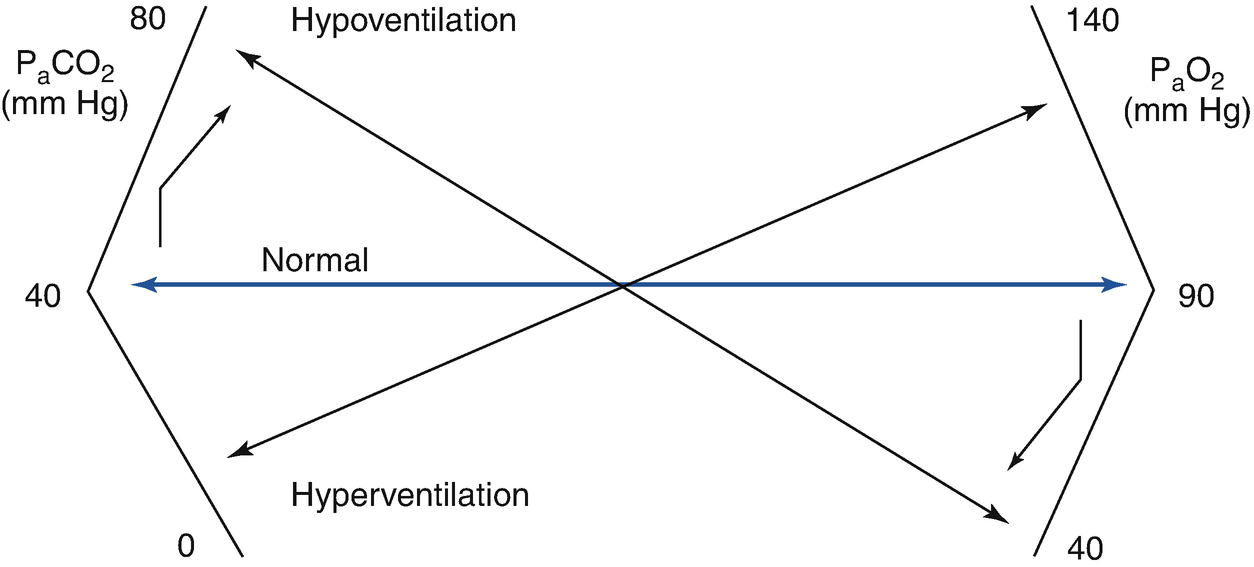
Hypoventilation
PaO2 is determined by the balance between oxygen provided by VA (which provides oxygen from inhaled air) and the extraction of oxygen by capillary blood. Consequently, when VA decreases significantly, PaO2 decreases and PcO2 increases, which are the fundamental characteristics of hypoventilation.
PcO2 is determined by VA and the production of CO2 (VCO2), multiplied by the K constant, as is seen in the formula PaCO2 = (VCO2/VA) × K, from which it can be deduced that increased CO2 production or a decrease in VA increases PaCO2. As the compensatory renal response to hypercarbia is slow (bicarbonate retention), there is an acute fall in arterial pH.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


