INDICATIONS/CONTRAINDICATIONS
This chapter deals with the technique for video-assisted right superior and basilar segmentectomy. The indications for video-assisted segmentectomy are similar to open segmentectomy and are the same for all segments. Video assistance refers to the visual guidance used to perform the procedure.
Segmentectomy is a useful option in the management of benign disease limited to either the superior or basilar segments that can be managed with segmental resection. Metastatic disease, unable to be managed with a wedge resection can also be treated with segmentectomy, as long as oncologic principles are followed. There continues to be debate as to the utility of segmentectomy in the management of primary lung cancer. The largest randomized controlled trial to date examining the outcomes of patients treated with segmentectomy versus lobectomy for early (T1N0M0) non-small cell lung cancer (NSCLC) concluded that segmentectomy resulted in higher local recurrence and lower overall survival (Ginsberg, 1995), a result which has also been observed in a later study examining the SEER database (Whitson, 2011). Variations in technique and margins of resection may account for this variability. In contrast, individual studies have demonstrated similar outcomes between segmentectomy and lobectomy for nonsmall cell lung cancer (Okada, 2006; Tsutani, 2013), although none of these were randomized prospective studies.
Although segmentectomy is typically offered to individuals who would not tolerate lobectomy, currently we offer it to individuals with small (<3 cm) peripheral lesions. As the debate over the oncologic acceptability of segmental resection continues, we follow select criteria for the use of this limited resection in patients with nonsmall cell lung cancer. It is our practice to perform segmentectomy in patients with typical carcinoid tumors and small cancers when in favorable anatomic locations. Although some may consider previous thoracotomy or other extensive adhesions as a contraindication to VATS segmentectomy, we have not found this to be the case.
Indications for Segmental Resection
 Benign disease: Pathology within segment
Benign disease: Pathology within segment
 Metastatic disease: Pathology inadequately resected with a wedge resection
Metastatic disease: Pathology inadequately resected with a wedge resection
 Primary lung cancer: Early stage disease following sound oncologic principles
Primary lung cancer: Early stage disease following sound oncologic principles
Absence of lymph node metastases
Adequate parenchymal margins
Unable to tolerate a lobectomy
Contraindications for Segmental Resections
 Pathology not adequately treated with a segmental margin
Pathology not adequately treated with a segmental margin
 Lymph node metastases
Lymph node metastases
 Adhesions (relative)
Adhesions (relative)
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
Workup of pathology being treated with a segmental resection should follow guidelines for the management of the suspected or proven pathology and will not be reviewed.
For video-assisted segmental resections, a careful review of the bronchial and vascular anatomy pertaining to the planned segmental resection is important to identify any aberrant vasculature that may complicate the resection. In particular, one should also pay close attention to the vascular anatomy that will be left behind to the remaining lobar segments, as inadvertent division would prevent sparing these segments.
Critical three-dimensional knowledge of the anatomy is crucial to safely and successfully performing these types of procedures. For superior segmentectomy and basilar segmentectomy, the surgeon should have an intimate understanding of the three-dimensional anatomy. The knowledge should be such that one can mentally visualize the bronchovascular structures through the parenchyma (Fig. 24.1).
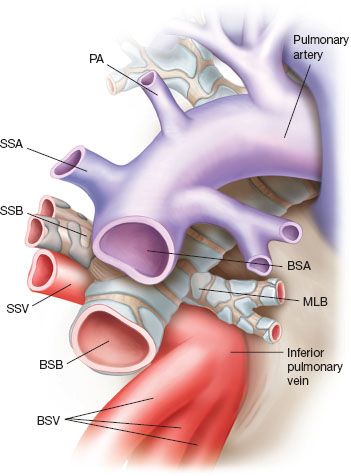
Figure 24.1 Three-dimensional anatomy of the right lower lobe artery, vein, and bronchus as viewed between the fissure of the upper, middle and lower lobes. The location of the pulmonary artery (PA), superior segmental artery (SSA), superior segmental vein (SSV), superior segmental bronchus (SSB), middle lobe bronchus (MLB) basilar segmental artery (BSA), basilar segmental vein (BSV), and basilar segmental bronchus (BSB) are marked.
 SURGERY
SURGERY
As with any pulmonary resection, detailed discussion regarding operative approach, ventilation needs, planned procedure, fluid management, and patient-specific factors must occur with the anesthesia team prior to the start of the case. The surgeon should perform a detailed flexible bronchoscopy prior to the procedure to evaluate the extent of endobronchial lesions or anatomic variations in the bronchial anatomy.
Positioning
Following bronchoscopy, the patient is positioned in a left lateral decubitus position with the table broken at the level of the hip. Rather than position as one would for a posterolateral thoracotomy, we tend to modify positioning for more anterior exposure. The patient’s shoulders are rotated exposing the anterior axillary line. The right elbow is also rotated cephalad to encourage the latissimus to a more posterior location. This allows the utility incision to be made without going through the latissimus dorsi muscle and keeps the thoracodorsal nerve out of the way of the utility port (Fig. 24.2).
Technique
The approach for video-assisted segmentectomy is the same that one would use for video-assisted lobectomy. Our approach is somewhat different from others in that we do not use the posterior port for anything more than 5-mm instruments. Given that the posterior intercostal spaces are narrower than the anterior spaces, placing staplers or other larger instruments through this port may increase trauma to the intercostal nerve.

Figure 24.2 Patient in a left lateral decubitus position. Left shoulder rotated under and right elbow rotated in the cranial direction to force the border of the latissimus dorsi to a more posterior position and expose the axilla.

Figure 24.3 Standard laparoscopic instrument at top of image compared with the pediatric laparoscopic instrument. Metal ports 3 mm, 5 mm, and 10 mm in diameter as seen from left to right.
Instruments
We frequently use the 3-mm pediatric laparoscopic instruments. These are much shorter than the standard laparoscopic instruments, eliminating the ergonomic challenges of using traditional laparoscopic instruments. As well, they allow one to finely dissect structures when needed. Also one should have a laparoscopic needle driver on hand to repair small vessels or for other suturing needs. We also use a laparoscopic knot pusher to tie sutures on vessels or other knots, as when sewing the bronchus closed, as an alternative to stapling. All of our resections are performed with a 5-mm 30-degree thoracoscope.
We use two 5-mm metal ports, a single 10-mm port, and a soft tissue retractor for the utility port (Fig. 24.3). At times, we may only use three ports, but have found the addition of a fourth 5-mm port useful as we do not have to move the camera from the anterior to the posterior port as frequently. To use the staplers from the anterior port, it is necessary to use articulating staplers.
The first site of entry into the chest is in the sixth or seventh rib space at the anterior axillary line with a 10-mm port. A second 5-mm port is placed posteriorly below the scapula, at the seventh intercostal space. A third 3- to 5-mm port is placed either between these two, usually a rib space or lower or alternative location as needed. The optimal location for the location of the utility port is identified with the camera in the chest, positioning the port directly over the location of the artery in the fissure. This incision is typically a 3- to 4-cm incision that allows extraction of the specimen and placement of multiple instruments (Fig. 24.4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


