Figure 27.1
Surgical technique; digital dissection of the trachea and innominate artery and scope insertion. Positioning is similar to that of conventional mediastinoscopy, with the patient supine, the neck reclined but not fixated, the surgeon at the patient’s head, and the scrub nurse at the patient’s right shoulder. The video monitor is placed above the patient’s midline at a comfortable distance and height for the surgeon. The surgeon sits down as soon as the mediastinoscope is introduced and takes the pedals of the electrocautery unit between his or her feet. Strictly using the left foot for the “yellow” cutting current and the right one for the blunt coagulation current avoids the inadvertent activation of “cutting” instead of “coagulation,” which may have fatal consequences if the probe is in contact with or close to larger vessels. Prerequisite is a spreadable video-mediastinoscope. Other basic requirements are a suction–coagulation device, an electrocautery unit providing “soft” coagulation, a grasper, scissors, a clip applicator, and a sponge stick. Using fixation gear for the scope, VAMLA may be performed by one surgeon. Jugular access to the trachea is the same as for standard mediastinoscopy. For quickest access, instrumentation should be restricted to the index finger compressing and retracting the tissue cranially in the midline, with the scissors in the other hand for dissection. Additional instruments, such as retractors, will deepen the wound, especially in obese patients, thus prolonging the operation. The pretracheal fat pad is separated digitally from the trachea, and then from the innominate artery. First, the index finger follows the trachea. Then, the hand performs a 180° rotation and is pulled back until the fingertip reaches the caudal circumference of the ventrally crossing artery. After the pretracheal fascia is broken by the surgeon’s finger, the fat pad is removed from the artery by gentle wrist rotation, abduction, and adduction. This maneuver is performed essentially to allow subsequent removal of all pre- and paratracheal nodes, which otherwise would remain hidden behind the pretracheal fascia. The surgeon should be sure to introduce the scope with the blades completely closed. Exactly how the scope should be moved and advanced in the mediastinum depends on the type of spreadable scope used. The Linder-Dahan scope (Richard Wolf Co., Knittlingen, Germany) has a roof-shaped upper blade; therefore, it should be elevated repeatedly while being introduced in a very typical manner. The Hürtgen-Linder scope (Karl Storz GmbH, Tuttlingen, Germany) may be introduced more like a typical mediastinoscope
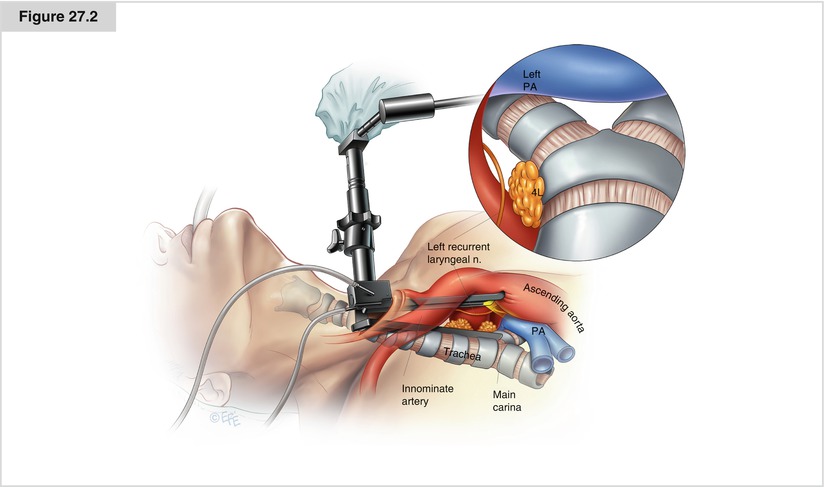
Figure 27.2
Exposure of the central airways, right pulmonary artery, and left recurrent laryngeal nerve; dissection of the left compartment. This step of the procedure is carried out with the scope closed, similar to the preparation technique used with conventional mediastinoscopy. The main carina and the upper part of the subcarinal region are crossed ventrally by the right pulmonary artery and must be completely separated from this vessel before any attempt is made to spread the blades. Otherwise, a partially fixed pulmonary artery might lacerate and cause potentially lethal bleeding. After the right and left tracheobronchial angles are identified, the axis of the scope is twisted to the left and with gentle longitudinal strokes leftward, the left recurrent laryngeal nerve is identified and exposed, thus preparing for the following step. In contrast to the other compartments, the left compartment should not undergo en bloc dissection if the function of the left recurrent nerve must be preserved. Instead, we suggest a thorough dissection of the adipose tissue with removal of all exposed lymph nodes. For the same reason, the use of electrocautery is not advisable. Thus, tissue unfeasible for blunt dissection must be cut with scissors and hemostasis assured with clips and hemostatic gauze. Twisting the scope to the left exposes the distal trachea and tracheobronchial angle. Now the scope may be opened and fixed to the holding device in an appropriate position for bimanual dissection. The fascia covering the left compartment is spread with a grasper or dissector between the left recurrent nerve and the airway or, if the nerve cannot be identified, next to the airway. Typically, the nodes lie dorsal to the recurrent nerve. Attention must be paid to the left pulmonary artery crossing the left main bronchus ventrally and further below. Dissection follows the compartment until it disappears between the trachea and ascending aorta. To remove the lymph nodes without causing bleeding and lymphatic leakage, the individual node is grasped and dissected bluntly out of the fatty tissue until the pedicle containing lymphatic and blood vessels is defined. Typically, one such pedicle containing a small artery crosses the recurrent nerve. It is very easy to put a clip on the pedicle tangential to the nerve, keep holding it with the clip applicator, and rip the node off
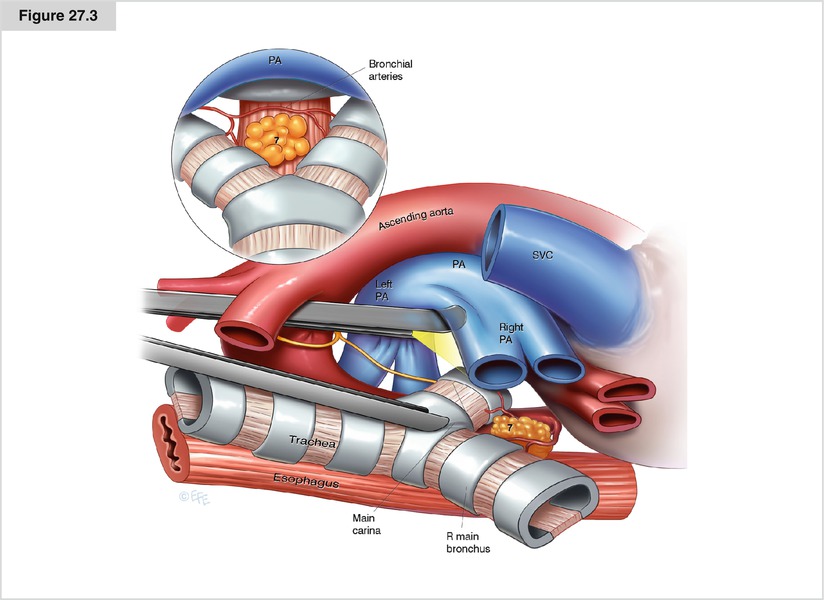
Figure 27.3
Dissection of the central compartment (Subcarinal Space). Loading the carefully dissected pulmonary artery onto the upper blade of the scope exposes the subcarinal space. Typically, if not dissected away from the tracheobronchial tree altogether with the pulmonary artery, the pretracheal fascia must be reopened to expose the subcarinal nodes. Dissection starts by separating the nodes from the medial surface of both main bronchi. Often, the subcarinal space is too wide to view both main bronchi at the same time through the scope. Then dissection starts either on the right or left side at the medial wall of the bronchus with the scope fixed in appropriate positions. The bronchial artery enters the compartment from the left side either above or underneath the left main bronchus or the carina. From there, it runs to the right main bronchus, with some variability with regard to its position in front of, between, or behind the subcarinal nodes; therefore, it often must be divided between clips. Coagulation alone may be ineffective (see section “Pitfalls and complications”). Next, the subcarinal specimen is pushed distally—not pulled into the scope—and dissected away from the anterior wall of the esophagus dorsally and the dorsal pericardium ventrally. The caudal margin of the specimen, by definition, should be 5 cm below the main carina. In practice, the dissection is carried as far as the instrument’s reach. It must be kept in mind that the operative field stretches distally to the open mediastinoscope to a depth of about 5 cm. In practice, the specimen ends distally shortly above or close to the right lower pulmonary vein and thus may include some right paraesophageal nodes, if not intentionally divided previously in upper and lower specimens. As a reference for radiology or subsequent resection of the primary tumor, this distal end of the VAMLA lymphadenectomy may be marked by one or two clips, which also avoids the need for electrocautery close to the lower pulmonary vein and the esophagus
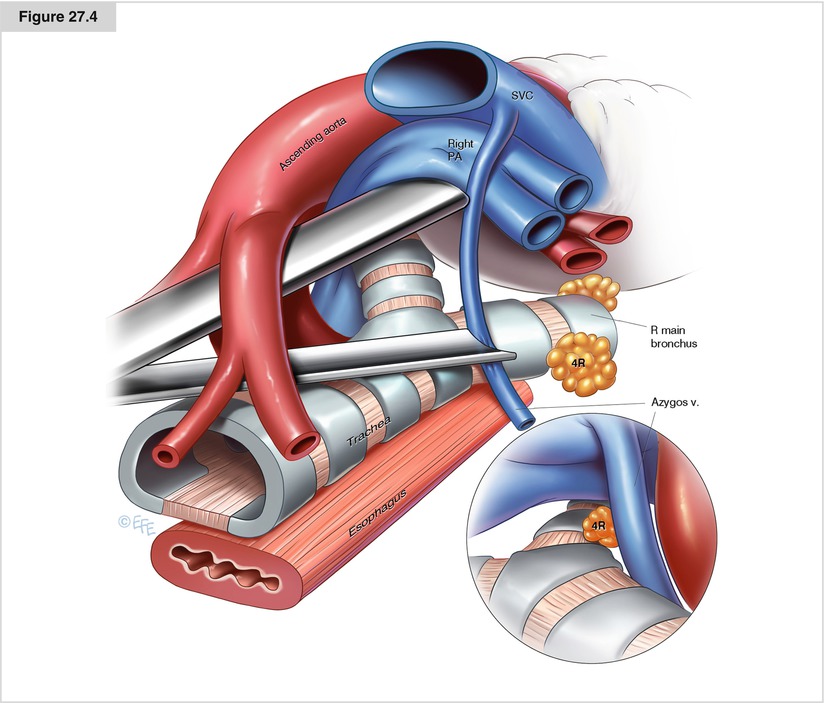
Figure 27.4




Dissection of the right compartment. The right is the largest compartment, and the scope must be repositioned repeatedly during dissection. To begin, the scope is directed toward the cranial part of the pretracheal fat pat dissected away from the innominate artery digitally at the beginning of the procedure. The scope is fixed at a position of 30–45° deviation from the tracheal axis to the right, and opened just into the adipose tissue. Thus, the fad pad initially obstructs the distal opening of the scope and must be pushed gently forward and downward, which will free the optic and expose the vena cava. Following that anatomic landmark, the fat pad is bluntly dissected away from the adjacent vessels, namely the innominate artery and vein, superior vena cava, and azygos vein, and from the right parietal pleura in a craniocaudal direction. Small veins draining into the vena cava should be clipped. After the azygos vein is reached, the specimen is either pushed leftward and caudally or pulled to the left to expose and divide under good visual control the last attachments to the right pulmonary artery and tracheobronchial angle distally to the azygos vein. In obese patients, the dimensions of the specimen may require its division, preferably proximal to or at the level of the azygos vein
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


