29 Ventricular Tachycardia
This chapter reviews the pathogenesis, diagnosis, and treatment of VT. SCD, which most commonly results from VT, is addressed in greater detail in Chapter 30.
Etiology and Pathogenesis
The type of VT, prognosis, and management of the arrhythmia are dependent on the presence of structural heart disease. The risk of sustained monomorphic VT is higher in patients with severe left ventricular (LV) dysfunction and extensive scarring. VT is also associated with myocardial ischemia, congestive heart failure, infiltrative cardiomyopathy, and high catecholamine states (Fig. 29-1). Any wide-complex tachycardia in a patient with a history of ischemic heart disease should be managed as VT until proven otherwise. In such a patient the mechanism is most often a reentry circuit in a region of healed myocardial infarction (MI). In these areas, gap junctions are often disrupted leading to slow and disorderly conduction by surviving cardiomyocytes. This physiology can lead to initiation and maintenance of reentrant circuits. Intracardiac recordings in the electrophysiology laboratory from the VT site of origin during sinus rhythm demonstrate fractionated low-amplitude electrograms that become continuous during VT. Sustained monomorphic VTs due to reentry can be reliably induced and terminated with ventricular programmed stimulation.
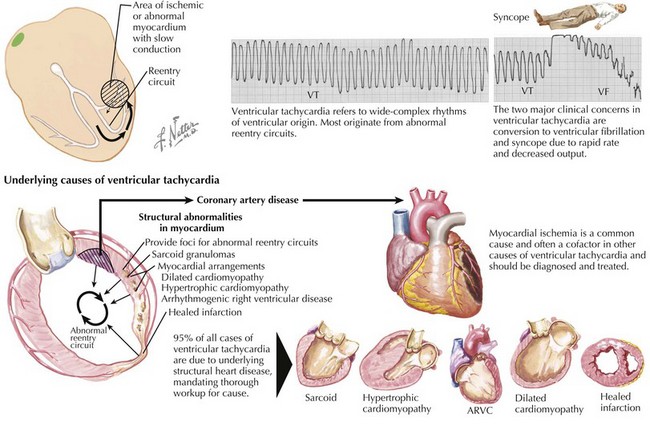
Figure 29-1 Mechanisms of ventricular tachycardia (VT).
ARVC, arrhythmogenic right ventricular cardiomyopathy; VF, ventricular fibrillation.
Differential and Ecg Diagnosis
QRS Morphology
If the QRS morphology changes during the tachycardia relative to baseline, then the diagnosis is probably VT. Intraventricular conduction is always abnormal in VT and results in broadening of the QRS. In general, the QRS duration is usually longer than 120 milliseconds in VT with the caveat that VTs originating from the His-Purkinje system can, on rare occasion, have a normal QRS duration. Wellens and colleagues (1978) found that approximately 70% of VTs have a QRS duration longer than 140 milliseconds in patients with a right bundle branch block pattern. VTs with a left bundle branch pattern generally have a QRS duration longer than 160 milliseconds. Generally, a VT with right bundle branch block morphology (predominantly positive QRS complex in lead V1) suggests an LV origin, whereas a VT with left bundle branch block morphology (predominantly negative QRS in lead V1) suggests right ventricular (RV) origin (Fig. 29-2A). VT with a right bundle branch block pattern will not have a typical RS wave. The R wave is single or biphasic (QR or RS) or triphasic (with initial R wave taller than the smaller r′ and an S wave in between that crosses the baseline). V6 typically demonstrates small r and large S waves. In VT with a left bundle branch block pattern, the duration of the initial R wave exceeds 30 milliseconds, and the beginning of the QRS to the nadir of the S wave exceeds 70 milliseconds. The S wave may be notched or slurred. Since SVT with aberration is due to a functional bundle branch block, the QRS should resemble a typical bundle branch block, and the S wave is neither notched or slurred. If V6 is used, a qS pattern suggests VT. Though sometimes useful, these findings have limited sensitivity and specificity.
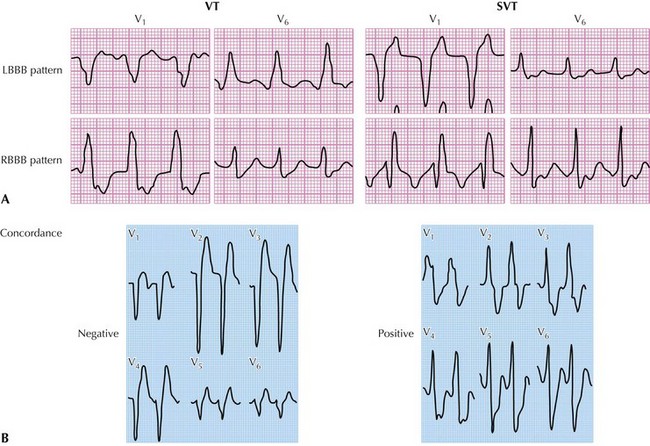
Figure 29-2 Changes in QRS morphology in ventricular tachycardia (VT) and in supraventricular tachycardia (SVT).
Change in the frontal plane QRS axis of more than 40 degrees, especially toward the “Northwest quadrant” between –90 and –180 degrees (normal is –30 to 90 degrees), is highly suggestive of VT. The presence of a qS pattern in lead V6 favors VT as a cause of wide-complex tachycardia. Concordance refers to uniform direction of the QRS complexes in the precordial leads, either all positive or all negative; for example, in VT with right bundle branch block pattern, the QRS is upright in all precordial leads (Fig. 29-2B).
Independent P-wave Activity
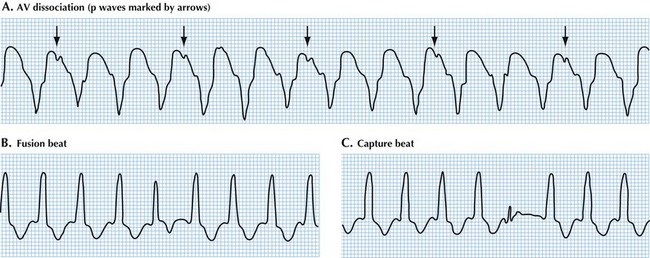
Atrioventricular (AV) dissociation indicates independent P-wave activity, and its presence is diagnostic of VT (Fig. 29-3A). The sinus rate is usually slower than the ventricular rate. The P waves should be upright in leads I and II if the origin is the sinus node. Variable deflections within the ST segment are suggestive of AV dissociation, and all 12 leads should be analyzed. AV dissociation can be difficult to discern, and its absence does not exclude VT, because the patient may have underlying atrial fibrillation (in up to one third of cases), or there may be retrograde ventricle-to-atrial conduction resulting in AV association in VT.
A fusion beat occurs when a sinus beat conducts to the ventricles via the AV node concurrent with a beat arising from the ventricles (Fig. 29-3B). The resulting QRS complex has an intermediate appearance between a normal beat and a VT beat. A capture beat occurs when the ventricle is depolarized via the AV node resulting in a narrow (normal-appearing) QRS (Fig. 29-3C). The presence of capture and/or fusion beats indicates AV dissociation and if present points to a diagnosis of VT. Their absence, however, does not exclude VT.
Additional Criteria
Two simplified approaches have been reported. One study used bundle branch pattern criteria and set VT as the default diagnosis (rather than SVT as in other criteria) and found a sensitivity of 96%. Another more recent algorithm has been reported that restricted ECG analysis to aVR (Fig. 29-4).
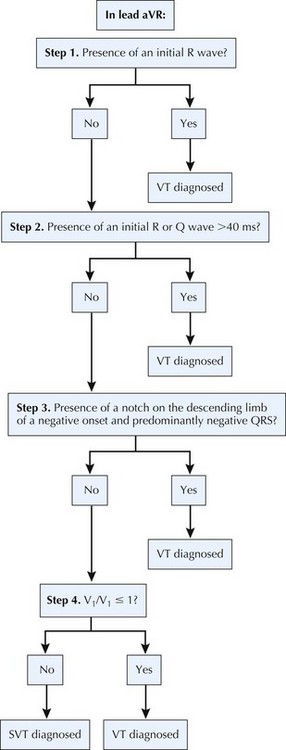
Figure 29-4 New aVR algorithm for diagnosing wide-complex tachycardia.
SVT, supraventricular tachycardia; VT, ventricular tachycardia.
Modified from Vereckei A, Duray G, Szénási G, et al. New algorithm using only lead aVR for differential diagnosis of wide QRS complex tachycardia. Heart Rhythm. 2008;5:89–98.
Diagnostic Approach
Some maneuvers may aid in differentiating SVT from VT in the hemodynamically stable patient. During an episode of tachycardia, carotid massage or Valsalva maneuver increases vagal stimulation and is most useful for tachyarrhythmias other than VT. Vagal stimulation can slow conduction over the AV node and thereby can terminate an AV nodal reentrant tachycardia or AV reentrant tachycardia, or unmask atrial flutter waves. Although the termination of a wide-complex tachycardia with intravenous adenosine favors a diagnosis of SVT with aberrancy, adenosine-responsive VT has been reported in patients with normal LV function and, thus, responsiveness to adenosine does not rule out VT. However, the idea that the absence of a response to adenosine rules in a diagnosis of VT is also a fallacy. The most common reason adenosine fails to terminate an adenosine-sensitive arrhythmia is that an insufficient dose reaches the heart before the drug is inactivated in the circulation. Moreover, adenosine can precipitate hemodynamic compromise in a patient whose condition is already tenuous and promote ventricular fibrillation (VF), and thus it should only be used with caution in a patient in whom VT is the most likely diagnosis (see Chapter 27).