Venous Thoracic Outlet Syndrome
LOUIS L. NGUYEN
Presentation
An 18-year-old right-hand dominant high school basketball player presents with acute swelling of his right arm. He has no other medical history. His vital signs are normal. On physical examination, he has a circumferentially enlarged right arm with prominent chest varicosities. He has palpable brachial and radial pulses bilaterally. No motor or sensory deficits are noted. He has no family history of clotting disorder.
Differential Diagnosis
Acute swelling in the arm most likely represents a deep venous thrombosis (DVT). When upper extremity DVT occurs in young, active persons, the cause is presumed to be effort thrombosis (Paget-von Schrötter syndrome), where structures of the thoracic outlet contribute to the stenosis and compression of the subclavian vein. Other causes of upper extremity DVT include the presence of intravenous catheters, external venous compression from trauma, and congenital or acquired hypercoagulable states, including malignancy. Most often, venous TOS (VTOS) occurs in the dominant arm, though nondominant VTOS can occur in persons who participate in bilateral arm sports (kayaking, swimming, weightlifting) or occupations (package handlers, retail shelf stockers).
Workup and Initial Treatment
Confirmation of the DVT and assessment of the extent of thrombosis can be made on venous duplex. Patients with acute DVT should be started on systemic anticoagulation unless otherwise contraindicated. A plain chest x-ray can evaluate for bony abnormalities, such as a cervical rib, a hypoplastic rib, and prior rib or clavicular fractures with a large bone callus. If the patient has symptoms of dyspnea or hypoxia, a computed tomography angiogram (CTA) of the chest can evaluate for pulmonary embolism.
In addition to prompt systemic anticoagulation, patients with VTOS should be considered for catheter-based thrombolysis of the DVT. This is performed via access of the basilic or cephalic vein in the upper arm under ultrasound guidance, followed by an attempt to cross the subclavian thrombosis and presumed stenosis with wires and catheters (Fig. 1). Successful mechanical and pharmacologic thrombolysis will reveal a stenosis at the proximal portion of the subclavian vein where the clavicle and first rib cross. Balloon angioplasty of the stenosis with a high-tensile strength balloon will help improve venous flow in the vein. Completion venograms in the arms-down and arms-up positions will demonstrate the dynamic compression of the vein at the thoracic outlet (Fig. 2). After successful thrombolysis, patients can be discharged on anticoagulation for subsequent VTOS decompression surgery after 2 weeks to allow for resolution of edema and inflammation.

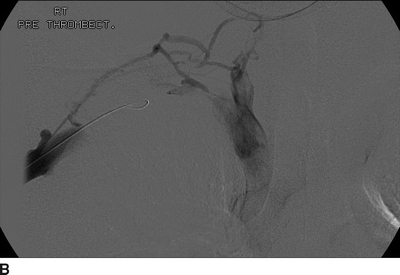
FIGURE 1 A, B:Initial subclavian venogram showing thrombosis.
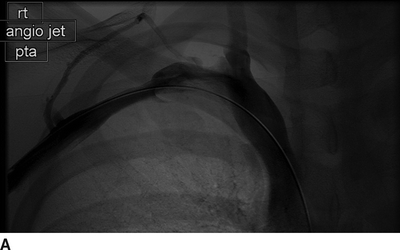

FIGURE 2 Subclavian venogram showing (A) patency in the arm-down position and (B) cessation of flow due to TOS compression in the arm-up position.
Surgical Approach
In order to access the supra- and infraclavicular spaces as well as the affected arm, the patient is placed in the semi-Fowler’s position (supine with back of bed up at 30 degrees) with the head turned slightly away from the affected side. The ipsilateral neck, anterior chest, and arm are prepped. A sterile arm sleeve is placed around the hand and forearm to allow for complete mobility of the arm.
A supraclavicular incision is made lateral to the sternal head of the sternocleidomastoid muscle (SCM) and carried through the platysma. The clavicular head of the SCM is divided to reveal the underlying internal jugular vein (IJV). The supraclavicular fat pad is mobilized laterally to expose the underlying anterior scalene muscle (ASM) and phrenic nerve. The phrenic nerve is carefully mobilized laterally to allow for circumferential dissection of the ASM insertion on the first rib. The ASM is sharply divided off the rib, and a 1- to 2-cm segment of the ASM is resected to reduce the chance of distal reattachment.
Next, the subclavian artery and roots of the brachial plexus are mobilized medially to expose the middle scalene muscle (MSM) as it attaches to the first rib. A periosteal elevator is used to lift the MSM off the rib, taking care to avoid the long thoracic nerve lying posterior and lateral to the MSM. The first rib is then cut at the MSM insertion site.
A medial infraclavicular incision is then made over the first rib and lateral to the sternal border. The dissection is carried down to the pectoralis fascia and then to the rib. A periosteal elevator is used to circumferentially free the rib from the surrounding intercostal muscles. The first rib is then divided just lateral to the sternal border and removed for inspection. The rib specimen should contain the subclavian artery and vein grooves as well as the costoclavicular ligament (Fig. 3). The proximal subclavian vein is mobilized, and any external fibrous bands are removed to allow the vein to fully fill. Care is taken to fully visualize the junction of the subclavian vein and IJV to assure that there is no longer any compression from a retained rib segment or fibrous scar.
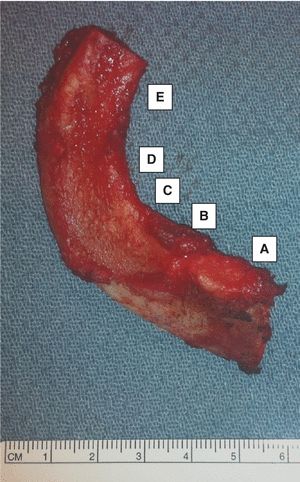
FIGURE 3 Right rib specimen with key landmarks (medial to lateral) (A) costoclavicular ligament, (B) subclavian vein groove, (C ) anterior scalene muscle insertion site, (D) subclavian artery groove, and (E ) middle scalene muscle insertion.



