Vena Cava and Central Venous Reconstruction
Audra A. Noel
Superior vena cava (SVC) and inferior vena cava (IVC) stenosis and occlusion may be caused by malignant disease, congenital disorders, iatrogenic or catheter-induced injury, chronic post-thrombotic disease, or external compression, such as mediastinal or retroperitoneal fibrosis. SVC obstruction can cause facial or cerebral edema, airway compromise, and orbital tissue swelling. IVC obstruction results in symptoms of lower-extremity venous hypertension that range from mild edema and varicose veins to massive swelling and ulcers.
Upper-extremity venous disease is less common and is typically caused by malignancy or catheter-induced injury. Lower-extremity disease due to obstruction or reflux is more prevalent, affecting up to 1% of the population, with nearly 164 of 1,000 people seeking medical care for lower-extremity venous disease. Venous leg ulcers are painful and debilitating, causing lost workdays and high medical costs. Patients are often noncompliant with elastic stockings, but even strict adherence to an effective nonoperative program will result in ulcer recurrence as high as 69% at 12 months.
Despite its significant social and economic consequences, venous obstruction is often considered less important than other vascular diseases. Fortunately, several groups have made active efforts to address the challenges of venous disease, including reconstruction of the central veins. This chapter reviews the principles of central venous reconstruction and the indications for intervention with either endovascular or open surgical techniques.
Principles
The decision to treat venous obstruction depends primarily on the severity of symptoms. Even in the face of complete central venous obstruction, collateral venous drainage often results in mild clinical symptoms that are unlikely to be improved with surgical intervention. The decision to treat must consider the duration of the symptoms, age of the patient, benign versus malignant disease, and hypercoagulability. In a patient with severe hypercoagulable disease and recurrent thrombosis, compressive therapy alone may be preferred, because percutaneous or open procedures have a significant failure rate in this patient population.
Functional and anatomic assessment should be performed before entertaining intervention. The gold standard of imaging is conventional venography, although computed tomography (CTV) and magnetic resonance venography (MRV) are improving rapidly. As with any vascular reconstruction, optimal inflow and outflow are required. For example, in patients with a chronically occluded femoral vein, an iliac stent alone may be ineffective and result in early stent failure. Often a combination of thrombolysis, stent placement, and open intervention provide the best long-term result. Long-term outcome of venous reconstructions and stents are based on data from small retrospectively analyzed case series. Thoughts about venous stents have been extrapolated from data on arterial stents. Precise knowledge of causes of failure, restenosis, or thrombosis after venous reconstruction therefore remains to be elucidated.
Pre-operative Classification, Noninvasive Studies, and Imaging
In order to assess patients for operative intervention of venous disease, accurate classification of venous disease must be performed. For SVC obstruction, patients should be classified according to the four groups described by Stanford and Doty in 1986 (Fig. 75-1). For the lower extremities, reporting standards in venous disease have been established by the International Consensus Committee on Chronic Venous Disease. Before being considered for intervention, each patient should be classified using the CEAP (Clinical, Etiologic, Anatomic, Pathophysiologic) system and the clinical severity scale based on pain, edema, venous claudication, skin changes, and ulceration. If present, ulcer size, duration, multiplicity, and incidence of recurrence after medical treatment should be documented. A thorough exam of the arterial system should be done, as venous and arterial diseases are not exclusive and arterial disease may contribute to poor healing of venous ulcers. Chronic nonhealing ulcers with unusual characteristics should be biopsied for evidence of malignancy.
A critical component of venous surgery is the use of noninvasive, functional studies to guide the surgeon in selecting the appropriate intervention. Severe chronic venous insufficiency may be due to primary valvular incompetence in superficial, deep, or perforator veins or secondary to deep venous thrombosis (DVT). Physiologic tests that have been described to assess the etiology of venous hypertension include foot volumetry, photoplethysmography, ambulatory venous pressure measurements, air plethysmography, and strain-gauge plethysmography. In our practice, we use strain-gauge plethysmography to identify abnormalities in calf muscle pump function, venous incompetence, and outflow obstruction. In addition, duplex ultrasonography is done to map venous anatomy and evaluate patency and competency in the deep, superficial, and perforating veins. It is imperative that venous reflux, valvular incompetency, and obstruction all
be considered prior to intervention for venous hypertension.
be considered prior to intervention for venous hypertension.
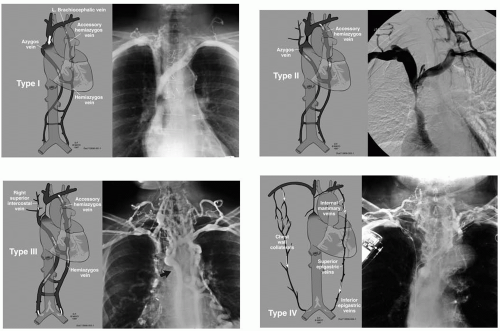 Figure 75-1. Diagrams of the four classifications of SVC obstruction based on contrast venography as originally defined by Stanford and Doty in 1986. |
As noted above, venography is the gold standard of venous imaging when evaluating a patient with obstruction with the intent to intervene. Often percutaneous intervention can be accomplished during the same procedure. However, when planning more complex interventions, CTV and MRV are rapidly becoming detailed enough to use in surgical planning (Fig. 75-2). One clear advantage of a contrast study is the ability to assess venous incompetence with a descending venogram and the ability to measure venous pressure gradients, as well as better imaging of collateral veins. At present, a patient with a straightforward history of chronic obstruction is most efficiently imaged with ultrasound followed by venography with potential concomitant intervention, whereas a patient with a complicated history would be imaged first with CTV or MRV.
Indications
More than 75% of patients with SVC syndrome have malignant disease, including primary and metastatic mediastinal or intrathoracic tumors. In this group, where the patients are often terminally ill, percutaneous intervention is employed as a means of improving quality of life. Even a short duration of improvement is very helpful in such patients. Intervention relieves facial swelling, improves airway control, and decreases massive upper-extremity edema.
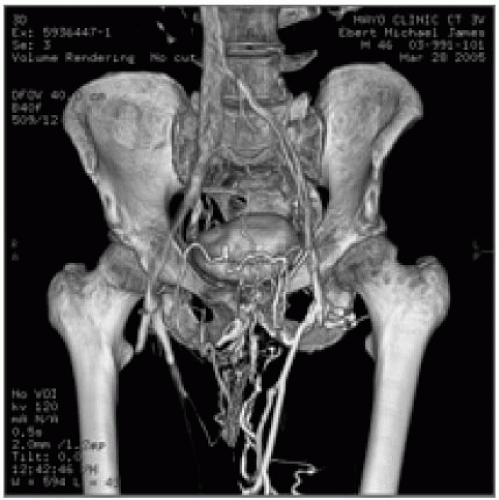 Figure 75-2. 64-Scanner computed tomography of left iliac venous obstruction demonstrating extensive suprapubic collateral veins. |
Many patients with benign disease have mediastinal fibrosis. In addition, increasingly larger proportions have thrombosis caused




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


