Figure 11.1
Patient positioning and port distribution for conventional three-port VATS wedge resection. With the patient in the lateral decubitus position, the target area in the lung is placed at the vertex of an ideal “baseball diamond” configuration. Opposite the target area is the port for the videothoracoscope, and lateral are the operative ports through which the endograsper and endostapler can be inserted
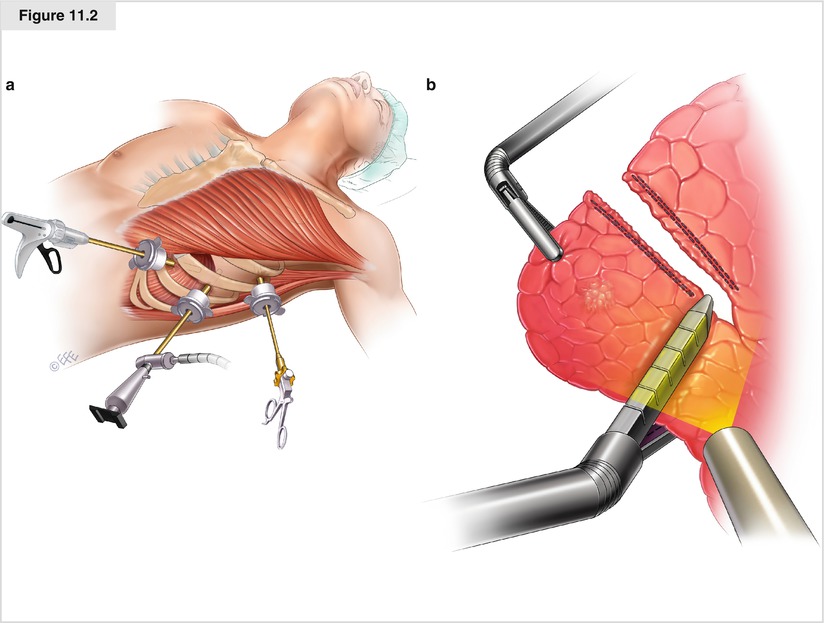
Figure 11.2
(a) Alternative port placement with the patient supine. (b) Thoracoscopic view of the anteroposterior approach to the parenchyma to be resected. The ring forceps grasp the lung on one side while the endostapler is placed from the opposite side
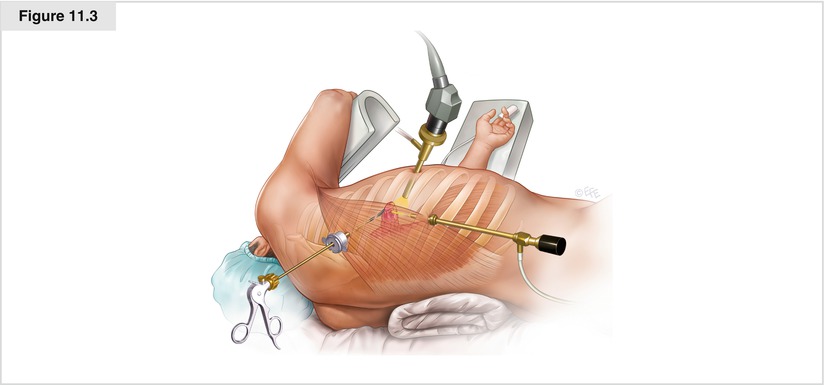
Figure 11.3
Patient positioning and port placement for VATS laser wedge resection
Technical Variants of the Conventional VATS Wedge Resection Technique
Prompted by scattered reports that the level of invasiveness offered by conventional VATS procedures is not as limited as presumed, especially with regard to chronic pain, as well as reports of the technical pitfalls intrinsic to a thoracoscopic approach compared with open surgery (e.g., lack of palpation), several alternatives to conventional three-port VATS wedge resection have emerged in the recent literature.
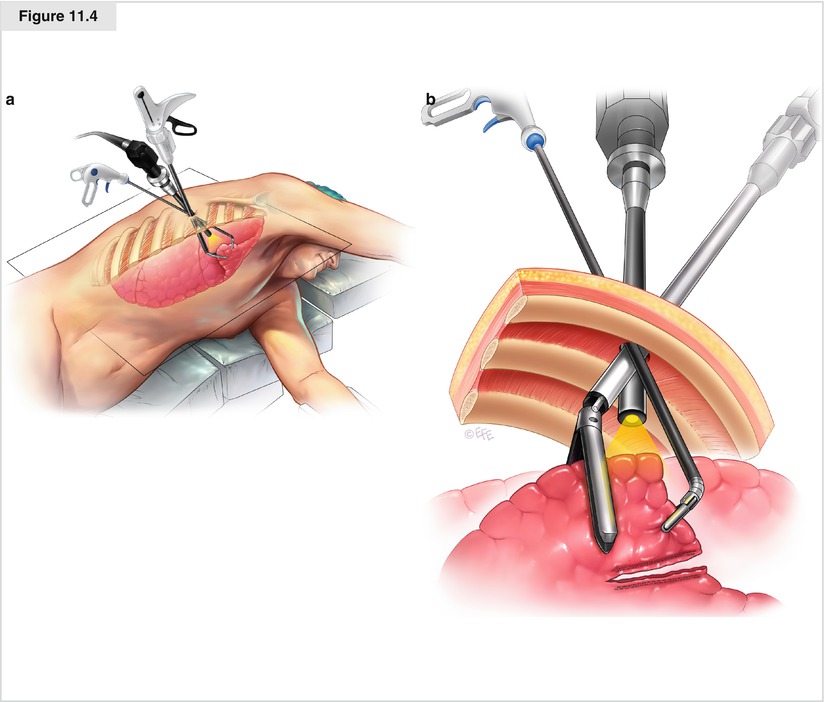
In particular, single-access (uniportal) VATS wedge resection has been proposed as a completely different surgical philosophy that takes advantage of current technologic innovations, such as articulating endoscopic instruments, and awake-patient anesthesia (Rocco et al. 2010). The uniportal technique involves the sequential insertion through the same 2- to 2.5-cm long incision, together with the 5-mm 0° or 30° videothoracoscope, of articulating endograspers and endostaplers that address the target area to be resected according to a craniocaudal (i.e., sagittal, not anteroposterior) line (Fig. 11.4a, b) (Rocco et al. 2010). There are obvious similarities to the open technique, as the surgeon manipulates the lung and performs the subsequent resection the same way he or she normally would during thoracotomy. This is possible because deployment of the articulating arms of the operative instruments occurs away from the target area, thereby increasing intrathoracic maneuverability. In turn, this advantageous spatial distribution of the instruments helps avoid interference because the stems of the operative instruments are kept sideways along the single incision, taking full advantage of the laterality of the incision itself. Hence, compared with conventional three-port VATS, the uniportal approach does not impinge on multiple intercostal bundles.
Another technique addresses the lack of palpation with conventional VATS wedge resection, especially when used for pulmonary metastases. Several authors (especially Mineo and Detterbeck) have proposed a hand-assisted VATS wedge resection aimed at coupling minimal invasiveness and maximal accuracy in detecting pulmonary nodules. From a surgical standpoint, the innovative point resides in the creation of a substernal tunnel to accommodate the surgeon’s hand, which therefore can palpate both lungs at the same time (Pfannschmidt et al. 2007).