Vascular Tumors and Anomalies
Ahmad I. Alomari
Introduction
Vascular anomalies are relatively common heterogenous disorders characterized by developmentally abnormal blood vessels including the venous, arterial, and lymphatic lineages. These anomalies may overlap clinically and radiologically creating considerable confusion in the clinical practice and published research. Nevertheless, the diagnosis and management of the vast majority of vascular anomalies fundamentally can be simplified if the proper nomenclature and classifications are applied. Commonly used inaccurate terms, such as lymphangioma, cystic hygroma, cavernous hemangioma, strawberry hemangioma, hemangiolymphangioma, and cavernoma should be abandoned for the more representative designation.
The binary classification proposed by Mulliken and Glowacki in 1982 (1) divides vascular anomalies into two major categories: (1) vascular tumors and (2) vascular malformations. Vascular malformations can be either of the slow-flow (venous, capillary, and lymphatic) or fast-flow type (namely, arteriovenous malformations [AVMs] and fistulas). The correct diagnosis and appropriate therapy require proper awareness of the clinical and imaging features of different types of vascular anomalies. Improper terminology can lead to the wrong diagnosis, mistreatment, and misdirected research efforts (2).
Unfortunately, terminology imprecision is still prevalent in the published literature. “Hemangioma,” according to Hassanein et al. (3) was used incorrectly in 228 of the 320 publications (71.3%) studied. The authors also demonstrated that inaccurate designation of the vascular anomaly was associated with an increased risk of erroneous management.
Embryology and Genetics
The embryonic vascular network primarily is created via two major, distinct mechanisms: vasculogenesis and angiogenesis (4,5). The differentiation and growth of blood vessels from hemangioblasts of mesodermal origin to form the heart and the primitive vascular plexus is called “vasculogenesis,” while the subsequent process of remodeling and expanding this network is referred to as “angiogenesis” (6). The distinction between arteries and veins is an early developmental process (7) with molecular differences between arterial and venous channels prior to the establishment of the circulation (8,9).
Due to the extensive, complex biologic pathways involved in the formation of normal blood vessels, developmental anomalies of the vasculature (both idiopathic and caused by specific defects) frequently are seen.
Most vascular anomalies are sporadic with no identifiable familial or genetic predisposition. Nevertheless, specific mutations have been identified for many vascular anomalies and syndromes. Inherited disorders of vessels include hemorrhagic telangiectasia (HHT, ENG, ALK1, or SMAD4 mutations), capillary malformation–arteriovenous malformation (CM-AVM, RASA1 mutation), cutaneomucosal venous malformation (VMCM, TIE2 mutations), glomuvenous malformation (GVM, GLOMULIN mutation), PTEN hamartoma tumor syndromes (PTEN mutation), ataxia-telangiectasia (ATM mutation), cerebral cavernous malformation (CCM, CCM1–4 mutations), primary congenital lymphedema (Milroy disease, VEGFR3 mutation), among others (10). Recently CLOVES syndrome has been shown to result from a PIC3CA mutation.
Several sporadic, complex syndromes are known to be associated with fast-flow vascular anomalies. Parkes Weber syndrome and CLOVES syndrome, two rare overgrowth syndromes, are associated with AV shunts and hypervascularity. AVMs and fistulas also have been reported in Noonan syndrome (11), Ehlers–Danlos syndrome (12,13), VACTERL association and fibromuscular dysplasia (14), and liver hemangioma (15). Infantile hemangioma (IH) and rapidly involuting congenital hemangioma (RICH) are probably the most vascular pediatric tumors and occasionally can be associated with arteriovenous shunts. For instance, hepatic RICH is typically a large solitary mass and might be associated with various types of transhepatic vascular shunts and high-output heart failure (16).
Classification
The well-known classification of vascular anomalies, proposed by Mulliken and Glowacki (1), divided vascular anomalies into two distinct types: tumors and malformations. The differentiation is based on clinical, histopathologic and imaging differences (Table 37.1).
IHs, the prototype of vascular tumors, are common endothelial tumors that present in early infancy and spontaneously involute later in childhood. Congenital hemangiomas, a less common lesion, are present at birth. Endothelial cell tumors also include a spectrum of uncommon hemangioendotheliomas (such as kaposiform hemangioendotheliomas [KHEs] and epithelioid hemangioendotheliomas) and angiosarcoma.
Vascular malformations are typically present at birth and grow with the patient. Based on the cellular lineage and flow pattern, malformations are divided into slow-flow (including venous malformations [VMs], lymphatic malformations [LMs], capillary malformations [CMs] or combined malformations) and high-flow malformations (AVMs and arteriovenous fistulae [AVF]). Finn et al., described 375 pediatric vascular anomalies (17); 96% of these lesions were classified as either tumors or malformations.
Clinical Manifestations and Treatment
Vascular Tumors
Infantile Hemangiomas
Infantile Hemangiomas (IHs) are the most common tumor of infancy. They present at birth or in the first few months of infancy
in 4% to 5% of children (18). IH is not fully developed at birth, though earlier signs (such as faint macular or telangiectatic stain) may herald the definitive manifestation of the lesion. Typically, IHs undergo rapid growth (proliferative phase) over a few months then regress spontaneously over years (involuting phase). IH, like many other vascular anomalies, have a predilection to affect the cervicofacial region. The lesions are known to disproportionately affect Caucasians, females, and premature infants. Histologically, IH show lobules and sheets of tightly packed, mostly capillary-sized vascular channels.
in 4% to 5% of children (18). IH is not fully developed at birth, though earlier signs (such as faint macular or telangiectatic stain) may herald the definitive manifestation of the lesion. Typically, IHs undergo rapid growth (proliferative phase) over a few months then regress spontaneously over years (involuting phase). IH, like many other vascular anomalies, have a predilection to affect the cervicofacial region. The lesions are known to disproportionately affect Caucasians, females, and premature infants. Histologically, IH show lobules and sheets of tightly packed, mostly capillary-sized vascular channels.
TABLE 37.1 Classification of Vascular Anomalies | ||||
|---|---|---|---|---|
|
The tumor initially manifests as a well-marginated reddish-purple lesion with variable size, shape, and depth of tissue involvement (Fig. 37.1). Superficial hemangiomas are limited to the skin and subcutis. Deep lesions affect the subcutis and adjacent anatomical spaces; typically sparing the skin and bone. Combined (deep and superficial) and multiple IH are not uncommon. These also can be solitary (focal) or multiple (multifocal) tumors. IHs are usually rubbery, warm, and can be pulsatile.
In most patients with IHs, no treatment is necessary because most lesions regress over years without residual scarring (18). Nevertheless, complications of hemangiomas, such as ulcers, bleeding, amblyopia (periorbital), airway obstruction (subglottic), and heart failure (liver) require prompt intervention (19,20).
 Figure 37.1 Infantile hemangiomas of the face. The raised, well-marginated reddish lesions have superficial (cutaneous) and deep portions. |
The combination of posterior fossa malformations, cervicofacial hemangiomas, arterial anomalies, cardiac defects, eye anomalies, sternal clefting, and supraumbilical raphe, are referred to as “PHACES” Association (21).
Congenital Hemangiomas
Congenital hemangiomas are present and fully mature at birth. Rapidly involuting (RICH) and noninvoluting congenital hemangioma (NICH) demonstrate marked similarities in appearance, location, and size with equal sex ratio (24). RICHs regress in the first year of life while NICH persists. Glucose transporter protein (GLUT1), an immunohistochemical marker for IH, is not expressed in congential hemangioma (25,26).
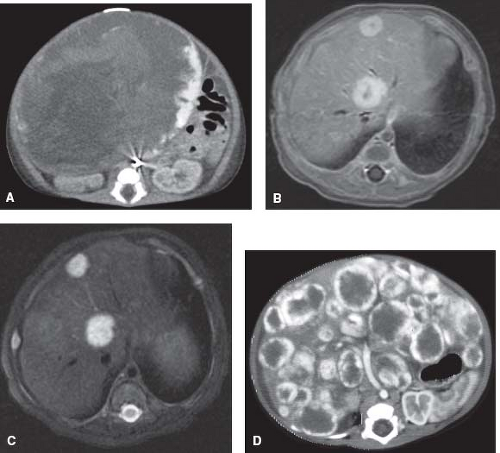
Liver hemangiomas represent a spectrum of lesions with variable clinical and imaging features. The large, solitary liver hypervascular tumors are RICHs while the multifocal and diffuse types are histopathologically IH (Fig. 37.2) (27). Hepatic hemangiomas typically are asymptomatic. However, they can cause high-output
cardiac failure, liver dysfunction, hypothyroidism, coagulopathy, and abdominal compartment syndrome.
cardiac failure, liver dysfunction, hypothyroidism, coagulopathy, and abdominal compartment syndrome.
KHE is an infiltrative tumor with clinical and imaging features distinct from IH. KHE typically is present at birth or appears shortly thereafter in early infancy, though it rarely can develop in adults. Histologically, KHE is characterized by a predominant Kaposi sarcoma-like, fascicular spindle cell growth pattern of epithelial cells, infiltrating nodules with slit-like or crescentic vessels that are poorly canalized (27). The tumor presents clinically with thickened, purple-ecchymotic skin discoloration (Fig. 37.3). Extensive KHE commonly is associated with Kasabach–Merritt phenomenon (KMP) with platelet entrapment within the tumor leading to severe thrombocytopenia (28). KHE, unlike IH, is a locally invasive solitary lesion, which affects both genders equally and has predilection to the trunk, extremities, retroperitoneum, head, and neck (27).
Imaging of Vascular Tumors
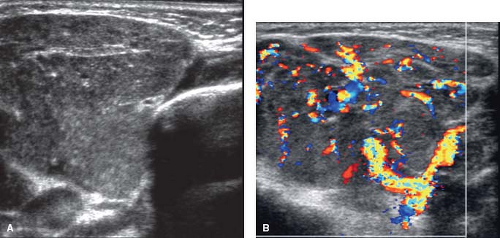
Ultrasonography is the initial, simple and reliable imaging modality for many vascular tumors. For IH, ultrasound images typically depict a solid, hypervascular mass with well-defined margins
(Fig. 37.4). The feeding arteries and draining veins are enlarged. The former will display a low-resistance arterial spectral waveform.
(Fig. 37.4). The feeding arteries and draining veins are enlarged. The former will display a low-resistance arterial spectral waveform.
 Figure 37.3 Kaposiform hemangioendothelioma. Irregular patch of purple-ecchymotic skin thickening with overgrowth of the right thigh. |
Magnetic resonance imaging (MRI) is superior to CT scan for demonstrating the characteristic features of hemangiomas. Both modalities show well-defined, lobulated solid masses with homogeneous enhancement following contrast administration. The tumor demonstrates homogeneous low or moderate intensity on T1-WI and high intensity on T2-WI MR images. Flow voids within or around the lesion are caused by the dilated feeding arteries and draining veins (Fig. 37.5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree