Figure 19.1
In about 70 % of cases, a vascular sleeve resection is done for tumors of the left upper lobe, which is shown here. The patient is placed on his or her right side, and an anterolateral thoracotomy is carried out in the fourth intercostal space. In rare cases, the tumor involves only the interlobar part of the PA; in these cases, the main PA may be prepared extrapericardially. However, in most instances, the tumor also infiltrates the central part of the PA, so the pericardium must be incised longitudinally and dorsal to the phrenic nerve to allow examination of the intrapericardial situation. If the central part of the PA seems to be free, the procedure may proceed by mobilization of the whole lung and dissection of the aortopulmonary window. Special caution must be used in preparing the vagus nerve to avoid damaging the recurrent nerve. Although in most instances the lower pulmonary vein can be encircled extrapericardially, the upper pulmonary vein usually is involved and must be dissected intrapericardially. After that, the central part of the PA has to be dissected completely. In most instances, the ductus Botalli must be divided. If the tumor infiltrates the artery very proximally, the posterior aspect of the vessel invariably is dissected blindly. This must be done very carefully to avoid damage to the right part of the PA. Once the PA has been encircled, a tourniquet may be applied and the flow to the left lung reduced. However, complete clamping at that time should be avoided because the interfissure part of the artery can be prepared much more easily if there is still some flow through the vessel. Before the interfissure part of the artery is dissected, the lung has to be mobilized also in the area of the mainstem bronchus. The lymphadenectomy should be completed in the paraesophageal and bifurcation regions, including the number four lymph nodes. Before proceeding with the operation, it should be clear that a pneumonectomy is technically possible if needed as rescue surgery. If this is clear, the interfissure part of the PA may be dissected. After dissection of the interlobar lymph nodes, the superior segment artery of the lower lobe should be prepared first, followed by the artery for the basal segment. After the interfissure part of the artery has been encircled, the lower lobe bronchus, as well as the mainstem bronchus, also should be encircled. For a better overview of the PA, at this point the upper lobe vein should be transected, followed by transection of the bronchus. In most instances, a bronchial sleeve resection also is necessary. Therefore, the lower lobe bronchus and the mainstem bronchus should be cut at an appropriate level. After that, the PA is visible at the complete course and may be prepared further. Depending on the area of tumor infiltration, it may be possible to dissect the arteries of the more apical segments of the upper lobe or, in other instances, those of segment 4 or 5. This facilitates the ensuing reconstruction of the PA. At this point, 2,000–4,000 U of heparin should be given, depending on the patient’s weight. The central part of the PA is clamped by either a Satinsky or long, curved aortic clamp. Clamping of the distal part of the PA should be avoided. Instead, backflow from the lower lobe is controlled by encircling the lower lobe vein and applying a tourniquet; the advantage to this is that no additional clamps are within the operative field. Next, the PA is dissected at an appropriate level and frozen section examinations are performed on the bronchial resection site as well as on the vascular part
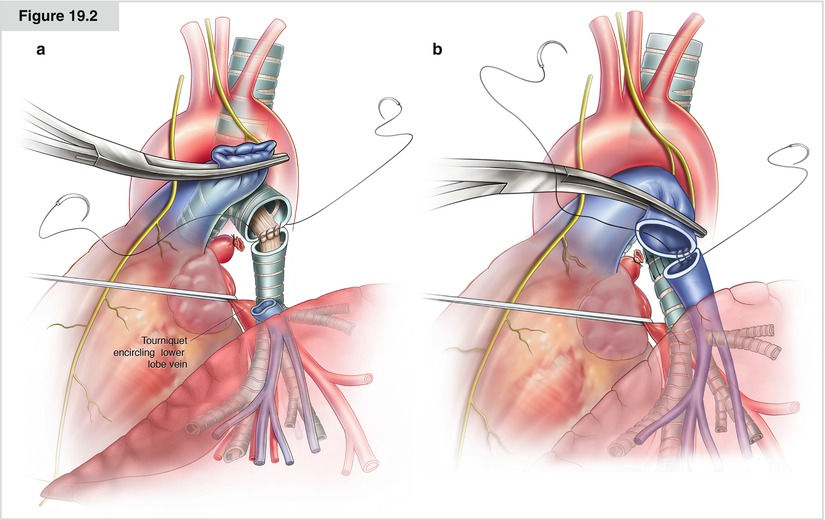
Figure 19.2




(a, b) In the case of double resection, the bronchial anastomosis is performed prior to the reconstruction of the PA. This minimizes the manipulation of the vessel; in addition, exposure of the bronchial stump is optimal if the artery is divided. When reconstructing the PA, special attention should be given to even margins on both sides of the vessels, even if the vessel has to be shortened further. This facilitates proper placement of the stitches, and it helps to have an uneven inside lumen. The anastomosis is performed by running 5-0 monofilament nonabsorbable sutures from the posterior to the anterior part while lifting the lower lobe gradually to avoid tension on the sutures. If the distance between the arterial stumps is deemed excessive, the interposition of a prosthetic conduit is mandatory. In most instances, the caliber discrepancy between the two sides of the anastomosis is no problem because of the elasticity of the vessel wall, which helps at this stage
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


