Chapter 17
Vascular Laboratory
Venous Physiologic Assessment
Brajesh K. Lal
Chronic venous insufficiency (CVI) of the lower extremity is most often characterized by venous hypertension caused by valvular reflux, obstruction, or a combination of both.1 Just as in the treatment of arterial disease, appropriate management of venous disease is predicated on accurate assessment of the anatomic abnormality and the physiologic impact of the disease. The development of therapies for patients with CVI was historically hampered by inadequate tools for objective clinical and noninvasive anatomic and hemodynamic evaluation of the venous system.
Currently available clinical and laboratory evaluations address the physical findings, underlying etiology, anatomic distribution, and mechanism of disease. The results of these evaluations provide the essential elements of the clinical, etiologic, anatomic, pathologic (CEAP) classification detailed in Chapter 55.2 Introduction of the CEAP classification system has advanced the evaluation of CVI from a subjective clinical impression based on physical examination alone to a more objective process similar to that followed for arterial disease.
As B-mode imaging technology has improved, it has assumed an important role in the anatomic diagnosis of CVI. By using the techniques outlined in Chapter 18, physicians can gain extensive knowledge of the anatomic sites and extent of disease with B-mode imaging noninvasively. Furthermore, the increasing sophistication of Doppler waveform analysis enables assessment of certain local physiologic measurements, such as the extent of segmental reflux. Many physicians base their clinical decisions on this combination of B-mode and Doppler waveform information (duplex ultrasonography) alone. However, duplex ultrasonography cannot define the importance of anatomic abnormalities in the context of global venous function of the limb.3 Clearly, one patient with gross reflux in the saphenous vein may have no resultant symptoms, whereas another patient may have an active ulcer. An objective measurement of the hemodynamic performance of the lower extremity venous system would greatly improve our ability to evaluate patients and recommend treatment.
Several noninvasive techniques are available to evaluate the global hemodynamic function of the venous system. However, they have not gained widespread use. The same considerations that exist in arterial disease are important in the diagnosis of CVI and assessment of treatment efficacy.4,5 Furthermore, for clinical research on the treatment of venous disease, hemodynamic evaluation should and will progressively become an important expectation in reporting standards.
This chapter focuses on methods of evaluating the hemodynamic significance of CVI. It details the instrumentation, techniques, interpretation, accuracy, and limitations of these tests. It also offers a perspective on appropriate clinical situations in which each test may provide clinically relevant information.
Ambulatory Venous Pressure
Venous insufficiency most often results in elevated venous pressure and may be due to the net result of outflow obstruction, valvular incompetence, arteriovenous malformations, or any combination of these conditions. Pollack and Wood6 first described venous pressure changes in 1949, when they noted that muscle contraction increased the outflow of blood from the lower extremities during exercise, thereby lowering venous pressure. They also documented the gradual return to resting venous pressure when the activity ceased. When Arnoldi et al7 demonstrated that variations in venous pressure in the superficial venous system reflected those in the deep venous pathways, their study validated the use of a dorsal foot vein for the evaluation of venous hemodynamics.
The sum of the hemodynamic factors involved in venous insufficiency can be quantified by the measurement of ambulatory venous pressure (AVP). AVP is defined as the venous pressure in a dorsal foot vein after 10 tiptoe maneuvers in a standing position. Most physicians consider AVP the “gold standard” measure of venous hemodynamics.8,9
Technique
To measure AVP, a catheter or butterfly needle is placed in a dorsal pedal vein and connected to a pressure transducer, and baseline standing pedal venous pressure is recorded. The patient then performs 10 tiptoe maneuvers at a rate of 1 per second to empty the calf veins and returns to the standing position. The pressure recorded at the end of the tiptoe maneuvers is defined as AVP. Refill time is measured as the time required to return to 90% of baseline venous pressure after cessation of calf muscle contraction.
Interpretation
In normal subjects, standing venous pressure is approximately 90 mm Hg (depending on their height). During exercise it should fall to approximately 30 mm Hg, and after exercise it should rise slowly back to standing pressure. Usually, 90% of baseline pressure is achieved in about half a minute (Fig. 17-1A). There are a number of possible abnormal results. The pressure may not fall normally during exercise, which indicates that the calf pump is not working effectively (Fig. 17-1B). AVP may return to the standing pressure too quickly, which would indicate reflux in the deep or superficial veins (see Fig. 17-1B). Pressure may also rise rather than fall during exercise, which indicates that the deep veins are occluded.
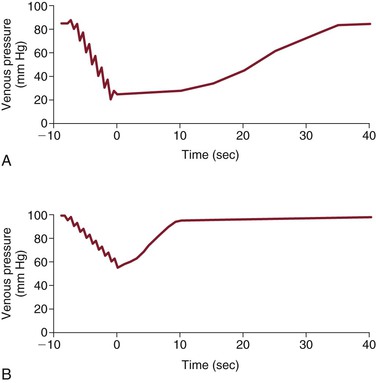
Figure 17-1 A, Tracing of ambulatory venous pressure (AVP) in a normal subject. Note the rapid fall in pressure during 10 calf contractions, indicative of good venous outflow and calf muscle pump function. Also note the slow rise to baseline pressure on completion of the calf contractions, indicative of absence of venous reflux. B, Tracing of AVP in a patient with chronic venous insufficiency. Note the higher baseline pressure, slow fall in pressure with tiptoe maneuvers, and high pressure on completion of the contractions, indicative of venous outflow obstruction and poor calf muscle pump function. Also note the rapid rise to baseline on completion of the calf contractions, indicative of severe venous reflux.
A higher AVP is generally indicative of more severe CVI. Nicolaides et al8 correlated AVP values to the incidence of limb ulceration and severity of CVI and showed a progressive increase in the incidence of skin ulceration as the mean values of AVP increased. They also reported differences in the AVP based on the anatomic pattern of venous reflux. Patients with deep venous insufficiency had higher AVP than did those with superficial insufficiency. Perforator incompetence and outflow obstruction also increased AVP, with the highest AVP reported in patients with deep valvular incompetence and proximal obstruction.
Accuracy
Overlap can exist between the AVP values of normal limbs and those with varying clinical categories of CVI. Up to 25% of patients with ulceration can have AVP values within normal limits.8,10 The use of tourniquets to occlude the superficial venous system during the study may help define the contribution of the superficial and perforator veins to refill time. In theory, a thigh tourniquet should occlude reflux occurring in the superficial system. If AVP and refill time correct after tourniquet application, the superficial system is probably the primary source of abnormal function. A lack of correction implicates the deep venous system. However, this aspect of the test has not proved to be reliable,11 and AVP should not be routinely used to identify the differential contribution of the deep and superficial systems to global venous hemodynamic dysfunction.
Limitations
Although AVP is generally perceived to be the gold standard measure of venous function, there is concern that pressure at the pedal vein may not accurately reflect changes in venous pressure within the leg, particularly in the deep venous system.12 Furthermore, it is an invasive and time-consuming procedure that may be difficult to perform in many patients, particularly those with active ulcers. Severe edema or dermal thickening and inflammation often accompany advanced CVI and may obscure the pedal veins, and thus, make access difficult. Therefore, it has been largely supplanted by techniques that measure venous hemodynamics noninvasively. These techniques also depend on a protocol of calf contraction and rest, much like the one used for measurement of AVP.
Plethysmography
Plethysmography is a noninvasive method of estimating changes in volume in an extremity.13 Because all other tissues maintain constant volume during the short period of testing, any recorded volumetric differences reflect changes in blood volume. Several plethysmographic techniques with different sensors have been used to measure changes in blood volume in a limb, including strain-gauge plethysmography (SGP), impedance plethysmography (IPG), photoplethysmography (PPG), and air plethysmography (APG).
These tests rely on the fact that the lower extremity veins are not filled to maximum capacity when the patient is in the supine position. With positional changes or when outflow is occluded by a pressure cuff, the venous system can accommodate increased volume before reaching maximal venous capacitance. With subsequent rapid positional changes or release of an externally inflated pressure cuff, patients with normal outflow exhibit rapid emptying of their lower extremity veins. These tests now routinely use an occlusion cuff, which has increased standardization by avoiding active patient movement and positional changes.
Positioning of the patient is critical in these tests. The patient is placed supine with the leg elevated 20 to 30 degrees on a soft heel support to enable venous drainage. The knee is flexed 10 to 20 degrees to prevent obstruction of popliteal vein outflow. The plethysmographic sensor is applied, and a thigh occlusion cuff is inflated to above venous pressure (50-60 mm Hg) and maintained until limb volume increases to a stable level. The cuff is then released rapidly to allow the tracing to return to baseline readings (Fig. 17-2A). The rise in the recording to the plateau during cuff inflation measures calf venous volume (VV), whereas the fall in the recording after rapid deflation measures venous outflow (VO). The rate at which this outflow occurs is inversely proportional to the resistance to VO. In the presence of VO obstruction or venous insufficiency, VV and VO are reduced (Fig. 17-2B).
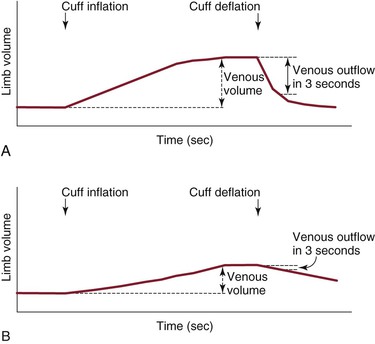
Figure 17-2 A, Representative plethysmographic tracing in a normal subject during inflation and deflation of proximal thigh occlusive cuff. B, Representative plethysmographic tracing in a patient with chronic venous insufficiency. Note the significantly reduced venous outflow recorded during the 3 seconds after cuff deflation (3-s venous outflow) indicative of severe venous outflow obstruction. The slope of the outflow curve (maximum venous outflow) is also reduced in comparison to the normal tracing in A.
Strain-Gauge Plethysmography
SGP is designed to detect changes in calf volume after inflation and then rapid deflation of a thigh occlusion cuff. A change in calf volume stretches a mercury-filled Silastic conductor tube (Dow Corning Corporation, Midland, Mich) with a proportional change in its resistance, which results in a corresponding change in voltage output signal. SGP provides an estimate of VO obstruction and has primarily been used in the past for the diagnosis of deep venous thrombosis (DVT). Although estimates of VV have not proved to be reliable diagnostic indicators of DVT, an estimate of VO in the form of maximal venous outflow (MVO) provides improved sensitivity.14 Barnes et al15 reported that MVO had a sensitivity of 90% for above-knee DVT, but only a sensitivity of 66% for below-knee DVT, whereas its overall specificity was 81%. Successful recordings from SGP require full cooperation from the patient. It cannot be performed on patients who are unable to lie flat. Prolonged recumbency, muscle wasting, and cardiac failure may result in measurement errors. Patients with limb injuries, bandages, casts, or severe edema are unsuitable candidates for SPG. Its use has been largely supplanted by duplex sonography.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


