Chapter 62 Vascular Compression Syndromes
Thoracic Outlet Syndrome
Thoracic outlet syndrome (TOS) describes a broad spectrum of symptoms and signs all related to compression or injury of the key anatomical structures that traverse this narrow aperture on their way to the upper extremity. This syndrome manifests in three main forms on the basis of the tissues involved: neurogenic, venous, and arterial. Neurogenic thoracic outlet is by far the most common, accounting for 98% of cases.1 At a distant second, venous thoracic outlet occurs in 1.5%, followed by arterial at 0.5%. Considerable controversy surrounds the diagnosis of TOS, especially the neurogenic form. However, decades of research have served to better establish pathophysiology, diagnosis, and treatment of this syndrome.
In 1956, Peet et al. caused a major shift in the modern conception of TOS when they coined the term thoracic outlet syndrome and described a therapeutic exercise program, essentially the first physical therapy program for TOS.2 This coincided with a shift of therapeutic focus to surgical intervention. In 1962, Clagett described high thoracoplasty for first rib resection, an operation requiring division of the trapezius and rhomboid muscles.3 In 1966, Roos described what has become for many the modern treatment of choice for TOS, the transaxillary first rib resection.4 This operation was fashioned after the transaxillary sympathectomy. First rib resection by this route offered reasonable exposure and minimal morbidity, especially when compared with previously employed techniques.
Anatomy of the Thoracic Outlet
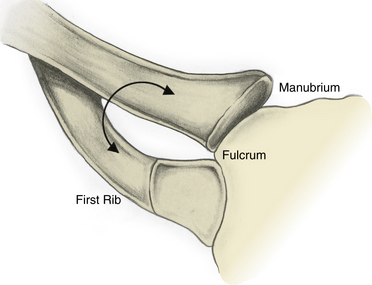
Definitions may vary from author to author, but it is generally accepted that the thoracic outlet is the area from the edge of the first rib extending medially to the upper mediastinum and superiorly to the fifth cervical nerve. The clavicle and subclavius muscles can be pictured as forming a roof, and the superior surface of the first rib forms the floor. Machleder’s description of the thoracic outlet as a triangle with its apex pointed toward the manubrium is helpful in visualizing the three-dimensional (3D) orientation of the structures, as well as the dynamic changes that can lead to injury.5 In this model, the clavicle and its underlying subclavius muscle and tendon form the superior limb, and the base is the first thoracic rib. The point at which these two structures “overlap” medially can be pictured as the fulcrum of a pair of scissors that opens and closes as the arm moves, potentially causing compression of the thoracic outlet contents (Fig. 62-1).
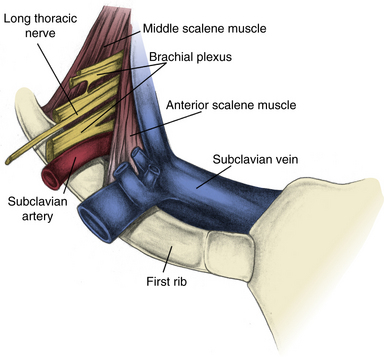
Although most TOS symptoms are related to nerve compression, almost any structure that travels through the thoracic outlet can be involved. Moving from anterior to posterior, one first encounters the exiting subclavian vein, usually positioned adjacent to the region where the first rib and clavicular head fuse to form a fibrocartilaginous joint with the manubrium. Immediately posterior to the vein is the anterior scalene muscle, which inserts onto a prominence on the first rib. Next encountered is the subclavian artery, with the anterior scalene muscle lying between the artery and vein. The brachial plexus is the next structure encountered, oriented superior, posterior, and lateral to the artery. The C4-C6 roots are superiorly oriented, and the C7-T1 roots inferior. Posterior and lateral to the plexus, there is a generally rather broad attachment of the middle scalene muscle to the first rib (Fig. 62-2).
Some authors further classify the thoracic outlet on the basis of three anatomical apertures within this broader space: the interscalene triangle, costoclavicular space, and subpectoral space.6 The most medial aperture that can result in neurovascular compression is within the interscalene triangle. The artery and brachial plexus together pass through this space formed by the anterior scalene anteriorly, middle scalene posteriorly, and first rib inferiorly. Abnormalities of the anterior or middle scalene, presence of a scalenus minimus muscle (seen in <50% of patients, originating between the T1 nerve root and the anterior and inserting onto the pleura and first rib), presence of a cervical rib (0.5% incidence), and presence of fibrous bands (scarring or congenital) can lead to neurovascular compression in this space.6
Lateral and anterior, one can describe the costoclavicular space, bound by the clavicle with its subclavius muscle and tendon anteromedially, the first rib, anterior and middle scalene muscles posteromedially, and the scapula posterolaterally. Bony abnormalities, either congenital or acquired, can narrow this space and result in neurovascular compression. The subclavian vein is especially susceptible to compression in this region as it passes through the narrow space created by the confluence of the clavicle, subclavius muscle and tendon, and the first rib.6
Just deep to the insertion of the pectoralis minor muscle on the coracoid process is the subpectoral aperture. Rarely, neurovascular compression can occur in this space, usually as a result of hyperabduction of the arm, compressing the structures against the chest wall.6
Pathophysiology of Thoracic Outlet Syndrome
The congenital soft-tissue anomalies believed to predispose one to TOS have been well described in the literature. Cadaver studies done by Juvonen, Raymond, and others shed light on the incidence of specific anatomical anomalies in the general population.7 This work is based on the initial observations of Roos, who extensively classified the muscular and fibrous band anomalies seen in patients presenting with TOS.8
Many acquired soft-tissue injuries leading to TOS are the direct result of physical trauma. Studies suggest that soft-tissue injury following motor vehicle trauma (e.g., whiplash) may be the most common underlying etiology.9,10 Other injury patterns include falling onto one’s head and shoulder, causing a lateral stretch injury. In a review of operative TOS patients by Sanders and Hammond,11 86% had a history of trauma. This prevalence of trauma is considerably higher than in many other reports, but stresses the role trauma can play in the disorder.11
Repetitive stress and poor postural habits are also leading causes of TOS.10 Vocations associated with TOS include typists, violinists, or assembly line workers. Other activities include weight lifting or strenuous sports, which lead to hypertrophied scalene musculature. Anatomical studies have documented compression of the subclavian vein into the costoclavicular notch by this muscle.12 This has clear implications for axillosubclavian vein thrombosis. Additionally, some surgeons see a link between Paget-Schroetter’s syndrome and subclavius tendon hypertrophy, particularly in the presence of an enlarged insertion tubercle. Others have implicated a role for the pectoralis minor muscle.13 Rarely, connective tissue disorders have been implicated as a direct causative agent, namely localized scleroderma.14
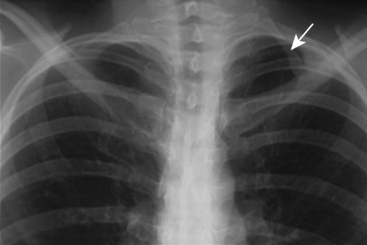
A number of bony abnormalities are found in association with TOS, with the presence of a cervical rib being most common. Autopsy studies indicate that approximately 0.5% of the general population has this structure15 (Fig. 62-3). Further, routine chest radiography demonstrates a cervical rib in roughly 0.7% of individuals.16 Historically, series from the United States report cervical ribs in 10% to 65% of TOS patients, while the European literature reports 25%.15,17 The reason for this discrepancy is not known. It may be at least in part due to variable recognition of neurogenic thoracic outlet in the general population, thus adding bias to these figures. Modern data suggest the percentage of TOS patients with cervical ribs is much lower.
Cervical ribs can be completely formed or rudimentary. In the latter case, there is almost always a compressive band of tissue extending to the first thoracic rib. As they project from transverse processes, cervical ribs displace the involved structures forward. The subclavian artery is particularly vulnerable to damage in this configuration, and some surgeons feel that arterial changes secondary to TOS rarely occur in the absence of a cervical rib. Another common bony anomaly is the presence of an elongated C7 transverse process, which can similarly impinge on the neurovascular structures. Fibrous bands may also be present from an elongated C7 transverse process to the first rib, further worsening the problem.9 Posttraumatic changes following clavicular or first rib fractures are commonly reported, with callous formation at the clavicle and pseudoarthroses of the first rib.18 These changes can frequently be appreciated radiographically.
Presentation of Thoracic Outlet Syndrome
Neurogenic THORACIC OUTLET SYNDROME
Patients can present with the symptoms of neurogenic TOS at any age, although it most commonly occurs in otherwise healthy young to middle-aged individuals. Women are affected three times more frequently than men.1 Neurogenic symptoms can range in severity from nuisance to severely debilitating pain. The most common symptom is pain in an arm, shoulder, and/or the neck. Paresthesias are also commonly present to varying degrees. Although less common, perceived weakness or loss of dexterity can be seen. This occasionally manifests as a decrease in grip strength.1 However, gross motor dysfunction and wasting of the upper extremity is unusual. Gilliat and colleagues description of classic neurogenic TOS with muscle wasting in the hand is seldom seen.19
Pain involving the arm can be focused to a particular nerve distribution or generalized. When localized, ulnar symptoms tend to be the most common, leading to pain and/or paresthesias involving the ring and small fingers. These so-called lower plexus (C8-T1) symptoms are commonly seen. However, upper plexus (C5-C7) manifestations can also be seen, manifesting as pain in the lateral arm and forearm, lateral neck, and deltopectoral region.1
Venous thoracic outlet syndrome (paget-schroetter’s syndrome)
Occasionally, aching pain due to tightness of the skin may also be present, but is absent in the majority of patients.20 However, the typical spectrum of symptoms seen in patients with neurogenic TOS are not usually associated with Paget-Schroetter’s syndrome. Although uncommon, ipsilateral sympathetic hyperactivity can be seen with this condition.
Arterial thoracic outlet syndrome
Arterial TOS is the most rare and varied form of TOS. Chronic compression of the artery leads to insidiously progressive inflammatory changes and scarring of the vessel. These patients rarely present early in the course of this process. Even after they seek medical care, many will have a history that supports the diagnosis, including symptoms such as episodic pallor, cyanosis, and cold intolerance. Patients may present with an array of complaints and physical findings, ranging from intermittent arm claudication to signs of distal embolization or frank ischemia. Rarely, patients may present with aneurysm rupture from long-standing poststenotic dilatation.16
Patients not infrequently are misdiagnosed with collagen vascular disease, various forms of arteritis, or Raynaud’s disease. However, when symptoms are unilateral and isolated to circulation distal to the subclavian artery, one should be alerted to the possibility of arterial TOS. Because there is overlap between the clinical presentation of arterial insufficiency and neurogenic disorders, patients may be misdiagnosed with carpal tunnel syndrome, cervical disc disease, or even neurogenic TOS. It is important to maintain a high index of suspicion for this entity because its clinical presentation is not straightforward.16
Diagnosis of Thoracic Outlet Syndrome
History and physical examination
Because the overwhelming majority of patients who present with a suspected diagnosis of TOS will be of the neurogenic type, this section mainly focuses on this type of TOS. Venous and arterial forms will be discussed later. As with any initial evaluation, an extensive history should be taken, including any injuries and the patient’s occupation. Exacerbating and ameliorating factors should be identified if present. In conjunction with a good history, most cases of TOS can be diagnosed on the basis of physical examination. A thorough examination should focus not only on the site of complaints but also on other areas commonly involved in neurological conditions. This includes the patient’s general appearance and other signs of symptom impact. Deep tendon reflexes, grip strength, and pulses should also routinely be assessed. Palmar hyperhidrosis should be noted if present. Machleder points out that even in neurogenic TOS, changes in pulses can occasionally be detected.21
After this general neurological assessment, tests more specific for the presence of TOS can be undertaken. The most useful test to aid in the diagnosis of TOS is the elevated arm stress test (EAST), which was originally described by Roos in 1966 as a means of eliciting upper-extremity claudication and neurological symptoms.22 In the test, the patient’s arms are placed in 90 degrees of abduction and external rotation, with 90 degrees of flexion at the elbow (“hold-up position”). The patient is then asked to repeatedly clench and unclench the hands. This positioning is designed to constrict the space within the thoracic outlet in an effort to reproduce the patient’s symptoms. When positive in patients with TOS, this test should bring on weakness and paresthesias in the ulnar and median nerve distributions within 3 minutes. Inability to complete testing owing to symptoms is also considered a positive result. Attention should also be made to the color of the hands during the EAST because one may become pale and ischemic if arterial compromise is involved. Proponents of EAST argue that it is specific for TOS and that the length of time to onset of symptoms correlates with severity of TOS. However, some question the anatomical basis for the test, particularly how clenching and unclenching the hand can lead to stress on the brachial plexus.23 This test is not without its detractors. Although anecdotally reported to have excellent specificity, a study from 1985 found a positive test in more than 80% of patients with carpal tunnel syndrome. Other studies conducted using healthy subjects have also reported a high rate of false positives.24,25
Closely related to the EAST is the abduction and external rotation (AER) test. The arm is abducted and rotated and held in that position. This test works by a similar mechanism and likewise produces the weakness and numbness seen with EAST in a similar distribution, namely the C8 to T1 fibers supplying the median and ulnar nerves. In addition, one can sometimes detect a bruit below the lateral portion of the clavicle that is attributable to partial compression of the axillary artery. Both of these tests appear particularly suited to work-related and repetitive motion–associated TOS.26
Although many clinicians routinely assess for pulse changes with these provocative maneuvers, this adds little useful information to such testing. The original Adson test (chin elevation and head rotation toward affected side) consisted of assessment of the radial pulse; Adson sign is subsequent loss of the radial pulse. Although it has historically been used to screen for TOS, Adson sign is also frequently seen in patients without TOS and is unreliably present in those with confirmed TOS. Therefore, it should not be used to establish the diagnosis.1,27 Additionally, Wright described the hyperabduction position back in 1945, which is also of little clinical utility, given its positive result in most healthy individuals. Furthermore, as many as 60% of healthy subjects who undergo EAST will have diminution of the radial pulse.25
Objective testing
Use of objective neurodiagnostic tests for TOS has met with some success, although it continues to be an area of considerable controversy. This modality came to the forefront in the early 1960s, but the anatomical constraints of attempting to measure changes across the brachial plexus have always made its application in this position difficult. Specific techniques vary, but principally these studies evaluate nerve conduction velocity as well as amplitude. The most common and basic electrophysiological studies involve direct motor and sensory nerve testing at the root, cord, trunk, and/or nerve level. Tests are considered abnormal when the velocities and amplitudes deviate from accepted norms. Perhaps the main criticism of these tests is that they only tend to be positive in patients with advanced disease, in whom history and physical examination should be sufficient. Roos suggests they offer “little definitive diagnostic information” and that one “still must rely on careful history and physical.”24 All of this reflects the fact that most electrophysiological tests evaluate larger myelinated nerve fibers, not the smaller fibers whose injury mediates the pain associated with TOS. A study by Franklin et al. found that of 158 TOS patients, only 7.6% had abnormalities in their electrodiagnostic tests.28 Furthermore, this diagnostic modality is subject to significant interobserver bias. No standardized easily reproducible technique has been adopted, nor has any been extensively studied and proven useful in suspected TOS patients. Beyond the limited role of establishing the diagnosis of TOS, these studies can result in significant discomfort for the patient who is already suffering from disabling pain. They should therefore be used only in special instances. These techniques can be useful, however, to exclude the diagnosis of TOS in cases where another neurological process is suspected (e.g., carpal tunnel syndrome).
Let us look closer at some specific techniques that have been used in patients with neurological disorders of the upper extremity. First, several authors have described their experience using ulnar conduction velocity from Erb’s point (above the clavicle and lateral to the insertion of the sternocleidomastoid muscle) to the elbow to assess for TOS, but this technique has been criticized.21 However, if there is severe disease with concomitant axonal damage, changes in ulnar action potentials can be demonstrated. A reasonable approach to conduction studies includes sensory testing of the median and ulnar nerves at the wrist to screen for carpel tunnel syndrome and TOS, respectively.
Electromyography is capable of providing objective data supporting the diagnosis of TOS in a setting of advanced disease. This study demonstrates spontaneous firing of acutely denervated muscle fibers (positive sharp waves, fibrillation potentials), but this is not the usual clinical situation for TOS. Rather, after reinnervation, prolonged and irregular potentials are seen. Because this is a reflection of previous denervation injury, many of these patients have atrophy of the involved muscle groups, and the electromyogram (EMG) can confirm that the lower trunk of the brachial plexus was injured. However, in patients without evidence of atrophy, this test is not likely to reveal these findings. This fact is supported by studies showing that standard EMG tests are negative in 62% of TOS patients.29 However, these tests can be used to examine the paraspinal muscles, which can be important in ruling out radiculopathy as the cause of the patient’s symptoms.
Somatosensory evoked potentials (SSEPs) can play a role in the workup of TOS. Currently, assessment of the ulnar and median nerves can be used for evidence of their compression at the thoracic outlet. When abnormal, these studies tend to show lower plexus injury (ulnar) with normal median function. This is seen primarily as a blunting of Erb’s point peak. Machleder et al.30 showed that 74% of their patients carrying a clinical diagnosis of TOS had abnormal evoked responses. Furthermore, when these patients were studied following operative decompression of their thoracic outlets, more than 90% had correlation between improved symptoms and normalization of their SSEPs.30 Increases of the sensitivity of these tests can be achieved with provocative maneuvers such as arm positioning, although these maneuvers can also cause SSEP changes in patients with no clinical evidence of TOS. Although neurodiagnostic testing remains useful as exclusionary testing, its role in establishing the diagnosis of neurogenic TOS remains limited.
In a study by Jordan and Machleder, 122 patients underwent EMG-guided scalene blockade for a suspected diagnosis of TOS. Reduction in pain was then assessed with provocative maneuvers (generally the EAST); 38 patients went on to have surgical decompression, 32 of whom had a positive result with muscle blockade. The 94% of patients who had a positive response to blockade had a positive long-term result with surgery, as opposed to only 50% of patients with a negative block.31
Beyond its utility as a predictor of good outcome following surgery, lidocaine blockade does offer patients some transient relief while awaiting surgery. However, this effect rarely lasts beyond 1 month. Some groups advocate botulinum toxin injection over lidocaine because of its longer duration of action. This is particularly useful in patients who may have a delay between scalene block and surgery. Jordan et al. also demonstrated in a cohort of 22 patients that botulinum injection results in a 50% reduction of symptoms for a least 1 month in 64% of patients (mean duration of 88 days). This is in contrast to only 12% of patients with continued symptomatic relief beyond 1 month when receiving lidocaine alone.32
Finally, some centers advocate the use of duplex ultrasonography to assess for the presence of TOS. To perform this test, provocative maneuvers in conjunction with color Doppler are used to assess blood flow velocities in the subclavian artery and vein. In theory, patients without TOS will have minimal velocity changes within the subclavian artery during varying degrees of abduction of the arm. If the patient’s symptoms are related to TOS, one would expect to see velocity changes. First, as the artery becomes partially compressed, velocity in the artery increases. Further abduction will worsen compression to the point where flow is diminished, and one should see a resultant decrease in velocities. Finally, with hyperabduction the compression may be so severe that the vessel becomes occluded, with cessation of flow. Recent data have given support to this modality. In a small cohort of patients suspected of having TOS on the basis of symptoms and physical examination, all patients demonstrated the anticipated hemodynamic changes described. With 120 degrees of abduction, mean peak systolic velocities increased greater than 50%. At 180 degrees of abduction, velocities were reduced below baseline values, and hyperabduction revealed absent flow in all patients for whom data were available. As anticipated, venous duplex revealed changes suggestive of venous compression, namely loss of atrial and respiratory dynamics, increased velocities, and increased turbulence.33 Although this study was underpowered to definitively establish duplex ultrasonography as a proven diagnostic modality in TOS, it does offer promising data. Validating studies should be conducted to further our understanding of the role of ultrasound in TOS.
Diagnosis of venous thoracic outlet syndrome
In the TOS patient who presents with upper-extremity swelling, the diagnosis of axillosubclavian vein thrombosis is suggested by the history and physical examination described earlier. Assessment of the venous system is usually initiated with noninvasive duplex ultrasonography and dynamic phlebography (also see Chapter 12). Provocative positioning, such as external rotation and abduction, can increase the sensitivity of these tests. Other authors describe a two-position technique, with the arms fully adducted and then 90 degrees abducted. It is not clear at this time how useful magnetic resonance venography (MRV) is for axillosubclavian evaluation. It appears to have anatomical limitations similar to duplex ultrasonography, with poor quality of images in the retroclavicular space.
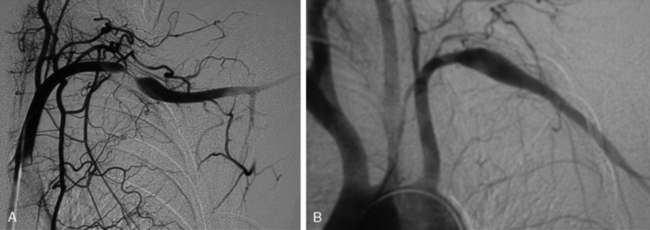
Many patients undergo a diagnostic venogram, which is the gold standard for thrombosis in this situation (Fig. 62-4). Occlusion of the axillosubclavian vein is readily identified with this diagnostic modality. Typically, patients will also have numerous venous collaterals not seen in normal individuals without thrombosis. Although this test confirms the diagnosis of venous thrombosis, the occasional patient needs further clarification as to its cause. Neurogenic symptoms are usually not present, and one must often rely on exclusion of causes of venous thrombosis other than TOS in this situation.
Diagnosis of arterial thoracic outlet syndrome
Frequently, arterial compression can be better visualized if the arm is abducted 90 degrees, and most studies are obtained with the arms in two positions (Fig. 62-5). When distal embolization is suggested, the angiography should encompass the target sites, often requiring studies of the hand on the affected side. Provocative positioning (abduction) can be used in conjunction with angiography to demonstrate arterial compression.
Treatment of Thoracic Outlet Syndrome
For many TOS surgeons, referral patterns are such that patients have already undertaken unsuccessful conservative therapy before seeking further consultation. It is important for surgeons to be aware of this selection bias. It is also important to have an algorithm for conservative treatment so that the correct patients are selected for operation. A minimum of 6 weeks of physical therapy is required before its effects can be evaluated. It is also important that the correct program be used because it has been recognized that inappropriate physical therapy can worsen TOS symptoms. In general, these programs are designed to relax muscle groups that tighten the thoracic outlet while conditioning those that open it. Aligne and Barral described a program in which the trapezius, levator scapulae, and sternocleidomastoid muscles are strengthened and the middle scalene, subclavius, and pectoralis muscles relaxed.34
Surgical treatment
When a symptomatic patient who has sought treatment fails to improve with physical therapy, surgical intervention is warranted. Resection of the first rib and anterior scalenectomy can be performed via either the transaxillary or supraclavicular approach. In our practice, we preferentially use the transaxillary approach owing to its excellent exposure of the first rib, minimal morbidity, and better cosmetic appearance. The patient is placed in the lateral decubitus position, with the head neutral. No paralytic agents are used beyond short-acting agents for induction. Various devices are available for elevation of the arm on the operative side, all of which should permit easy lowering of the extremity intermittently throughout the procedure to allow periods of increased arterial inflow and decreased tension on stretched nerves (Fig. 62-6). The incision is placed between the pectoralis major and the latissimus dorsi in the lower aspect of the axilla. Dissection is carried down to the chest wall, with care taken to identify intercostal brachial cutaneous nerves. These structures should be avoided and preserved when possible, but it is preferable to sacrifice them rather than leave them injured, thereby subjecting the patient to possible causalgic pain.
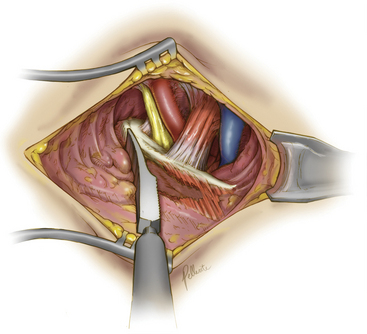
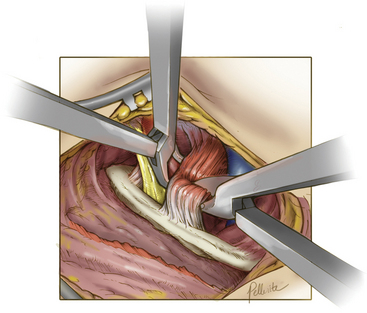
Deep dissection begins by bluntly exposing the external surface of the first rib. Using a periosteal elevator, intercostal muscle and soft-tissue attachments to the first rib are cleared (Fig. 62-7). The parietal pleura is then bluntly dissected away from the internal surface of the first rib. The anterior surface of the first rib is cleared of soft tissue and middle scalene fibers, again using the periosteal elevator. Care is taken to not cut the fibers of the middle scalene. The long thoracic nerve often traverses the muscle in this region, and injury to the long thoracic nerve will result in a winged scapula and is associated with significant long-term disability. Tissue is then cleared bluntly overlying the nerve, artery, and vein. The anterior scalene muscle is now carefully separated from the subclavian vessels, and its attachment to the first rib is divided (Fig. 62-8). The subclavius tendon is also divided.
The supraclavicular approach for scalenectomy (with or without first rib resection) is considered in three situations. The first is when the patient’s symptoms are particularly suggestive of upper brachial plexus involvement (as opposed to the more common lower plexus). As described by Roos,35 it is reasonable to use an approach in which these nerves can be more directly decompressed. The second situation is in patients who have undergone transaxillary operation but now have upper plexus symptoms. The third situation is a matter of preference when a surgeon feels the supraclavicular approach is as effective as and safer than the transaxillary operation. The first rib can also be resected as a component of this procedure, although some argue that it cannot be done with the same margins as the transaxillary approach.
A brief mention should be made here of some alternative surgical approaches for patients with TOS. Some advocate for a thoracoscopic approach to rib resection and scalenectomy. Although offered at several centers, this procedure has not gained widespread acceptance. Many question the stated benefits over the transaxillary approach.36 Also reported in the literature is endoscopic-assisted transaxillary rib resection and scalenectomy. Again, this has not been demonstrated in any large series to be superior to the traditional approaches.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree