Valvular Heart Disease
Dermot Phelan • Maran Thamilarasan
QUESTIONS
Case 1
A 60-year-old man presents to the emergency room with complaints of weakness, lethargy, and severe dyspnea. One week prior, his family notes that he complained of chest pressure that lasted for several hours. On physical examination, he appears to be in respiratory distress. Blood pressure (BP) is 80/50 mmHg. Heart rate is 130 bpm. His oxygen saturation is 87% on room air. Chest examination reveals diffuse crackles. Cardiac examination reveals a nondisplaced point of maximum impulse (PMI). Third and fourth heart sounds are heard, as is an apical systolic murmur. No thrill is present. Electrocardiogram reveals inferior Q waves without ST-segment elevation. He is urgently intubated and pressors are started. An intra-aortic balloon pump is placed. A surface echocardiogram reveals a normal-sized left atrium and a mild jet of mitral regurgitation (MR).
1.What test do you perform first?
a.Cardiac catheterization
b.Transesophageal echocardiography (TEE)
c.Right heart catheterization with an oxygen saturation run
d.Administration of thrombolytic therapy
2.A TEE is performed urgently (Fig. 2.1 shows a 3D view of the mitral valve from above). What is the most likely diagnosis?
a.Endocarditis involving the mitral valve
b.Posterior papillary muscle rupture as it has a single blood supply
c.Anterior papillary muscle rupture as it has a single blood supply
d.Severe mitral valve prolapse secondary to recent myocardial infarction
Case 2
A 65-year-old woman presents to your office for follow-up of a murmur she was told about several years prior. She denies any symptoms, but is not very active. Her past medical history is significant for hypertension and diabetes, both of which have been well controlled. On examination, she is in no acute distress. BP is 125/75 mmHg, with a resting heart rate of 70 bpm. Lungs are clear. Cardiac examination reveals a displaced PMI. S1 is soft. S2 reveals an increased P2 component. There is a right ventricular (RV) lift. An S3 is present. There is a grade III/VI holosystolic murmur heard at the apex radiating to the base. She has no peripheral edema. Chest X-ray demonstrated cardiomegaly with prominence of the central pulmonary vasculature.
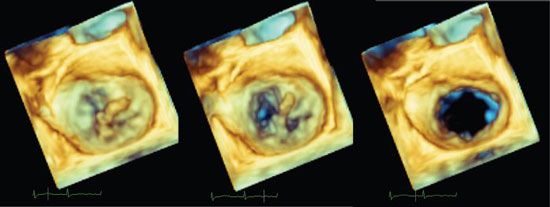
Figure 2.1
3.An echocardiogram is performed on this patient (Fig. 2.2). Left ventricular (LV) systolic dimension is 4.7 cm. Ejection fraction is 45%. There is posterior leaflet prolapse. There is a very eccentric jet of MR, which is read out as 2+. Which of the following is most likely?
a.MR is unlikely to account for her presentation.
b.She likely has more severe MR than is evident on the echocardiogram.
c.Her LV function is better than it appears on the echocardiogram.
d.TEE is unlikely to be helpful here.
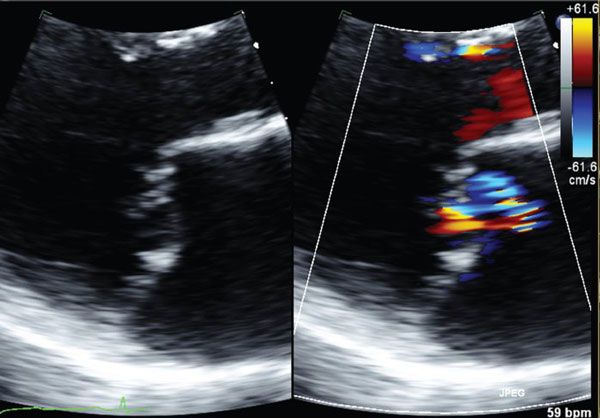
Figure 2.2
4.What do you recommend next?
a.Stress echo, to assess LV and PA (pulmonary artery) pressures post stress
b.Mitral valve surgery
c.Start an angiotensin-converting enzyme inhibitor (ACEI) and reassess in 3 months
d.Start a β-blocker
Case 3
A 40-year-old woman is referred to your office for evaluation of a murmur heard during a routine physical examination. She is asymptomatic. She used to jog 2 to 3 miles a day without problems but over the past few years has stopped exercising. She had frequent febrile illnesses as a child, but her past medical history is otherwise unremarkable.
Physical Examination
BP 120/70 mmHg, pulse 73 bpm.
She is in no acute distress.
Jugular venous pulse (JVP) is not elevated.
Chest is clear.
Cardiac—PMI not displaced. Regular rate and rhythm. S1 is increased in intensity. S2 is normal. A high-pitched diastolic sound is heard at rest and is heard best between the apex and left sternal border, 0.10 seconds after S2. This is followed by a low-pitch decrescendo murmur with pre-systolic accentuation.
Abdomen—No organomegaly.
Extremities—No edema. Normal distal pulses. Good capillary refill.
An echocardiogram is performed (Fig. 2.3); proximal flow convergence radius (PFCR) using color 3D across the mitral valve indicates an orifice area of 1.2 cm2. Resting PA pressures are 35 mmHg. Splittability score is 5. LV size and function are normal.

Figure 2.3
5.Which of the following would be the most reasonable next step in management?
a.Immediate referral for surgery
b.Immediate referral for percutaneous valvuloplasty
c.Stress echocardiogram, to assess for mitral pressures post stress
d.Follow-up in 2 years
6.A stress echocardiogram is performed. Patient exercises for 6 metabolic equivalents (METs). Right ventricular systolic pressure post stress is estimated at 70 mmHg. Which of the following would be an appropriate next step?
a.Consideration for percutaneous valvuloplasty
b.Mitral valve replacement
c.Start β-blocker and return for follow-up in another 2 years
d.Start digoxin
Case 4
A 50-year-old woman presents to you for evaluation. She complains of easy fatigability, as well as abdominal fullness and right upper quadrant pain. She also notes marked swelling in her legs. She has recently been diagnosed with asthma and is also undergoing evaluation for recurrent diarrhea. On examination, she has a BP of 100/60 mmHg. Heart rate is 96 bpm. There is elevation in jugular venous pressure, with a large a wave and a prominent v wave. Lungs are clear. Cardiac examination reveals a nondisplaced PMI. Rhythm is regular. S1 and S2 (including P2) are normal. A diastolic murmur is heard along the sternal border, which increases with inspiration. A pansystolic murmur is also heard in this area. Hepatomegaly is present, along with ascites and peripheral edema.
7.What is the most likely cause of this patient’s signs and symptoms?
a.Rheumatic heart disease
b.Carcinoid
c.Primary pulmonary hypertension
d.Cirrhosis of the liver secondary to chronic hepatitis
Case 5
A 28-year-old man is referred to your office for a second opinion regarding his hypertension. On physical examination, he is in no acute distress. BP is 160/90 mmHg, symmetric in both arms. Pulse rate is 75 bpm. Cardiac examination reveals a nondisplaced PMI. S1 is normal. It is followed by a high-pitched sound widely transmitted throughout the precordium. A short II/VI systolic ejection murmur is heard. S2 is normal.
8.What is the most important diagnostic test to perform next?
a.Check plasma catecholamines.
b.Check serum potassium level.
c.Check lower extremity BP.
d.Check plasma cortisol levels.
Case 6
A 59-year-old man presents for further evaluation of recurrent congestive heart failure. He appears to be in no acute distress on your evaluation. BP is 100/60 mmHg. Carotid upstrokes are weak, but not delayed. Chest examination shows minimal bibasilar rales. PMI is displaced and sustained. A summation gallop is present. There is an increased P2. There is mild peripheral edema. An echocardiogram reveals a dilated LV with an ejection fraction of 25%. The aortic valve does have some calcification, with restricted leaflet excursion. Peak/mean gradients are 25/15 mmHg. By the continuity equation, the aortic valve area is calculated as 0.7 cm2.
9.What is your next step?
a.Immediate referral for aortic valve replacement (AVR)
b.Referral for cardiac transplant
c.Dobutamine echocardiogram
d.Start an ACEI
10.With dobutamine echocardiography, the gradients across the valve increase to 60/40 mmHg, and the calculated valve area stays at 0.7 cm2. What do you recommend?
a.AVR
b.Continued medical management
c.Cardiac transplant evaluation
d.Balloon aortic valvuloplasty
11.Alternatively, how would you interpret the following results: an increase in stroke volume by 5% and an increase in peak/mean gradients to 30/19 mmHg without a significant change in the aortic valve area?
a.Patient has true severe aortic stenosis (AS) and should proceed to surgery.
b.Patient has pseudo-AS and should be managed with medical therapy alone.
c.Patient has a lack of contractile reserve and should be managed with medical therapy alone.
d.Patient has a lack of contractile reserve but should still be considered for AVR.
Case 7
A 32-year-old man with known bicuspid aortic valve is referred to you for management of aortic insufficiency (AI). He is completely asymptomatic and jogs 3 miles a day as well as doing other aerobic exercise for 30 minutes daily. He has a grade III/VI systolic and diastolic murmur at his left sternal border, a collapsing pulse on examination, and his BP 170/70 mmHg. An echocardiogram reveals a mildly dilated LV (end-diastolic dimension of 6.0 cm) with an ejection fraction of 65%. There is prolapse of the conjoined aortic leaflet with 3 to 4+ insufficiency.
12.What is your recommendation?
a.Referral for surgery
b.Addition of vasodilator therapy
c.Observation for now, return for follow-up in 3 years
d.Cardiac catheterization
13.What do you tell him is his yearly risk of sudden death?
a.<1%
b.2%
c.3% to 5%
d.>5%
14.The above patient undergoes a gated computed tomography angiography of the thorax (Fig. 2.4), what would you recommend?
a.Observation with echocardiography every 6 months
b.Start a β-blocker and reassess in 6 months
c.Refer to computed tomographic (CT) surgery for surgical replacement of his aortic valve
d.Referral for surgical intervention to repair or replace his aortic valve and to replace his ascending aorta
Case 8
A 76-year-old woman has been accepted for AVR for severe symptomatic AS. Your opinion is sought by the cardiothoracic surgeon regarding best management of reported concomitant valvular lesions. On review of the echocardiogram you confirm severe AS. In addition, you note a morphologically normal mitral valve, mild MR, and moderate tricuspid regurgitation (TR) associated with annular dilation (45 mm). There is also mild pulmonary hypertension.
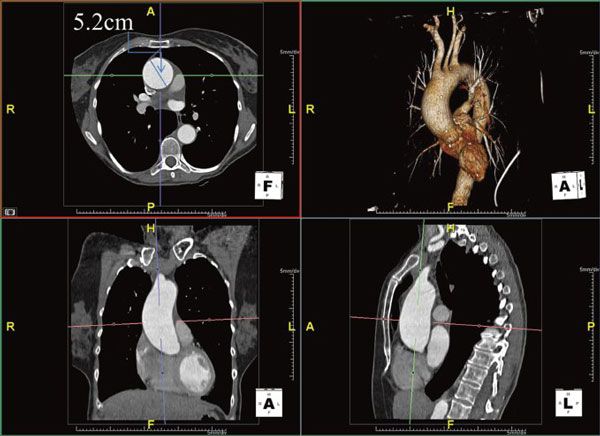
Figure 2.4
15.What do you recommend?
a.AVR alone
b.AVR with mitral and tricuspid valve repair
c.AVR with tricuspid valve replacement
d.AVR with tricuspid valve repair if feasible
e.AVR and mitral valve repair alone
Case 9
A 46-year-old woman with chronic obstructive pulmonary disease is referred by her pulmonologist for evaluation of a murmur and concern that her symptoms of shortness of breath with moderate exertion may be related to severe MR diagnosed on an outside echocardiogram. On examination, her body mass index is 19 kg/m2, BP is 130/75 mmHg, and her heart rate is 75 bpm and regular. Her apex beat is nondisplaced. On auscultation, S1 and S2 are normal; there is a mid-systolic click with a grade IV/VI late systolic murmur heard best at the apex. An echocardiogram is performed (Fig. 2.5A).
16.Assuming an aliasing velocity of 40 cm/s and an MR Vmax of 5 m/s, based on the PFCR seen here, what is the estimated effective regurgitant orifice area (EROA)?
a.0.4 cm2
b.0.45 cm2
c.0.18 cm2
d.Not enough information to calculate an EROA
17.A continuous-wave signal is provided through the mitral valve (Fig. 2.5B); based on the data provided how would you classify this MR?
a.1+, mild
b.2+, moderate
c.3+, moderately severe
d.4+, severe

Figure 2.5A

Case 10
A 45-year-old man with rheumatic mitral stenosis presents for further evaluation. In the past 2 to 3 years, he has noted progressive dyspnea with less than moderate activity. He was started on a β-blocker 1 year ago, but remains symptomatic. Echocardiogram reveals a mean mitral gradient of 4 mmHg with a valve area of 1.6 cm2. As there was a discrepancy between the degree of symptoms and resting hemodynamics you proceed to a stress echocardiogram that revealed a post stress PA pressure of 70 mmHg and a mean transmitral gradient of 17 mmHg. You decide to send this patient for percutaneous intervention.
18.What is the most appropriate test to order at the time of or prior to the valvuloplasty procedure?
a.Transesophageal echocardiogram
b.24-Hour electrocardiographic monitoring to assess for paroxysmal atrial fibrillation
c.Cardiac CT to assess for aortic calcification
d.Stress nuclear perfusion study
Case 11
A 65-year-old man is referred to you for evaluation of a heart murmur. He denies any symptoms at this time. On physical examination, he is in no acute distress. BP is 135/75 mmHg; pulse is 82 bpm and regular. Carotid upstrokes are diminished. The PMI is sustained and displaced. A2 is soft. A late-peaking systolic murmur is heard at the base. You order an echocardiogram. This reveals LV hypertrophy with moderate global impairment of LV function, calculated ejection fraction of 35%. There is severe calcific AS, with peak/mean gradients of 75/45 mmHg. Aortic valve area is 0.5 cm2.
19.What is the role of AVR in this setting?
a.It is absolutely indicated.
b.It is absolutely not recommended.
c.There is some evidence/opinion that would favor valve replacement.
d.Dobutamine echocardiography is needed to determine whether this is truly severe AS.
Case 12
A 76-year-old woman is referred to your clinic with recent onset of exertional chest pain. She has a long-standing history of hypertension and atrial fibrillation. On examination, her body surface area is 2.0 m2, BP is 150/100 mmHg, and heart rate is 80 to 90 bpm and irregular. The carotid upstroke is delayed and diminished. The apex beat is nondisplaced but sustained. S1 is normal, and S2 is soft and paradoxically split. There is a grade II/VI ejection systolic murmur heard best at the right upper sternal border that radiates to the carotids. An echocardiogram reports normal ejection fraction with a stroke volume of 55 mL. The peak and mean gradients across the aortic valve are 44/28 mmHg. The dimensionless index is 0.21 and the calculated aortic valve area is 0.83 cm2. You review the echocardiogram (Fig. 2.6) and confirm the accuracy of the left ventricular outflow tract (LVOT) diameter and are satisfied that multiple windows were used to obtain the gradients.
20.Which of the following statements is true?
a.The patient has moderate AS confirmed by gradients across the valve and should be followed up in 6 months with a repeat echocardiogram.
b.The echocardiogram shows inconsistent data and should be repeated.
c.This is a definite contraindication to AVR.
d.The rate of mortality, for a patient with these findings, is higher compared with patients with severe AS and high gradients across the aortic valve, but aortic valve surgery has resulted in better outcomes in these patients.
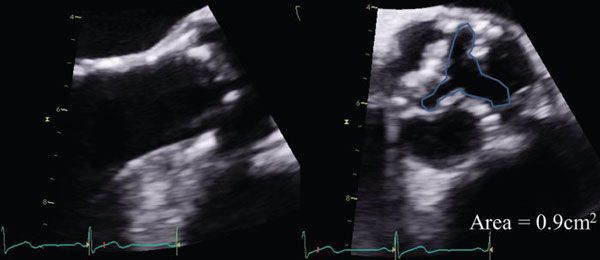
Figure 2.6
Case 13
A 75-year-old man is referred to you for evaluation of aortic regurgitation. He has no symptoms at this time. His past medical history is significant only for hypertension. On physical examination, he is in no acute distress. BP is 170/60 mmHg. Arterial pulses are brisk. A bisferiens pulse is noted in the brachial artery. The apical impulse is displaced and hyperdynamic. S1 is not loud, and no opening snap is heard. A high-frequency holodiastolic murmur is heard, loudest along the right sternal border. A late diastolic apical rumble is heard as well.
21.You order an echocardiogram. Which of the following are you most concerned about?
a.Aortic valve commissural anatomy
b.Degree of AI
c.Aortic root dimension
d.Mitral valve
22.The above patient returns for follow-up 6 months later. He now reports symptoms of marked exertional dyspnea. An echocardiogram is read as 2+ central aortic regurgitation, with an LV end-diastolic dimension of 6.9 cm and an ejection fraction of 50%. What do you do next?
a.Cardiac catheterization with aortography
b.Start an ACEI, reassess in 6 months
c.Continue observation
d.Start a β-blocker, reassess in 6 months
Case 14
A 56-year-old man presents to the emergency room with the sudden onset of chest pain. He is tachypneic on presentation. O2 saturation is 82% on room air. BP is 80/60 mmHg. Heart rate is 125 bpm. Lung examination reveals diffuse bilateral crackles. Cardiac examination reveals a nondisplaced PMI. S1 is soft. P2 is loud. An S3 is present. A short decrescendo diastolic murmur is heard at the upper sternal border. Extremities are cool. Electrocardiogram reveals inferior ST-segment elevation. He is promptly intubated, and pressors are started. A brief echocardiogram is performed at the bedside. The study is difficult, but reveals premature closure of the mitral valve. There is hypokinesis of the inferoposterior walls.
23.Which of the following would be your next course of action?
a.Transesophageal echocardiogram, emergent cardiac surgical consultation
b.Intra-aortic balloon pump to stabilize hemodynamics, followed by emergent angiography
c.Administer thrombolytics
d.Send patient for magnetic resonance imaging (MRI)
Case 15
A 77-year-old patient is admitted to the hospital for urosepsis. His past medical history is significant only for having undergone AVR 5 years prior. On examination, he is febrile to 102°F. Heart rate is 106 bpm. Carotid upstrokes are full. Chest examination reveals clear lung fields. Cardiac examination reveals a hyperdynamic apical impulse, which is not displaced. S1 and S2 are normal. An early-peaking systolic murmur is heard at the sternal border. No diastolic murmur is heard. An echocardiogram is performed. Peak/mean gradients are 50/30 mmHg. LVOT VTI (velocity time integral) is 36 cm and aortic valve VTI is 78 cm. The aortic valve itself is not well seen. Flow in the descending thoracic aorta is normal. An echocardiogram 2 years prior had revealed peak/mean gradients of 24/12 mmHg. LVOT VTI was 19 cm and aortic valve VTI 41 cm.
24.What do you conclude about prosthetic aortic valve function?
a.He has prosthetic valve stenosis
b.No evidence for dysfunction
c.He has severe prosthetic valve regurgitation
d.He likely has endocarditis
25.The above patient remains febrile despite 1 week of antibiotic therapy. Electrocardiogram reveals a new long first-degree atrioventricular (AV) block. The patient becomes progressively dyspneic. A short, regurgitant murmur is heard. What do you recommend?
a.TEE with surgical consultation
b.TEE
c.Change antibiotic regimen
d.Monitor closely with daily electrocardiogram
Case 16
A 56-year-old man with mitral stenosis presents for evaluation. He has NYHA class II-III shortness of breath.
Physical Examination
He is in no acute distress.
JVP is mildly elevated.
Pulse is regular at 80 bpm.
Chest is clear.
Cardiac: Nondisplaced PMI. Opening snap heard 0.09 milliseconds after S2. Long diastolic rumble. No peripheral edema.
Echocardiogram reveals a planimetered mitral valve area of 1.2 cm2. Mean gradient 10 mmHg. Pressure half-time of 185 milliseconds.
He undergoes percutaneous valvuloplasty. The following morning, on examination, you note that he is comfortable. His oxygen saturation is 100% on room air. Opening snap is 0.12 milliseconds after S2. A shorter decrescendo diastolic rumble is heard. You obtain a predischarge echocardiogram. The report indicates a pressure half-time of 180 milliseconds.
26.What do you do next based on the echocardiogram?
a.There was a less-than-optimal result from the valvuloplasty. No significant change in mitral valve area was achieved. You plan to send him for another procedure or surgery.
b.There was an error in half-time measurement. You order a repeat assessment of pressure half-time later that day.
c.Repeat echocardiogram with planimetry of mitral valve area.
d.Consider TEE to see the valve opening better.
27.The echocardiogram reveals a small left-to-right shunt at the atrial level by color. What do you recommend?
a.Observation
b.Referral for percutaneous closure
c.Referral for surgical closure
d.Indefinite anticoagulation
Case 17
An 80-year-old man underwent successful AVR with a bioprosthetic valve 4 months ago. He presents to your office for a routine follow-up visit. He is asymptomatic. He is in sinus rhythm. Echocardiogram reveals a normally functioning prosthetic valve. Chamber dimensions are normal with normal biventricular function. He has no clinical history of embolic events.
28.Which of the following should you recommend?
a.Antibiotic prophylaxis, office visits if he feels unwell
b.Antibiotic prophylaxis, with yearly office visits
c.Warfarin therapy indefinitely
d.Clopidogrel therapy indefinitely
Case 18
A 28-year-old 20-week pregnant woman is referred to your clinic after being diagnosed with mitral valve prolapse and severe MR on an echocardiogram ordered by her obstetrician. She reports no symptoms prior to pregnancy but since being told her diagnosis is extremely worried and has noticed some shortness of breath on exertion (New York Heart Association [NYHA] class II). She is clinically euvolemic.
29.What do you recommend?
a.Antibiotics at the time of delivery
b.Commence afterload reduction with an ACEI given her new onset symptoms
c.Refer to an experienced surgeon for consideration for mitral valve repair as there is a high likelihood of successful durable repair
d.Commence afterload reduction with diuretics and hydralazine
e.No therapy at present but follow carefully with serial clinical and echo evaluation
Case 19
A 67-year-old woman is referred to your office for evaluation of a heart murmur. She describes symptoms of significant and limiting exertional dyspnea. On examination, she is normotensive. Pulse rate is 67 bpm and regular. Cardiac examination reveals a sustained but nondisplaced PMI. S1 and S2 are normal. An S4 is present. A loud III/VI systolic ejection murmur is heard throughout the precordium. Carotid upstrokes are delayed and diminished. An echocardiogram is performed (Fig. 2.7); continuous-wave Doppler evaluation reveals a 4.5-m/s jet across the LVOT.
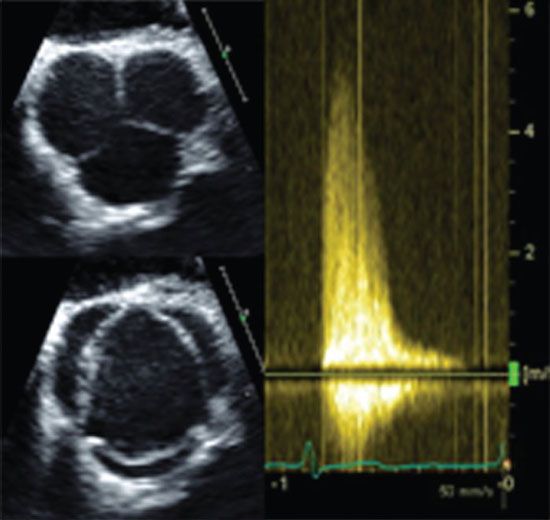
Figure 2.7
30.Which of the following would you do next to arrive at a diagnosis?
a.TEE
b.Repeat echocardiogram with amyl nitrate
c.Stress echocardiogram
d.Dobutamine echocardiogram
e.The Pedoff probe has picked up an MR signal, the MR appears mild on all other views, no need for further investigation
Case 20
A 30-year-old woman presents to your office for a routine physical examination. She is asymptomatic. BP is 95/65 mmHg, with a resting heart rate of 65 bpm. Physical examination is remarkable for a mild pectus deformity. On cardiac auscultation, a mid-systolic click is heard. The click is heard earlier in systole with standing, and later in systole with squatting. No murmur is heard at rest, but a soft systolic murmur becomes audible with dynamic maneuvers.
31.Echocardiography demonstrates no high-risk features. What is the role of aspirin therapy in such patients who have had no evidence of embolic events?
a.Should be prescribed to all patients
b.May play a role, if a murmur is heard
c.There is no clear role for aspirin therapy in such patients
Case 21
A 50-year-old man with severe AI is referred to you for a second opinion. He is asymptomatic. An echocardiogram reveals a mildly dilated LV (end-diastolic dimension of 6.2 cm and end-systolic dimension of 3.5 cm) with a normal ejection fraction. He has already undergone a stress echocardiogram. He exercised for 14 METs. No symptoms or electrocardiographic changes were noted. Resting ejection fraction was calculated at 65%. Post stress, the ejection fraction is 60%. No segmental wall motion abnormalities were seen.
32.What do you recommend?
a.Surgical intervention
b.Continue with vasodilator therapy and reassess in 6 months
c.Cardiac catheterization
d.Stress nuclear ventriculogram
Case 22
A 70-year-old man presents to your office with complaints of exertional dyspnea. He is mildly hypertensive on examination. Carotid upstrokes are brisk, with a secondary upstroke. A loud III/VI systolic murmur is heard along the sternal border radiating to the neck. S1 and S2 are normal. An S4 is heard. The murmur increases in intensity with Valsalva and decreases with handgrip.
33.An echocardiogram reveals a <2-m/s jet across the LVOT. What is your next step?
a.Repeat the echocardiogram, but have Doppler interrogation performed in other views and with a nonimaging transducer. The degree of AS has been underestimated
b.Repeat the echocardiogram with amyl nitrate
c.Transesophageal echocardiogram to better assess the valves
d.Coronary angiography
Case 23
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


