Hyperlipidemia
Michael B. Rocco
QUESTIONS
1.Familial hypercholesterolemia (FH) is a common autosomal dominant disorder resulting from mutations leading to impaired hepatic clearance of low-density lipoprotein (LDL) from the circulation. All of the following statements are true regarding heterozygous FH except that
a.it occurs in 1 in 5,000 persons.
b.it is associated with serum low-density lipoprotein cholesterol (LDL-C) two to three times above the average.
c.it is associated with four- to sixfold increased risk of premature coronary heart disease (CHD).
d.without treatment, the average age for development of symptomatic CHD is 45 years in men and 55 years in women.
e.ninety percent of FH heterozygotes exhibit detectable xanthomas on the extensor tendons of the hands or on the Achilles tendons by the age of 39.
2.Phenotypic presentation of FH has been demonstrated to be caused by various mutations associated with all but one of the following:
a.Defects in the hepatic LDL receptor (LDL-R)
b.Defects in apolipoprotein B (apoB)
c.Loss-of-function mutation of PCSK9
d.Loss-of-function mutation of LDLRAP1
3.A 31-year-old man is referred to you for hyperlipidemia assessment. He has no previous cardiovascular history himself and denies any first-degree relatives with a history of CHD although his father and paternal uncle are treated for elevated cholesterol and triglycerides (TGs). He reports that two uncles and a cousin have had heart attacks at young ages. His physical examination reveals a body mass index (BMI) of 32, arcus cornea and xanthelasmas but no xanthomas, and a blood pressure (BP) of 150/80 mmHg. His fasting lipid profile is as follows: total cholesterol (TC) 300 mg/dL, TGs 430 mg/dL, high-density lipoprotein cholesterol (HDL-C) 50 mg/dL, direct LDL-C 202 mg/dL. Fasting blood glucose is 112 mg/dL. Which primary dyslipidemia is this patient most likely to have?
a.Polygenic hypercholesterolemia
b.Heterozygous FH
c.Familial combined hyperlipidemia
d.Hyperapobetalipoproteinemia
e.Familial endogenous hypertriglyceridemia
4.Which of the following statements regarding FH is NOT true?
a.The Food and Drug Administration (FDA) indications for LDL apheresis after maximal tolerated pharmacologic therapy include (a) homozygous FH patients and (b) heterozygous FH in the absence of CHD when LDL-C ≥300 mg/dL and in the presence of CHD when LDL-C ≥200 mg/dL.
b.Mipomersen (which inhibits the translation of apoB100 mRNA, thus blocking the production of apoB100 and formation of very low-density lipoprotein [VLDL] and LDL particles) lowers LDL-C by 28% to 36% in individuals with homozygous and heterozygous FH.
c.TC levels are generally >600 mg/dL with LDL-C levels 6- to eightfold higher than average in individuals with homozygous FH.
d.Lomitapide has been approved to treat homozygous and heterozygous FH.
e.Simon Broome Register Group criteria for definite FH requires (a) TC >290 mg/dL in adults or TC >260 mg/dL in children under 16 years OR LDL-C >190 mg/dL in adults or >155 mg/dL in children PLUS (b) tendon xanthomas in the patient, or first- or second-degree relative OR DNA-based evidence of mutations such as LDL-R mutation or familial defective apoB100.
5.Recent statistics from the American Heart Association (AHA) Statistical Update in 2014 report that all of the following regarding dyslipidemia in the United States are true EXCEPT that
a.98,900,000 U.S. adults over 20 years of age have elevated TC >200 mg/dL (43.4%).
b.35.8% of adults have LDL >130 mg/dL (71 million adults).
c.48.7 million adults (21.8%) have HDL <40 mg/dL.
d.National Health and Nutrition Examination Survey (NHANES) data through 2006 reported that 10.3% of adolescents (12 to 19 years) have abnormal lipid levels.
e.inadequate control of dyslipidemia is responsible for 4 million yearly deaths worldwide and 350,000 in the United States.
f.68.2% of adults and 31.8% of children/adolescents are overweight or obese.
6.Many randomized clinical trials (RCTs) and meta-analyses have contributed to the lipid management guidelines over the past two decades. Which of the following statements is NOT correct?
a.PROVE-IT/TIMI-22 showed that individuals post myocardial infarction (MI) treated with the more potent statin atorvastatin versus pravastatin had a 16% relative risk reduction.
b.The JUPITER trial demonstrated that in individuals without documented cardiovascular disease (CVD) and median LDL-C of 108 mg/dL, aggressive statin therapy with rosuvastatin offered greater benefit in individuals with ultrasensitive C-reactive protein (usCRP) >2 versus <2 mg/L.
c.Primary prevention hypertensive patients in the ASCOT-LLA trial showed reductions in nonfatal MI, CHD death but not all-cause mortality when patients with average lipids and hypertension were treated with atorvastatin 10 mg daily for an average of 3.3 years.
d.WOSCOPS and AFCAPS/TexCAPS were both primary CHD prevention studies, which showed significant clinical benefits for statin therapy, with similar percentage reductions in LDL-C. The main difference between these trials was that subjects in AFCAPS/TexCAPS had considerably lower baseline LDL-C levels than those in WOSCOPS.
e.Scandinavian Simvastatin Survival Study (4S), Cholesterol and Recurrent Events (CARE), and Long-Term Intervention with Pravastatin in Ischemic Disease (LIPID) all involved secondary prevention of CHD.
f.Meta-analyses have demonstrated a >20% reduction in CHD events for every 1 mmol/L reduction in LDL-C with similar proportional reductions in diabetics versus nondiabetics. Similar percent reductions were seen even in lower-risk groups with <5% 5-year risk for CVD.
7.The Framingham Risk Score (FRS) was popularized in the National Cholesterol Education Project: Adult Treatment Panel (NCEP ATP) III guidelines. Potential limitations of the FRS include the following:
1.Does not take family history into account
2.May overestimate lifetime risk in individuals ≤50 years of age with ≥1 NCEP risk factor
3.May not accurately calculate risk in certain ethnic groups because original Framingham population was almost entirely of European origin
4.Incorporates risk due to insulin-resistant conditions such as metabolic syndrome
5.Does not include emerging risk factors such as CRP, lipoprotein(a), and apoB
a.All of the above
b.1, 3, and 5
c.1, 3, 4, and 5
d.None of the above
8.Based on the definition proposed by the NCEP ATP III guidelines, metabolic syndrome would be present if three or more of five criteria were present. Which of the following is NOT one of the criteria?
a.BP ≥130/≥85 or on treatment for hypertension
b.TGs ≥150 mg/dL
c.HDL-C of <40 mg/dL in men and women
d.Fasting glucose =100 mg/dL
e.Waist circumference of >40 inches in men and >35 inches in women
9.NCEP ATP III was published in 2001. Modifications to NCEP ATP III published in 2004 include all of the following except that
a.LDL-C goal <70 mg/dL is a therapeutic option for very high-risk patients.
b.LDL-C goal <70 mg/dL extends to patients at very high risk even with baseline LDL-C <100 mg/dL.
c.factors that favor the optional goal of <70 mg/dL include CVD plus multiple major risk factors (especially diabetes), severe and poorly controlled risk factors (especially smoking), metabolic syndrome, and acute coronary syndromes.
d.for moderately high-risk patients, LDL-C <100 mg/dL is an option with consideration of initiation of therapy with statins for LDL-C between 100 and 130 mg/dL.
e.both higher-dose statins and addition of fibrates and niacin to achieve non–HDL-C goals should be considered to achieve secondary targets and to further reduce cardiovascular event rate.
10.A 53-year-old obese, sedentary woman undergoes lipid screening, revealing TC of 310, TG of 720, HDL-C of 41. LDL-C was not calculated due to elevated TG. HbA1c is 5.9 and thyroid-stimulating hormone (TSH) is normal. NCEP ATP III guideline recommendations for TGs and HDL-C management include all but which of the following:
a.If TGs are ≥500 mg/dL, then TG is the primary target with use of therapeutic options to prevent pancreatitis including fibrates or niacin before LDL-lowering therapy, than treat LDL-C to goal.
b.In patients attaining LDL-C goals, those with TG ≥200 mg/dL have an increased cholesterol content of TG-rich, atherogenic lipoprotein particles. Non–HDL-C takes into account cholesterol in these and LDL particles and is a secondary target for therapy.
c.Therapeutic goal for TG is <150 mg/dL and for HDL-C is >40 in men and >50 in women.
d.HDL-C <40 mg/dL is defined as low and is a risk factor for CVD.
e.Non–HDL-C goal equals the LDL-C goal +30 mg/dL.
f.Combining a fibrate or nicotinic acid with an LDL-C-lowering drug can be considered.
11.Guidelines for management of dyslipidemia emphasize the importance of weight management, dietary choices, and exercise. TLC or Therapeutic Life Style Therapies for primary prevention of CVD include all of the following except
a.diet to reduce intake of saturated fats and dietary cholesterol with total fat range of 25% to 30% of total calories, saturated fat <7% of calories, and low intake of transfatty acids and <200 mg/day of cholesterol.
b.increased intake of plant stanols/sterols up to 2 g/day as a therapeutic option to reduce LDL-C.
c.increased intake of viscous (soluble) fiber to at least 5 to 10 g/day.
d.omega-3 polyunsaturated fatty acid supplements of 800 to 1,000 mg a day.
e.regular physical activity: >30 minutes five to seven times per week or enough moderate activity to expend at least 200 kcal/day.
f.weight loss to maintain BMI <25 kg/m2.
12.Secondary causes of dyslipidemia include all EXCEPT which of the following?
a.Hyperthyroidism
b.Obstructive liver disease/biliary cirrhosis
c.Renal disorders including nephrotic syndrome and chronic renal failure
d.Drugs including estrogen/progestins, protease inhibitors, anabolic steroids, corticosteroids, isotretinoin (Accutane®), and cyclosporine
e.Metabolic syndrome or diabetes mellitus (DM)
f.Pregnancy
13.According to NCEP ATP III, CHD risk equivalent defines high-risk individuals who would benefit from more intensive lipid-modifying therapies and include individuals with all of the following except
a.diabetes and additional cardiovascular risk factors.
b.FRS indicating a 10-year risk of MI or coronary death of >10%.
c.claudication with an ankle brachial index of 0.78.
d.individual status post aortic aneurysm endograft.
e.history of transient ischemic attack (TIA) followed by carotid endarterectomy.
Questions 14 to 16
You see a 52-year-old man with a history of type 2 DM on metformin. He has a history of hypertension controlled on amlodipine and an angiotensin-converting enzyme inhibitor. His BMI is 31.7 and waste circumference is 41 inches. His father had a coronary stent at the age of 54. He has the following fasting laboratory values:
Total C: 212 mg/dL
LDL-C: 120 mg/dL
HDL-C: 36 mg/dL
TG: 278 mg/dL
Non–HDL-C: 176 mg/dL
Glucose: 156 mg/dL
HbA1c: 7.6%
TSH: 1.2 mU/L
LFTs (liver function tests): WNL (within normal limits)
14.Based on NCEP ATP III and American Diabetes Association (ADA) guidelines, the most appropriate lipid goals for therapy in this patient are
a.LDL <70 mg/dL and non-HDL <100.
b.LDL <100 mg/dL and non-HDL <130.
c.LDL <70 mg/dL and non-HDL <130.
d.LDL <130 mg/dL and non-HDL <160.
15.Additional secondary goals for therapy in this patient based on these guidelines include
a.apoB <80 mg/dL.
b.apoB <90 mg/dL.
c.LDL particle number (LDL-P) <1,200.
d.LDL-P <1,000.
e.usCRP <2.
f.Answers a and d.
g.Answers a and e.
16.The best initial treatment for this patient’s dyslipidemia would be
a.atorvastatin 40 mg/day.
b.fenofibrate 148 mg/day.
c.extended release niacin 2,000 mg/day.
d.simvastatin 20 mg/day.
e.ezetimibe 10 mg/day.
f.omega-3 fish oil 4,000 mg/day.
17.The patient above was started on rosuvastatin 20 mg/day, metformin dose was increased, an aerobic exercise program was recommended, and he was referred for dietary advice. Repeat laboratory values in 4 months are as follows:
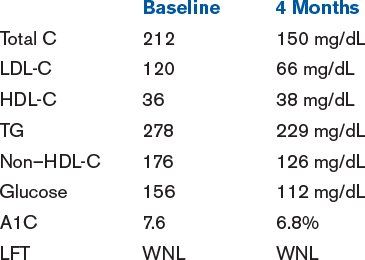
The most appropriate additional therapies recommended by NCEP ATP II at this time would include all but
a.nicotinic acid.
b.fenofibrate.
c.ezetimibe.
d.intensification of diet, exercise, and weight loss program.
e.intensification of statin therapy, increase rosuvastatin to 40 mg/day.
f.all of the above.
g.none of the above.
18.Patients such as the one above with diabetes are considered at high risk for CVD events. Which of the following statements is not true in regard to patients with diabetes?
a.Atherosclerosis accounts for approximately 65% to 75% of all diabetic mortality with 75% of these deaths due to coronary atherosclerosis.
b.A diabetic patient without a clinical history of prior MI or coronary artery disease (CHD) has a mortality rate from CHD and MI rate equal to a nondiabetic who has had a previous MI.
c.NHANES data from 2010 indicate that although goals of HbA1c <7 mg/dL, systolic BP <130 mmHg, and LDL-C <100 mg/dL are recommended for diabetics, only 32% of diabetics in the survey currently achieve all three of these goals.
d.Risk for atherosclerotic events is two- to fourfold greater in diabetics than in nondiabetics.
e.Atherosclerosis begins years to decades prior to diagnosis of type DM2 and >50% already have clinical CHD at the time of the diagnosis of DM.
19.Additional markers beyond standard risk factors have been shown to help reclassify risk assessment particularly in individuals in an intermediate-risk category (e.g., FRS of 10% to 20% or American College of Cardiology [ACC]/AHA guideline risk score of 5% to 7.5%). All but one of the following may be useful in hyperlipidemia treatment decisions:
a.usCRP
b.LDL-P
c.Coronary artery calcification score (CACS)
d.HDL particle size and number
e.Lipoprotein(a)
20.Major differences in the ACC/AHA hyperlipidemia treatment guidelines of 2013 compared with NCEP ATP III recommendations include all of the following except
1.elimination of LDL-C and non–HDL-C targets for therapy.
2.a focus on risk reduction targeting therapy to four major groups demonstrated to benefit from statin therapy based on RCT data rather than targeted to risk category and LDL-C level.
3.replacing the FRS with a newly developed risk calculator that includes ethnicity and family history and broadens the outcome events to include stroke.
4.that since the absolute benefit in CVD risk reduction is proportional to the baseline risk of the individual and to the intensity of statin therapy, treatment is focused on intensity of statin treatment and does not recommend use of low-dose statin therapies.
5.that decreasing statin dose is reasonable if LDL-C on therapy is <40 mg/dL.
a.None, all are true
b.1, 3, and 5
c.3 and 5
d.All are not true
e.3, 4, and 5
21.The ACC/AHA hyperlipidemia guidelines of 2013 identify four groups shown to benefit from high-intensity and moderate-intensity statin therapy for use in secondary and primary prevention of CVD. High-risk individuals who would be a candidate for high-intensity statin therapy for LDL-C lowering would include all except
a.those with clinical atherosclerotic cardiovascular disease (ASCVD).
b.primary elevations of LDL-C ≥160 mg/dL.
c.individuals with diabetes aged 40 to 75 years with LDL-C 70 to 189 mg/dL without clinical ASCVD and with ASCVD risk ≥7.5%.
d.without clinical ASCVD or diabetes with LDL-C 70 to 189 mg/dL and estimated 10-year ASCVD risk ≥7.5%.
22.The American Academy of Pediatrics (AAP) 2008 lipid management recommendations for children and teenagers include all of the following except
a.screening as early as 2 years of age in setting of family history of CVD or hyperlipidemia.
b.lower LDL cut points for initiation of treatment dependent on risk level.
c.bile acid sequestrants as initial therapy in younger patients under 16 years of age.
d.considering initiation of therapy as early as 8 years of age in high-risk children.
e.emphasis on overweight, high TG, and low HDL managed with lifestyle interventions and weight management.
f.fiber up to 20 g/day and use of dietary plant stanols/sterols.
23.In decisions regarding screening for and treating hyperlipidemia in children and adolescents, it is important to remember that all of the following are true except that
1.cholesterol is lowest intrauterine and at birth.
2.concentrations are similar to young adult levels by 2 years of age with strongest relation to adult levels at 5 to 10 years and 17 to 19 years.
3.cholesterol levels decrease from 10% to 20% during pre-pubertal and pubertal development.
4.low-fat diets should not be implemented until after age 5 years.
5.statins have not been shown to have an adverse effect on sexual or physical maturation.
6.impact on the atherosclerotic process and clinical outcomes has been demonstrated with statin treatment in children and adolescents.
a.None of the above
b.2, 4, and 6
c.4 and 6
d.3, 5, and 6
e.All of the above
24.Although statin therapy and LDL-C reduction is the main thrust of pharmacologic therapies, there has been an interest in treating beyond LDL-C with other therapies directed toward HDL-C and TG to further reduce CVD events. This concept is supported by the following observations except that
a.cardiovascular events occur in individuals with treated LDL-C even after aggressive LDL lowering with statins.
b.patients with diabetes studied in clinical trials on statins have CVD event rates higher than the CVD event rates of those patients without diabetes on placebo.
c.intravascular ultrasound (IVUS) studies have shown LDL-C <70 to 80 mg/dL to be associated with plaque regression but the 20% of individuals that progress on therapy often have DM, less increase in HDL, and less decrease in apoB on treatment.
d.the action to control cardiovascular risk in diabetes clinical trial (ACCORD) trial demonstrated a benefit of fenofibrate when added to baseline simvastatin therapy in diabetic patients.
e.observational studies have noted an impact of low/abnormally functioning HDL, VLDL remnants, elevated TG small dense LDL, LDL-P, and apoB/apoA ratios on adverse outcomes.
f.epidemic of obesity, diabetes, and metabolic syndrome associated with dyslipidemia is marked by only modest elevations in LDL-C but increases in HDL-C and TG.
25.In the setting of strong observational and epidemiologic data supporting HDL-C’s relationship to CVD risk, the limitations of current therapies, and the increase in incidence of diabetes/metabolic syndrome, there remains a strong interest in focusing on other therapeutic interventions in addition to LDL-C lowering, particularly HDL modulation. HDL is more than a simple carrier of cholesterol. Which of the following statements regarding HDL-C metabolism and function is not true?
a.In addition to reverse cholesterol transport, HDL may have beneficial effects due to antioxidant and anti-inflammatory effects.
b.ATP-binding cassette transporter 1 (ABCA1) and ABCG1 both facilitate free cholesterol efflux to lipid-poor pre-β1-HDL.
c.Cholesteryl ester transfer protein (CETP) enables exchange of cholesterol esters for TGs between HDL and apoB-containing lipoproteins (LDL and VLDL).
d.HDL can deliver cholesterol to the liver via both direct and indirect reverse cholesterol transport.
26.Since most lipid-lowering guidelines emphasize the use of statin therapy and at potent doses in the highest-risk individuals, it is important to recognize side effects. Clinically significant adverse effects of statins include all of the following except
a.muscle-related adverse events.
b.liver-related adverse events.
c.renal insufficiency.
d.headaches.
e.dyspepsia.
27.You see a 68-year-old woman recently started on a statin for a calculated FRS of 18% 10-year risk and elevated usCRP. She returns in 6 weeks complaining of left lower extremity aching, which she had not experienced before. Regarding muscle-related side effects with statin drugs, all of the following statements are true except that
a.myopathy occurs in approximately 0.1% to 0.5% of patients on statin monotherapy and is dose dependent.
b.the incidence of statin-associated rhabdomyolysis across large, randomized, controlled statin trials is <0.1% and the reported incidence of fatal rhabdomyolysis with statins is extremely rare with 0.15 death per 1 million prescriptions.
c.a review of five large-scale controlled clinical trials of statin safety reported a rate of myopathy ranged from 0.1% to 0.6% and rate of rhabdomyolysis ranged from 0.03% to 0.05%.
d.myalgia symptoms reported in prescribing information range from 5% to 10%.
e.identifying factors that may contribute to myopathy should lead to statin dose reduction.
28.For the patient in Question 27, you obtain a creatine phosphokinase (CPK) which is 282 (upper normal in laboratory of 220 U/L). No baseline CPK is available for comparison. She has no reproducible pain or weakness on examination. She denies darkening of the urine. Should you stop the statin?
a.Yes
b.No
29.You see a 49-year-old obese, sedentary woman with type 2 DM, hypertension, and family history of coronary stent in her father at age 53. LDL-C was 173 mg/dL. Based on NCEP ATP III and 2013 ACC/AHA guidelines she is a candidate for intensive statin therapy. Laboratory values obtained 3 months after treatment with 40 mg of atorvastatin revealed alanine transaminase (ALT)/aspartate transaminase (AST) of 102/96 (upper normal in laboratory of 50/42 U/L). Which of the following regarding liver abnormalities with statin use is not true?
a.Reversal of transaminase elevation is frequently noted with continuation of statins or a reduction in statin dose.
b.Elevations do not often recur with either readministration or selection of another statin.
c.Statins have been shown to worsen the outcome in persons with chronic transaminase elevations due to hepatitis B or C.
d.In this patient review other drugs and supplements, continue the current dose, and repeat in 6 to 12 weeks.
e.Baseline measurement of ALT should be performed before starting therapy.
30.Later that afternoon you are referred a 58-year-old man with waist circumference of 42 inches, fasting glucose of 112 mg/dL, hypertension, current smoker with brother with MI at age 54. LDL-C is 163 mg/dL, TG 275 mg/dL, and HDL-C 47 mg/dL. When first seen prior to initiation of any therapy, he had LFTs similar to those reported for the patient in the previous question (approximately two times upper limit of normal [ULN]). The patient is very worried about taking statins due to concerns of liver failure. Which of the following can you tell him? 10 year risk by Framingham Risk Score is >30% and ACC/AHA calculator score is 21.2.
a.Statin use has not been investigated in patients with baseline LFT abnormalities but should be used due to his high risk.
b.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


