Fig. 28.1
Operative exposure of the right popliteal artery shunted with a long external (or looped) Sundt© vascular shunt in the presence of concomitant orthopedic injury (not visualized)
The wars in Afghanistan and Iraq demonstrated the military’s ability to manage complex extremity vascular injuries in austere environments including those of the Forward Surgical Team (FST). In this setting, temporary vascular shunts were found to be useful in lieu of prolonged extremity ischemia associated with continued tourniquet application or vessel ligation. Vascular shunts were found to be an effective tool to restore extremity flow (arterial and venous) upon exploration and control of vascular injuries at these more remote locations. In these scenarios, shunts were secured in the vessel(s), the wound partially closed, and the patient evacuated to a higher level of care typically within 45–90 min (Fig. 28.2). At these higher levels or echelons of care, the patient arrived with a perfused limb and the vascular shunt was removed and vascular reconstruction performed [20, 21]. This same sequence may also be effective in the civilian setting where temporary vascular shunts should be considered by less experienced surgeons or those at more rural hospitals. In these instances, a vascular shunt should be placed and secured upon exploration of the vascular injury and the patient evacuated to a larger hospital with expertise in vascular reconstruction.
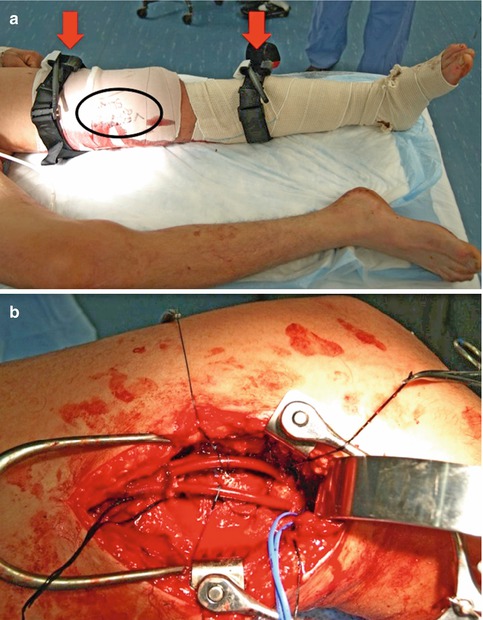
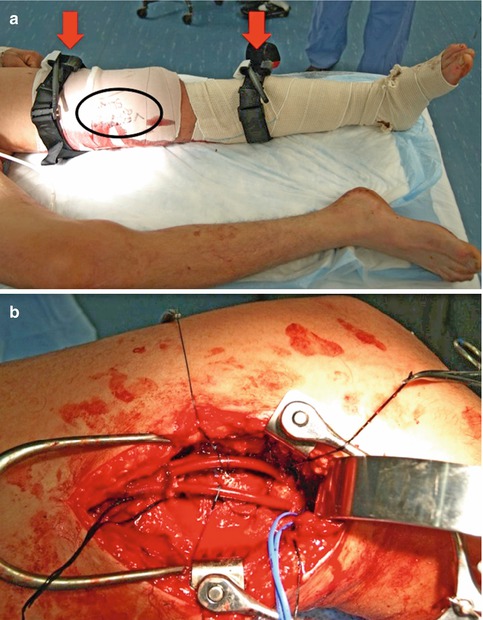
Fig. 28.2
(a) After sustaining a penetrating injury to the left thigh, a patient was initially treated with arterial and venous shunting as indicated on the dressing (circled). Additionally, tourniquets (arrows) were loosely applied and available in the case of shunt dislodgement. (b) Operative exposure of the same patient demonstrating in-line vascular shunts in the femoral artery and vein secured with silk sutures and a silastic loop
The third indication for a temporary vascular shunt is in the setting of a patient with extremity vascular injury and other life-threatening injuries and/or severely compromised physiology. In these instances, the vascular shunt is applicable as part of an overall damage control resuscitation strategy allowing for extremity perfusion and reduction of ischemic burden while the patient is resuscitated or other life-threatening injuries are managed. Depending upon the injury scenario, the temporary vascular shunt may be placed prior to or concomitant with laparotomy, thoracotomy, craniotomy, or other procedure. The shunt may remain in place for 12–24 h while the patient is resuscitated and vascular repair can be considered. In rare multiple casualty scenarios which outstrip operating capacity, vascular shunts have been used as an expeditious way to restore extremity perfusion and clear an operating table. In such cases the patient is monitored in the intensive care unit until additional operating room space becomes available and the shunt can be removed in favor of vascular reconstruction.
Finally, vascular shunts are indicated in scenarios of mangled extremity with ischemia or in cases of an extremity amputation in which reimplantation is attempted. As stated previously, vascular injury exploration and shunt placement should take priority in these scenarios to reduce the neuromuscular ischemic time. Once vascular flow is reestablished, then the associated extremity fracture or amputation can be carefully stabilized. In these and other scenarios, vascular shunts are often useful in the extremity vein as well as the artery.
28.4 Timing: When to Apply and for How Long
Shunts should be considered at the time of vascular injury exploration. Once in place shunts have remained patent without systemic anticoagulation for as long as 52 h. However, experience shows that most shunts are in place for 4–6 h and that the risk of shunt-related complications such as thrombosis or thromboemboli increases after 12 h [22]. Shunts which are used in larger vessels (axillary-brachial and femoral-popliteal) have a greater patency than those placed in small, distal vessels (forearm and tibial). In most instances patency of large proximal vascular shunts is maintained without systemic anticoagulation, which is often contraindicated in trauma. Even in cases where anticoagulation is not possible, local and regional heparinized saline (1,000–10,000 units/l) should be used to reduce platelet aggregation and thrombus formation at the time of shunt placement. It is the authors’ observation that a low level of systemic anticoagulation is necessary to maintain patency in a shunt used in small, distal arteries. Experience from the war in Iraq showed that despite a higher rate of thrombosis, use of shunts in distal arteries did not detract from overall limb salvage.
28.5 Technical Considerations
Use of a temporary shunt begins with exposure and control of the vascular injury. In the extremity this may be facilitated with the use of tourniquets in order to temporarily control hemorrhage. If there is no bleeding from a wound, the tourniquet may not be necessary and control can be gained by operative exposure at or just proximal to the site of injury. Control of mesenteric vascular injuries can usually be obtained at or just proximal to the site of hemorrhage although control of the aorta above the celiac artery may be necessary. Once broad control of bleeding and the injury site is obtained, the exact site of the disrupted vessel(s) should be exposed. Dissection of the proximal and distal aspects of the injured vessel(s) is performed, and these segments are gently encircled with silastic vessel loops. One can next determine the extent of the injury which may range from a contusion with varying degrees of occlusion to transection of the vessel. At this stage in the operation, the surgeon must determine his or her mode of management: ligation, placement of a shunt, or vascular reconstruction. As previously noted, this decision depends on several factors including anatomic location of the vascular injury, physiological status of the patient, the experience of the surgeon, and the capacity of the medical facility in which the operation is taking place.
Before placing the vascular shunt, the open edges of the injured segment must be exposed and flow established using a combination of Fogarty thromboembolectomy catheters and flushes of heparinized saline. These steps establish proper inflow and outflow of the injured segment, and failure to do so equates to placing the shunt in an occluded vascular segment with no perfusion. At the least, the proximal inflow vessel must be opened, allowing brisk bleeding and flushing of platelet aggregate or thrombus. Regional heparinized saline should also be flushed in the injured vascular segment including the inflow and outflow using a soft plastic catheter or a metallic infusion instrument such as a St. Mark’s injection tip. If there are no serious concomitant injuries, systemic anticoagulation should considered at this point as well.
Once the edges of the vascular segment have been debrided such that there is space to place the shunt, the distal end should be inserted and allowed to bleed in a retrograde fashion (i.e., “back bleed”). When grasping the shunt for positioning and insertion, it is important not to grasp too aggressively or to crimp the shunt. While most shunts are robust and resist impingement on their inner lumen, some have a wire lining which can be deformed with too aggressive of handling. Crushing or crimping of the internal lumen will result in restriction of flow and early thrombosis or occlusion. The depth of insertion will depend upon the length of the shunt as well as the length of the vascular defect.
Once the distal end of the shunt is placed, the proximal aspect of the vascular injury should be allowed to flush (i.e., “fore bleeding”), clearing any elements of platelet debris or thrombus. The proximal end of the shunt is then placed into this segment and perfusion established. Gentle release and then retraction of the silastic vessel loops at the proximal and distal aspects of the vascular injury are helpful in placement and securing of the device. If the vessel has contracted and the lumen significantly reduced in size, insertion can be facilitated by use of a small right-angled dissecting device inserted into this lumen and opened to spread or gently dilate the intended insertion site. Although the shunt should not be inserted any deeper than is necessary to secure it into a true luminal position, the important point is to make this step as easy and fluid as possible. Because the short, in-line shunts are not designed to loop, they often require deeper insertion in order to easily position the opposite end. In contrast, the longer, looped shunts tend to be more flexible and accommodating of very minimal insertion depth. Once the shunt is in the desired location and flow confirmed with continuous wave Doppler, it can be secured using silk ties around the edges of the vessel in which it is inserted.
28.6 Types of Shunts
Shunts used for vascular injury today were originally designed to provide cerebral perfusion during carotid endarterectomy and include (among others) the Sundt©, Javid©, Pruitt-Inahara©, and Argyle©. These devices have varying inner diameters ranging from 1.9 to 5.7 mm and fall into two categories including the short “in-line” and the long “external” or “looped” shunts (Table 28.1). The Sundt© shunt (Fig. 28.3) is a silicone elastomer reinforced with a spiral stainless steel wire within the wall to prevent kinking. The Sundt© has atraumatic bulb-tipped insertion ends and comes in a short (10 cm) in-line and a long (30 cm) external or looped design. The Javid© (Fig. 28.4) is a long, external shunt composed of a polished polymer and tapered ends to allow atraumatic insertion. The Pruitt-Inahara© (Fig. 28.5) is a long, external shunt made out of polyvinyl chloride and secured inside the vessel lumen by inflatable balloons on the proximal and distal ends. The Pruitt-Inahara© also has a side port that may be used for transducing blood pressure or infusing therapeutics. The Argyle© (Figs. 28.6 and 28.7) is a polyvinyl chloride in-line shunt available in 15 or 28 cm lengths. Each container of Argyle© shunts contains 8, 10, 12, and 14 Fr diameters. These shunts have all performed equally well with regard to insertion and patency in the military and civilian settings over the past decade. The choice of shunt may be left to the surgeon, but any of these commercially manufactured devices are preferred over improvised devices such as chest tubes, nasogastric tubes, or even intravenous tubing [23].
Table 28.1
Summary of commonly available temporary vascular shunts
Shunt model | Manufacturer | Style | Proximal diameter | Distal diameter | Length (cm) |
|---|---|---|---|---|---|
Sundt© | Integra LifeSciences | In-line or looped | 2.1–3.1 mma | 1.3–2.2 mma | 10, 30 |
3.9–5 mm | 2.7–4 mm | ||||
Javid© | Bard Peripheral Vascular | Looped | 17 Fr | 10 Fr
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|