Glycated hemoglobin (HbA1c) is an approved and widely used laboratory investigation for diagnosis of diabetes that is not affected by acute changes in blood glucose. Our aim was to analyze the extent to which routine HbA1c measurements diagnose unknown diabetes mellitus (DM) in patients presenting with ST-segment elevation myocardial infarction (STEMI). We also compared outcomes in patients with newly diagnosed DM, previously established DM and those without DM. Consecutive patients undergoing PCI for STEMI from January 2005 to December 2012 were included and routinely performed admission HbA1c was used to identify patients with previously undiagnosed DM (HbA1c ≥6.5 and no history of DM or DM therapy) and pre-DM (HbA1c 5.7% to 6.4%). Overall 1,686 consecutive patients underwent primary percutaneous coronary intervention for STEMI during the study period and follow-up data were available for 1,566 patients (90%). A quarter of the patients (24%, n = 405) had history of DM, 7% (n = 118) had previously undiagnosed DM, and 38.7% (n = 652) had pre-DM. Mortality was comparable in patients with known DM and newly diagnosed DM both in-hospital (11.1% vs 11.9%, p = 0.87) and at 3-year follow-up (27.3% and 24%). Patients with DM, including those who were newly diagnosed, had higher mortality at 3 years (26.5%) compared to those with pre-DM (12.1%) or no dysglycemia (11.2%, p <0.01). In conclusion, a substantial number of patients with STEMI have previously undiagnosed DM (7%). These patients have similar in-hospital and long-term mortality as those with known DM, and outcomes are inferior to patients without dysglycemia.
An estimated 387 million subjects or 8.3% of the global population have diabetes mellitus (DM), and nearly half of them are unaware of their diagnosis. Cardiovascular disease resulting from atherosclerotic complications of DM is the foremost contributor to mortality in patients with DM. Abnormal glucose tolerance is significantly more common in subjects with coronary artery disease (CAD), and patients with a history of myocardial infarction (MI) have twice the annual incidence of insulin resistance compared to subjects with no history of MI. This leads some clinicians to suspect that MI may be a pre-DM equivalent. Indeed, standard guidelines recommend routine screening for DM and pre-DM in patients with CAD. Previous data using oral glucose tolerance test (OGTT) suggest that 1/4 of patients with MI may have undiagnosed DM and another 40% may have impaired glucose tolerance or pre-DM. However, difficulty in performance and the presence of stress hyperglycemia in an acutely ill patient with MI make OGTT a rarely used diagnostic test in this setting. Since 2010, glycated hemoglobin (HbA1c) has been recognized by the World Health Organization and American Diabetes Association as a point-of-care test for diagnosis of DM (≥6.5%) and pre-DM (5.7% to 6.4%). Our aim was to assess the yield of HbA1c testing in identifying as yet undiagnosed DM in patients presenting with an ST elevation myocardial infarction (STEMI). We also sought to evaluate the implications of the new diagnosis of DM and compare outcomes in patients with known DM or no dysglycemia.
Methods
We included all patients who underwent primary percutaneous coronary intervention (PCI) for STEMI at a single, large, tertiary care institution from January 2005 to December 2012. Baseline characteristics, cardiac history, risk factors, medications, other preexisting chronic medical conditions, angiographic, and procedural data were obtained from the institutional review board approved institutional PCI registry. Patients with history of DM were identified based on International Classification of Diseases , Ninth Revision diagnosis or the use of DM therapy (oral hypoglycemic drugs or insulin) before admission. Routinely performed glycated hemoglobin (HbA1c) on day of admission was used to classify patients as having previously undiagnosed DM (HbA1c ≥6.5 and no history of DM or DM therapy) or pre-DM (HbA1c 5.7% to 6.4%). In patients in whom HbA1c was not available (n = 140, 8.3%), fasting plasma glucose on day of discharge was used to classify patients in the aforementioned categories (≥126 mg/dl as DM and 101 to 125 mg/dl as pre-DM). Follow-up data were obtained from the institutional PCI registry.
Continuous variables are presented as mean with SD or median with interquartile range, and categorical variables are presented as percentage affected. Fisher’s exact test for categorical variables and Wilcoxon rank order test for continuous variables were used to compare differences in groups. We calculated the time-to-event according to the date of the initial index procedure for both single and staged procedures. We used the Kaplan–Meier method to assess the proportion of patients who died during follow-up for time-to-event analysis. A risk-adjusted analysis was also performed after adjusting for age and gender. Log-rank tests were used to compare Kaplan–Meier curves plotted for cumulative survival. Finally, sensitivity analysis were done after excluding patients who did not have an HbA1c on admission and additionally after classifying all patients with HbA1c ≥6 as having newly diagnosed DM. All tests were 2-tailed and a p value of <0.05 was considered significant. Statistical calculations were done in SAS, version 9.2, (SAS Institute Inc., Cary, North Carolina).
Results
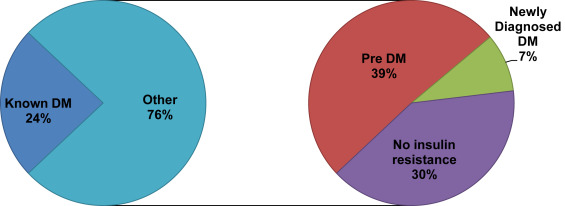
Mean age of the overall population was 60 years, and 67% (n = 1,136) were men ( Table 1 ). An admission HbA1c was performed in 92% (n = 1,546) of patients undergoing primary PCI for STEMI. Glycemic abnormalities were detected in nearly 70% (n = 1,175) of these patients and about a quarter (24%, n = 405) of patients had an established history of DM. Using admission HbA1c, we diagnosed an additional 7% (n = 118) of subjects with DM (newly diagnosed DM) and another 39% (n = 652) with pre-DM ( Figure 1 ).
| Variable | Total Patients (N=1,686) | Known DM (n=405) | Newly diagnosed DM (n=118) | Pre-DM (n=652) | No Insulin resistance(n=511) | P- value ∗ |
|---|---|---|---|---|---|---|
| Age (years) | 60.4 ± 13.2 | 62.8 ± 12.4 | 62.2 ± 14.5 | 60.5 ± 12.8 | 58.1 ± 13.6 | <0.001 |
| Male | 67.4% | 59.0% | 65.3% | 67.9% | 74.0% | <0.001 |
| Body Mass Index (Kg/m 2 ) | 29.3 ± 6.3 | 31.5 ± 7.0 | 30.5 ± 6.4 | 28.8 ± 6.0 | 28.0 ± 5.4 | <0.001 |
| Dyslipidemia | 66.1 % | 81.9% | 61.3% | 64.7% | 56.4% | <0.001 |
| Hypertension | 69.9% | 88.1% | 74.6% | 67.5% | 57.5% | <0.001 |
| Smoker (current or former) | 72.5% | 70.4% | 60.4% | 75.8% | 71.8% | 0.038 |
| Glycated Hemoglobin, mean ± SD | 6.4 ± 1.51 | 8.0 ± 2.0 | 7.5 ± 1.3 | 5.9 ± 0.2 | 5.3 ± 0.3 | <0.001 |
| Admission glucose, (mg/dl) ± SD | 158.9 ± 82.3 | 225 ± 103 | 191 ± 89 | 137 ± 66 | 128 ± 37 | <0.001 |
| Infarct Related Artery (%) | ||||||
| Left Anterior Descending | 662(39.3%) | 174 (43%) | 50 (42.4%) | 222 (34.0%) | 216 (42.3%) | NS |
| Left Circumflex | 275 (16.3%) | 57 (14.1%) | 18 (15.3%) | 120 (18.4%) | 80 (15.6%) | |
| Right Coronary Artery | 732 (43.4%) | 168 (41.5%) | 49 (41.5%) | 305 (46.8%) | 210 (41.1%) | |
| Left Main Trunk | 17 (1%) | 6 (1.5%) | 1 (0.8%) | 5 (0.8%) | 5 (1.0%) | |
Patients with DM (known or newly diagnosed) tended to be older, had greater body mass index, and a higher incidence of traditional risk factors such as hypertension and hyperlipidemia than those without DM ( Table 1 ). HbA1c and admission glucose were highest in those with known DM, followed by newly diagnosed DM, pre-DM, and no dysglycemia, respectively.
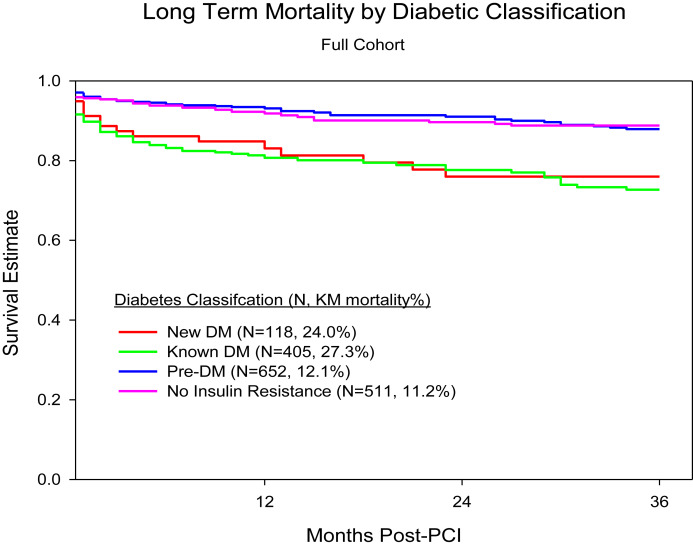
In-hospital mortality was comparable between those with known DM (11.1%) and newly diagnosed DM (11.9%), with both being significantly higher than those with pre-DM (4.1%) or no insulin resistance (4.7%). Mortality at 3 years was highest in patients with known DM (27.3%), followed by those with newly diagnosed DM (24%). Mortality rates were comparable in groups with pre-DM (12.1%) and no insulin resistance (11.2%), with both being significantly lower than groups with DM (known or newly diagnosed; Figure 2 ). At discharge, DM therapy (insulin or oral agents) was prescribed for 80% of patients with known DM and 25.4% of patients with newly diagnosed DM ( Table 2 ). A sensitivity analysis including only patients with an admission HbA1c revealed similar results. We also performed a sensitivity analysis after classifying all patients with HbA1c ≥6.0 as newly diagnosed DM and noted that mortality at 3 years was highest in the group with known DM (27%, n = 111 of 405) followed by those with newly diagnosed DM (17%, n = 63 of 371) and pre-DM (9%, n = 34 of 399).
| Variable | Known DM (n=405) | Newly diagnosed DM (n=118) | Pre-DM (n=652) | No Insulin Resistance (n=511) |
|---|---|---|---|---|
| In-hospital death | 45 (11.1%) | 14 (11.9%) | 27 (4.1%) | 24 (4.7%) |
| Death at 3 years | 111 (27.4%) | 28 (24.0%) | 79 (12.1%) | 57 (11.2%) |
| Unadjusted Hazard Ratio for death at 3 years (95% CI) | 2.55 (1.8 – 3.7) | 2.10 (1.2 – 3.6) | 1.07 (0.6 – 1.4) | 1.0 |
| Adjusted Hazard Ratio ∗ for Death at 3 years (95% CI) | 2.1 (1.5 – 3.1) | 1.7 (1.0- 3.0) | 0.9 (0.6 – 1.3) | 1.0 |
| Discharged on diabetic therapy (insulin or oral hypoglycemic agent) | 324 (80%) | 30 (25.4%) | 11 (1.7%) | 0 (0%) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


