Recoarctation of the aorta (RCoA) is a major cause of morbidity and mortality after the Norwood procedure. We sought to identify transthoracic echocardiographic (TTE) indexes associated with RCoA and to develop a highly sensitive and specific diagnostic score for accurate diagnosis. All subjects who underwent a Norwood procedure from December 2005 to December 2009 were identified. Subjects were excluded if they did not undergo a TTE within 1 month of an outcome-defining event (cardiac catheterization, autopsy, or surgery). RCoA was defined as arch intervention at catheterization or surgery or findings of RCoA at autopsy. Of 113 subjects included for analysis, RCoA occurred in 19 (17%). All TTE indexes were significantly associated with RCoA in univariate testing. In the final multivariate model, peak isthmus velocity >2.5 m/s (p <0.001), coarctation index, defined as the ratio of the narrowest region of the descending thoracic aorta to the distal descending thoracic aorta diameter <0.7 (p <0.01), and decrease in ventricular systolic performance (p = 0.03) were all significantly associated with RCoA. A composite score was developed using a peak velocity of >2.5 m/s (2 points), coarctation index <0.7 (1 point), and a decrease in ventricular systolic performance (1 point). A score of ≥2 diagnosed RCoA with 100% sensitivity and 85% specificity. The score performed equally well regardless of shunt type. In conclusion, a composite score of TTE indexes accurately discriminates RCoA in patients who have undergone the Norwood procedure.
The Norwood procedure is performed as a neonatal palliative procedure for children born with hypoplastic left heart syndrome (HLHS) and other single-ventricle anomalies. Morbidity and mortality after the Norwood procedure has improved in the recent era of surgery, yet remains among the highest of all congenital heart defects.
One of the most important causes of morbidity and mortality is recoarctation of the aorta (RCoA), which occurs in up to 37% of patients. In the setting of RCoA, patients with HLHS are at risk for ventricular dysfunction, atrioventricular valve regurgitation, and decreased systemic perfusion. RCoA is challenging to diagnose by transthoracic echocardiography (TTE), and current methods lack sensitivity and specificity. The current gold standard to diagnose RCoA is cardiac catheterization, which has potential risks in this patient population and often is not performed until there is a clinical suspicion of RCoA.
We sought to identify TTE measures that accurately discriminate RCoA and to create a clinical diagnostic rule with high sensitivity and specificity. Furthermore, we sought to determine if the diagnostic rule’s performance varied based on shunt type.
Methods
The study protocol received institutional review board approval. Subjects who underwent a Norwood procedure from December 2005 to December 2009 at our institution were identified through a query of our surgical database. We excluded patients from analysis if they did not undergo a TTE at our institution within 1 month of an outcome-defining event. Outcome-defining event included RCoA diagnosed at cardiac catheterization, autopsy, or direct surgical inspection. Demographic data and preoperative factors that might be associated with RCoA were recorded from echocardiographic and clinical databases, including gender, age at surgery, gestational age, presence of a chromosomal anomaly, size of the ascending aorta, and subtype of HLHS. Perioperative data recorded from surgical databases included the type of shunt used during the Norwood procedure (Blalock-Taussig shunt [BTS] or right ventricle-to-pulmonary artery shunt). For subjects with multiple cardiac catheterizations, the first procedure was used for analysis. In addition to the TTE performed within 1 month of the outcome study, previous TTE studies were used to assess for change in ventricular performance and atrioventricular valve regurgitation over time.
TTE studies performed within 1 month of an outcome-defining event were analyzed. Data were recorded from previously obtained images stored in a recorded database (syngo Dynamics; Siemens, Ann Arbor, Michigan). The echocardiographic studies were performed using a Philips (Andover, Massachusetts) echocardiographic system with appropriate phased array transducers for the size of the patient. The right ventricular systolic performance was assessed in the apical 4-chamber and parasternal short-axis views, providing orthogonal planes. The aortic arch was assessed in the suprasternal notch view with 2-dimensional, color flow, pulse-wave and continuous-wave Doppler interrogation along the length of the aorta. Tricuspid valve regurgitation was subjectively quantified in the apical 4-chamber view and parasternal long-axis views.
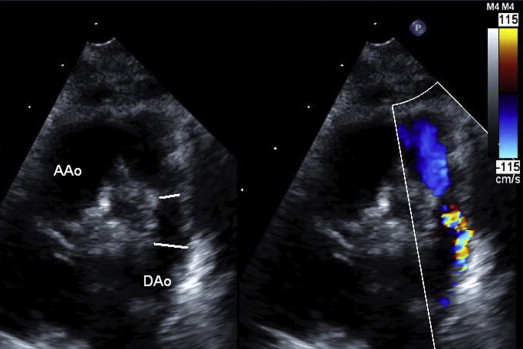
The principal investigator, blinded to outcome, measured the echocardiographic indexes. TTE data collected included the peak velocity and mean gradient across the aortic arch by continuous-wave Doppler, absolute measurements of the narrowest portion of the aorta at the level of the isthmus, evidence of aliasing of flow at the level of the aortic isthmus, calculation of the coarctation index (CI; ratio of the narrowest portion of the descending thoracic aorta to the distal descending thoracic aorta, Figure 1 ), a change of at least 1 grade in atrioventricular valve regurgitation, and/or right ventricular systolic performance. Interobserver reliability of all measures was assessed by a senior echocardiographer on 20% of the cohort.
Cardiac catheterization or findings at autopsy or surgery were used to define the outcome of RCoA. During the study period, cardiac catheterization was performed as part of the routine preoperative assessment before the cavopulmonary anastomosis or if there was a change in clinical status requiring further investigation. The first cardiac catheterization performed after the Norwood procedure was used as the outcome-defining event. A positive outcome by cardiac catheterization was defined as a balloon dilation of the descending aorta. This decision was made at the discretion of the physician performing the cardiac catheterization. Typically, the assessment for RCoA consisted of measurement of the pressure gradient from ascending to descending aorta by either simultaneous or pullback pressure measurements. In addition, anatomic assessment of aortic arch narrowing was made by power injection cineangiography. Interventions are typically performed based on the presence of a significant pressure gradient (≥10 mm Hg in the presence of a normal cardiac output) or a significant angiographic narrowing (≥50% stenosis compared with the diameter of the descending aorta). If cardiac catheterization was not performed, a positive outcome was also defined as a surgical intervention on the descending aorta or findings of RCoA at autopsy.
Descriptive statistics were used to summarize the preoperative and demographic characteristics of the cohort. The mean and SD were used to summarize normally distributed continuous variables, median and range were used to summarize skewed continuous variables, and frequency was calculated for categorical variables. Logistic regression analysis was performed to assess for associations between demographic and preoperative factors and the development of RCoA. Logistic regression was also used to identify potential TTE indexes significantly associated with RCoA. A final multivariate model was built to identify the significant independent echocardiographic indexes diagnostic of RCoA. Echocardiographic indexes with p values <0.2 in univariate testing were considered for inclusion in the final multivariate model in a forward stepwise fashion and retained if the resultant p value was <0.05.
A clinical diagnostic rule was developed using the echocardiographic indexes included in the final multivariate model. Point values for each component of the score were assigned based on the magnitude of the odds ratio. Receiver operating characteristic analysis was used to identify the cut point for the diagnostic score that maximized specificity while maintaining a minimum sensitivity of at least 90%.
Assessment for interrater reliability of the TTE indexes was performed on a randomly selected 20% of the cohort. Kappa scores were calculated for dichotomous variables, and intraclass coefficient was calculated for continuous variables. Kappa scores were defined as high agreement if they were >0.8 and substantial agreement if they were from 0.6 to 0.8. Definitions for intraclass coefficient correlations included high agreement for a score >0.7 and moderate for 0.4 to 0.7.
Results
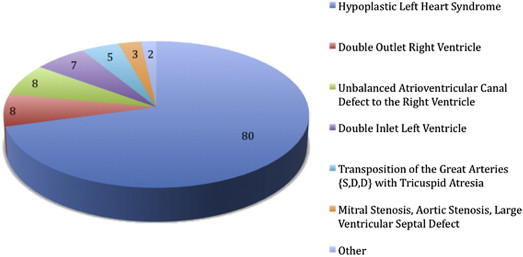
Of 174 subjects who underwent the Norwood procedure during the study period, 113 (64.9%) were included in the study. Subjects were excluded for the following reasons: no TTE within 1 month of an outcome-defining event (21), death without autopsy before an outcome-defining event (18), follow-up at an outside institution (13), no cardiac catheterization performed (4), no evaluation of the aortic arch (4), and intraoperative death without autopsy (1). The clinical and demographic characteristics of the cohort are listed in Table 1 . The anatomic subtypes of study subjects are detailed in Figure 2 . Of the 113 subjects included for analysis, 19 (17%) developed RCoA. All subjects with RCoA were diagnosed by cardiac catheterization, and none were diagnosed with RCoA at autopsy or by surgical inspection. Of the 113 subjects who met the inclusion criteria, 81 (71.7%) underwent surgical palliation with a BTS only, 23 (20.3%) with a right ventricle-to-pulmonary artery shunt only, and 9 (8%) had both a BTS and a right ventricle-to-pulmonary artery shunt. There was no difference in the incidence of RCoA between the 2 shunt types.
| Variable | Total Cohort (n = 113) | Recoarctation of the Aorta (n = 19) | No Recoarctation of the Aorta (n = 94) | p-Value |
|---|---|---|---|---|
| Female | 46 (41%) | 6 (32%) | 40 (43%) | 0.37 |
| Age at Norwood (days) | 3 (0–39) | 4 (1–8) | 3 (0–39) | 0.62 |
| Prematurity | 11 (10%) | 5 (26%) | 6 (7%) | 0.01 |
| Ascending aorta <2 mm | 32 (31%) | 8 (47%) | 24 (28%) | 0.13 |
| Hypoplastic left heart syndrome | 80 (71%) | 14 (74%) | 66 (70%) | 0.76 |
| Blalock-Taussig shunt | 88 (79%) | 13 (72%) | 75 (79%) | 0.47 |
The associations between TTE indexes and RCoA are summarized in Table 2 . The final multivariate model included peak velocity across the aortic arch of >2.5 m/s, CI <0.7, and decrease in right ventricular systolic performance. Based on the multivariate model, the covariates included in the clinical diagnostic score were as follows: peak velocity across the aortic arch of >2.5 m/s (2 points), CI <0.7 (1 point), and worsening right ventricular systolic performance (1 point). A score of ≥2 points accurately discriminated RCoA with a sensitivity of 100% and a specificity of 85% ( Table 3 ). The receiver operating characteristic curve is shown in Figure 3 with an area under of the curve of 96%, demonstrating high discriminating ability. The clinical diagnostic rule performed equally well regardless of shunt type. All TTE measures used in the clinical diagnostic rule had acceptable measures of interrater reliability.
| Variable | Total Cohort | Recoarctation of the Aorta | Univariate | Multivariate | |||
|---|---|---|---|---|---|---|---|
| Yes | No | OR (95% CI) | p Value | OR (95% CI) | p Value | ||
| Peak velocity >2.5 m/sec | 28 (26%) | 18 (95%) | 10 (11%) | 142 (17.1–1183) | <0.001 | 208 (17.2–2515) | <0.001 |
| Peak velocity (m/sec) | 1.82 (0.8–4.5) | 3.23 (1.8–4.5) | 1.61 (0.8–3.5) | 29.6 (6.8–129) | <0.001 | ||
| Mean gradient mm Hg | 4.9 (1.1–48.5) | 19.6 (3.8–48.5) | 4.14 (1.1–25.9) | 1.31 (1.1–1.4) | <0.001 | ||
| Coarctation index <0.7 | 38 (34%) | 16 (84%) | 22 (24%) | 17 (4.5–64) | <0.001 | 7.8 (1.7–35) | <0.01 |
| Coarctation index | 0.75 (0.3–1) | 0.53 (0.3–0.9) | 0.77 (0.44–0.94) | 0.91 (0.88–0.95) | <0.001 | ||
| Aorta <4 mm | 21 (19%) | 12 (63%) | 9 (10%) | 9.4 (5–51) | <0.001 | ||
| Acceleration at the aortic isthmus | 43 (40%) | 15 (88%) | 28 (39%) | 16.9 (3.6–78.8) | <0.001 | ||
| Decreased right ventricular systolic function | 21 (19%) | 9 (26%) | 12 (13%) | 6 (2–17.8) | <0.001 | 11.9 (1.6–112) | 0.03 |
| Worse atrioventricular valve regurgitation | 20 (18%) | 5 (26%) | 15 (16%) | 1.8 (0.5–5.8) | 0.31 | ||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


