It is unknown whether recurrence of atrial fibrillation (AF) is related to severity of left ventricular diastolic dysfunction (LVDD) before ablation in patients with preserved left ventricular ejection fraction (LVEF). We tested the hypothesis that the presence and/or severity of LVDD before catheter ablation are related to AF recurrence during the 12-month follow-up period in patients with normal LVEF. We also aimed to determine what echocardiographic and Doppler indexes of LVDD before ablation are associated with recurrence of AF after ablation. We identified 198 patients with normal LVEF who underwent catheter ablation for AF with evidence of normal sinus rhythm within 1 year before ablation. The recurrence rate during 12-month follow-up period was assessed. Of the 198 patients, 76 patients (38%) had symptomatic recurrence and 122 patients (62%) had no recurrence. None of the independent variables, including mitral valve Doppler E and A peak velocities, E/A ratio, tissue Doppler e′ and a′ peak velocities, left atrial volume index, isovolumic relaxation time, and deceleration time, predicted recurrence. Patients with average E/e′ ratio >13, however, had increased recurrence (67% vs 35%, odds ratio 3.70, 95% confidence interval 1.21 to 11.3, p <0.05). In conclusion, there was no difference in the severity of LVDD using conventional echocardiographic indexes of LVDD in patients with or without recurrence of AF ablation. However, patients with average E/e′ ratio >13 did have an increased recurrence rate of AF at 12 months after procedure. Therefore, E/e′ ratio, indicative of increased left atrial pressure, may serve as a marker for AF recurrence after ablation.
Previous studies have reported improvement in the grade of left ventricular diastolic dysfunction (LVDD) after ablation for atrial fibrillation (AF). However, it remains to be elucidated whether the presence and/or severity of LVDD in patients with preserved LV systolic function are associated with AF recurrence after ablation. Therefore, the aim of our study was to compare echocardiographic variables of diastolic function, specifically mitral valve early (E) and late (A) diastolic velocities, tissue Doppler early (e′) and late (a′) peak velocities, estimated pulmonary artery systolic pressure, mitral E velocity deceleration time, and isovolumic relaxation time between patients with and without recurrence of AF in the 12-month period after ablation. We also aimed to determine what echocardiographic and Doppler indexes of LVDD before ablation are associated with increased AF recurrence after ablation.
Methods
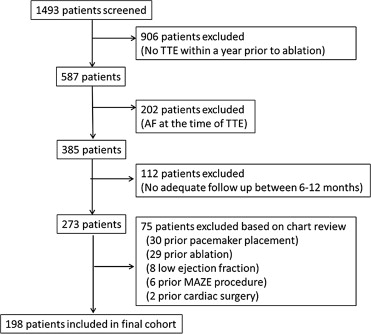
This was a retrospective case-control study of a total of 198 patients from the Loyola ablation registry (2002 to 2012). We screened a total of 1,493 patients. Inclusion criteria were as follows: (1) patients with transthoracic echocardiogram within 1 year before the procedure, (2) normal sinus rhythm during the transthoracic echocardiogram, (3) adequate follow-up after the procedure, and (4) normal LV ejection fraction (EF) at the time of the study. Patients with previous history of ablation, valvular disease, history of cardiac surgery, and history of pacemaker or implantable cardioverter-defibrillator placement were excluded ( Figure 1 ).
Choice of radiofrequency ablation or cryoballoon ablation was left to physician’s discretion. The techniques of pulmonary vein isolation using radiofrequency energy or cryoablation have been previously described. In brief, the patient was brought into the laboratory in a fasting state and placed under general anesthesia. Diagnostic coronary sinus catheter (14 pole; TZ Medical, Portland, Oregon), intracardiac ultrasound (SoundStar 3D; Biosense Webster Inc., Diamond Bar, California), Lasso (Biosense Webster Inc.), and ThermoCool ablation catheters (Biosense Webster Inc.) were placed using standard femoral and internal jugular access sites. Three-dimensional electroanatomic mapping of left atrium (LA) and pulmonary veins were obtained using intracardiac ultrasound and Carto System (Biosense-Webster Inc.). Ten thousand units of heparin were given following transseptal access, with a target activated clotting time of 300 to 350 seconds. After mapping of the LA, wide circumferential atrial ablation was performed around pulmonary veins in pairs using radiofrequency ablation with a maximal energy of 35 W over 30 to 60 seconds. Electrical isolation of pulmonary veins was confirmed after the procedure. Any additional focal triggers identified using high-dose isoproterenol were ablated in a similar fashion. Atrial flutter line ablation was performed if arrhythmias were inducible after the pulmonary vein isolation. Further outpatient medical management, including choice of antiarrhythmic drugs, was left to the discretion of the primary electrophysiologist. All antiarrhythmic drugs were discontinued at 3 months after the ablation if there was no evidence of recurrence.
AF was classified according to American College of Cardiology/American Heart Association/European Society of Cardiology guidelines. Paroxysmal AF was defined as recurrent AF (≧2 episodes) that terminates spontaneously within 7 days. Persistent AF was defined as AF that lasts beyond 7 days or lasts between 48 hours and 7 days but requires pharmacologic therapy or electrical cardioversion. Long persistent AF was defined as ongoing AF of >12-month duration. Any symptomatic or asymptomatic recurrence of AF or atrial flutter documented in medical record during follow-up was considered as recurrence. Follow-up visits were at 1, 3, 6, and 12 months with 7 days event monitoring at 6 months and 12 months. The first 6-month period after ablation was considered as blanking period.
All studies were performed using Phillips (Cleveland, Ohio) i33, Toshiba (Irvine, California) Artida, or General Electric (Stamford, Connecticut) Vivid 7 echocardiographic systems with a combined 5-MHz Doppler transducer. Two-dimensional echocardiographic images were obtained in parasternal long-axis, apical 2-chamber, and apical 4-chamber (A4C) views. Doppler gains were adjusted to provide a smooth velocity distribution without introducing noise at 100 mm/s swipe speed. All measures were acquired during sinus rhythm and were analyzed offline with customized software (ProSolv Fujifilm USA, Stamford, Connecticut).
LVEF was assessed using Simpson’s method. LA dimensions (area and longitudinal diameters) were measured at end-systole from A4C and apical 2-chamber views according to the American Society of Echocardiography guidelines. LA volume index was calculated from these measurements. LA volume index was categorized as normal (<28 ml/m 2 ) and mildly (29 to 33 ml/m 2 ), moderately (34 to 39 ml/m 2 ), and severely (>40 ml/m 2 ) enlarged.
Doppler analysis of mitral inflow and tissue Doppler imaging were recorded to assess LVDD. E and A peak velocities and deceleration time were measured from the A4C view. Pulsed tissue Doppler imaging measurements of mitral annulus motion were performed in the A4C view with a sample volume placed at the septal and lateral aspects of the mitral annulus. Peak gradient of the continuous flow Doppler across the tricuspid valve were measured from the A4C view to estimate the pulmonary artery pressure. Right atrial–right ventricular gradient was estimated by way of the modified Bernoulli equation, and the pulmonary artery systolic pressure was assessed by adding the right atrial pressure estimated using inferior vena cava indexes (<2.1 cm and >50% respiratory variation: 3 mm Hg; <2.1 cm and <50% respiratory variation: 8 mm Hg; and >2.1 cm: 15 mm Hg). Isovolumic relaxation time was measured at the Doppler imaging of the LV outflow tract.
Diastolic dysfunction (DD) grade was evaluated and categorized according to the American Society of Echocardiography guidelines by interrogating the mitral Doppler, tissue Doppler, and LA size. Septal and lateral e′/a′ ≧1 were normal and <1 was abnormal. Grade 0, normal diastolic function, was defined as septal e′ ≧8 cm/s, lateral e′ ≧10 cm/s, and LA volume index <34 ml/m 2 . If any of the 3 criteria were abnormal (septal e <8 cm/s, lateral e <10 cm/s, or LA volume index ≧34 ml/m 2 ), this was considered as evidence of DD. E/A ratio was used to further define the grades: E/A<0.8 was defined as grade 1 (mild dysfunction), 0.8 ≦ E/A < 1.5 was defined as grade 2 (moderate dysfunction), and E/A ≧2 was defined as grade 3 (severe dysfunction). If the E/A ratio was from 1.5 to 2.0, the grade was defined by deceleration time. Deceleration time ≧160 was categorized as grade 2, and deceleration time <160 was labeled grade 3. LA pressure was assessed by determining both septal E/e′ and lateral E/e′. Furthermore, we used average E/e′ >13 as an additional measure of increased LA pressure.
Continuous variables are reported as mean ± SD and were compared by Student t test. Categorical variables were compared by chi-square or Fisher’s exact test, as appropriate. p Value <0.05 was used as a cutoff for statistical significance. Analysis was performed using SPSS software, version 21 (SPSS, Chicago, Illinois).
Results
Baseline characteristics of the patient population are summarized in Table 1 . Of the 198 patients, 78 (38%) had recurrence and 122 (62%) did not have recurrence during the 12-month follow-up period. A total of 173 patients (87%) had paroxysmal AF, 23 (12%) had persistent, and only 2 (1%) had long persistent AF. Comparison between groups showed no significant difference between demographics, type of AF, clinical risk factor, or type of medication. However, there was a trend toward increased use of amiodarone before ablation (15% vs 4.2%, p = 0.10).
| Total (n = 198) | Recurrence | p-Value ∗ | ||
|---|---|---|---|---|
| Yes (n = 76) | No (n = 122) | |||
| Age at ablation (years) | 60 ± 10 | 59 ± 10 | 59 ± 10 | 0.82 |
| Men | 130 (66%) | 49 (64%) | 81 (66%) | 0.78 |
| White | 185 (93%) | 70 (92%) | 115 (94%) | 0.55 |
| Height (inch) | 70 ± 4 | 70 ± 4 | 69 ± 4 | 0.49 |
| Weight (lb) | 200 ± 40 | 199 ± 39 | 201 ± 40 | 0.73 |
| Body mass index (kg/m 2 ) | 28 ± 5 | 28 ± 5 | 29 ± 5 | 0.37 |
| Time between echo to ablation (days) | 75 ± 66 | 80 ± 69 | 72 ± 64 | 0.33 |
| Type of atrial fibrillation | 0.20 | |||
| Paroxysmal | 173 (87%) | 64 (84%) | 109 (89%) | |
| Persistent | 23 (12%) | 12 (16%) | 11 (9%) | |
| Long persistent | 2 (1.0%) | 0 (0%) | 2 (1.6%) | |
| Mitral regurgitation | 0.80 | |||
| None/trivial | 150 (76%) | 59 (78%) | 91 (75%) | |
| Mild | 46 (23%) | 16 (21%) | 30 (25%) | |
| Moderate | 2 (1.0%) | 1 (1.3%) | 1 (0.8%) | |
| Clinical risk factors | ||||
| Hypertension | 109/193 (57%) | 41/75 (39%) | 68/118 (61%) | 0.69 |
| Diabetes mellitus | 12/193 (6.2%) | 4/75 (5.3%) | 8/118 (6.8%) | 0.69 |
| Heart failure | 10/193 (5.2%) | 5/75 (6.7%) | 5/118 (4.2%) | 0.46 |
| Chronic obstructive lung disease | 7/193 (3.6%) | 4/75 (5.3%) | 3/118 (2.5%) | 0.31 |
| Chronic renal failure (Cre >1.5) | 2/183 (1.1%) | 0/69 (0%) | 2/114 (1.8%) | 0.27 |
| Prior CVA or TIA | 14/193 (7.3%) | 7/75 (9.3%) | 7/118 (5.9%) | 0.38 |
| Prior PCI | 9/193 (4.7%) | 6/75 (8.0%) | 3/118 (2.5%) | 0.08 |
| Prior coronary artery disease | 14/193 (7.3%) | 7/75 (9.3%) | 7/118 (5.9%) | 0.38 |
| Obstructive sleep apnea | 16 (8.1%) | 6 (7.9%) | 10 (8.2%) | 0.94 |
| Medication (current) | ||||
| Flecainide | 52/193 (27%) | 19/75 (25%) | 33/118 (28%) | 0.69 |
| Propafenone | 22/193 (11%) | 7/75 (9%) | 15/118 (13%) | 0.47 |
| Sotalol | 25/193 (13%) | 11/75 (15%) | 14/118 (12%) | 0.57 |
| Dofetilide | 5/193 (2.6%) | 2/75 (2.7%) | 3/118 (2.5%) | 0.95 |
| Dronedarone | 17/193 (8.8%) | 5/75 (6.7%) | 12/118 (10%) | 0.40 |
| Amiodarone | 16/193 (8.3%) | 11/75 (15%) | 5/118 (4.2%) | 0.10 |
| Beta-blocker | 107/193 (54%) | 41/75 (58%) | 66/118 (56%) | 0.86 |
| Calcium channel blocker | 57/193 (30%) | 22/75 (29%) | 35/118 (30%) | 0.96 |
| Statin | 77/193 (40%) | 29/75 (39%) | 48/118 (40%) | 0.78 |
| Warfarin | 94/193 (49%) | 32/75 (43%) | 62/118 (53%) | 0.18 |
∗ p Value is comparison between recurrence and nonrecurrence groups.
Mean values of echocardiographic variables across the 2 groups are demonstrated in Table 2 . There was no significant difference in LVEF, 2-dimensional measurements, LA volume index, estimated pulmonary artery systolic pressure, isovolumic relaxation time, or deceleration time. We then evaluated the echocardiographic values as categorical values ( Table 3 ). There was no significant difference in severity of LA volume index or grade of DD between the 2 groups. Similarly, there was no significant difference in frequencies of abnormal septal e′/a′ ratio (55% vs 50%, p = 0.55), and lateral e′/a′ ratio (37% vs 28%, p = 0.23) across recurrence group and no-recurrence group, respectively. Elevated LA pressure (average E/e′ >13) was observed more often in patients with recurrence (14% vs 4%, p <0.05). Furthermore, the rate of AF recurrence after ablation was greater in patients with elevated LA pressure (67% vs 35%, odds ratio 3.70, 95% confidence interval 1.21 to 11.3, p <0.05). Using more stringent criteria inclusive of both septal E/e′ ≧15 and lateral ≧12, the results were still significant (64% vs 35%, odds ratio 3.28, 95% confidence interval 1.05 to 10.2, p <0.05). Therefore, this finding confirms that there is an association between elevated LA pressure and AF recurrence after ablation.



