The CHA 2 DS 2 -VASc and CHADS 2 risk stratification schemes are used to predict thromboembolism and ischemic stroke in patients with atrial fibrillation. However, limited data are available regarding the utility of these risk stratification schemes for stroke in patients with atrial flutter. A retrospective analysis of 455 transesophageal echocardiographic studies in patients with atrial flutter was performed to identify left atrial (LA) thrombi and/or spontaneous echocardiographic contrast (SEC). The CHA 2 DS 2 -VASc (Congestive heart failure, Hypertension, Age ≥75 years [doubled risk weight], Diabetes mellitus, previous Stroke/transient ischemic attack [doubled risk weight], Vascular disease, Age 65 to 74 years, Sex) and CHADS 2 (Congestive heart failure, Hypertension, Age ≥75 years, Diabetes mellitus, previous Stroke/transient ischemic attack [double risk weight]) scores were calculated to stratify the risk of stroke or transient cerebrovascular ischemic events. Transesophageal echocardiography revealed LA thrombi in 5.3% and SEC in 25.9% of patients. Using CHADS 2 , LA thrombus was found in 2.2% of the low–intermediate-risk group and 8.3% of the high-risk group (p = 0.005). SEC was found in 19.8% of the low–intermediate-risk group and 32% of the high-risk group (p = 0.004). Using CHA 2 DS 2 -VASc, LA thrombus was found in 1.7% of the low–intermediate-risk group and 6.5% of the high-risk group (p = 0.053). SEC was found in 11.8% of the low–intermediate-risk group versus 30.9% of the high-risk group (p = 0.004). The sensitivity for LA thrombus/SEC with a high CHADS 2 and CHA 2 DS 2 -VASc score was 64.8% and 88.7%, respectively (p = 0.0001). The specificity for LA thrombus/SEC with high CHADS 2 and CHA 2 DS 2 -VASc scores was 52.6% and 28.9%, respectively (p = 0.0001). In conclusion, both CHA 2 DS 2 -VASc and CHADS 2 scores are useful for stroke risk stratification in patients with atrial flutter. CHA 2 DS 2 -VASc had greater sensitivity for LA thrombus and SEC detection at the cost of reduced specificity.
Because of the morbidity associated with atrial fibrillation (AF) and atrial flutter (AFL), The American College of Cardiology/American Heart Association/European Society of Cardiology/Heart Rhythm Society guidelines recommend antithrombotic therapy (either aspirin or warfarin/dabigatran) for all patients with AF and AFL according to the clinical risk factors for thromboembolism. The CHADS 2 (Congestive heart failure, Hypertension, Age ≥75 years, Diabetes mellitus, previous Stroke/transient ischemic attack [double risk weight]) score is the most commonly used method to assess clinical risk factors and identify which patients would benefit most from therapeutic anticoagulation with warfarin/dabigatran. Recent studies have recommended inclusion of newly recognized risk factors, including female gender, age 65 to 74 years, and coronary artery disease to more accurately assess the thromboembolic risk. These factors have been incorporated into the CHA 2 DS 2 -VASc (Congestive heart failure, Hypertension, Age ≥75 years [doubled risk weight], Diabetes mellitus, previous Stroke/transient ischemic attack [doubled risk weight], Vascular disease, Age 65 to 74 years, Sex) risk score. The CHA 2 DS 2 -VASc score has been validated for thromboembolic risk stratification in patients with AF and might be especially helpful in identifying truly low-risk patients with AF. In contrast, the clinical utility of either the CHADS 2 or CHA 2 DS 2 -VASc score in patients with AFL has not been well studied. The objective of the present study was to evaluate and compare the ability of the CHADS 2 and CHA 2 DS 2 -VASc scores to predict the detection of left atrial (LA) thrombus in patients with AFL.
Methods
Heart failure was defined as left ventricular systolic dysfunction (left ventricular ejection fraction ≤40% ) and clinical symptoms. Vascular disease was defined as any clinical history of myocardial infarction or angiographically proven significant coronary artery/peripheral artery disease. Other risk factors, including hypertension, diabetes mellitus, stroke/transient ischemic attack, age, and gender, were defined using standard clinical criteria.
All patients with AFL who underwent preprocedural transesophageal echocardiography at Rush University Medical Center for evaluation of LA thrombi before radiofrequency catheter ablation or direct current cardioversion from September 2002 and February 2011 were identified. The study population included 455 transesophageal echocardiograms (in 373 patients with AFL). The patients’ mean age was 61.3 ± 13.2 years, and 31.2% were women ( Table 1 ). For each patient, the preprocedural transesophageal echocardiogram was reviewed. Thrombus was defined as a circumscribed, uniformly echodense mass distinct from the underlying LA endocardium and pectinate muscles. Spontaneous echocardiographic contrast (SEC) was defined as dynamic “smoke-like” echoes with characteristic swirling motion that could not be eliminated despite optimized gain settings. The presence of thrombus was considered an absolute contraindication for direct current cardioversion or radiofrequency catheter ablation but the presence of SEC (regardless of severity) was not.
| Clinical Variable | Value |
|---|---|
| Mean age ± SD (years) | 61 ± 13 |
| Age group (n) | |
| <65 | 276 (60.7%) |
| 65–74 | 106 (23.3%) |
| ≥75 | 73 (16.0%) |
| Men (n) | 313 (68.8%) |
| Left ventricular ejection fraction ≤40% (n) | 154 (33.8%) |
| Hypertension (n) | 299 (65.7%) |
| Diabetes mellitus (n) | 118 (25.9%) |
| Stroke/transient ischemic attack (n) | 42 (9.2%) |
| Coronary artery or peripheral vascular disease (n) | 166 (36.5%) |
| Concomitant atrial fibrillation (n) | 201 (44.2%) |
The calculation of the CHADS 2 and CHA 2 DS 2 -VASc scores was performed by retrospective clinical chart analysis of the risk factors present at transesophageal echocardiography. To compare the predictive ability of the CHADS 2 and CHA 2 DS 2 -VASc scores, we separated patients into a “low–intermediate-risk” group (CHADS 2 and CHA 2 DS 2 -VASc score 0 to 1) and a “high-risk” group (CHADS 2 and CHA 2 DS 2 -VASc score ≥2). Any documented history of AF or therapy with anticoagulant agents (e.g., low-molecular-weight heparin subcutaneous injection, heparin infusion, warfarin, or dabigatran) at transesophageal echocardiography was also noted. For calculation of the CHADS 2 sensitivity and specificity, we defined true-positive results as the presence of LA thrombus/SEC and a high CHADS 2 score. True-negative results were defined as no LA thrombus/SEC and a low–intermediate CHADS 2 score. False-negative results were defined as the presence of LA thrombus/SEC and a low–intermediate CHADS 2 score. False-positive results were defined as no LA thrombus/SEC and a high CHADS 2 score. For calculation of the CHA 2 DS 2 -VASc sensitivity and specificity, we defined true-positive results as the presence of LA thrombus/SEC and a high CHA 2 DS 2 -VASc score. True-negative results were defined as no LA thrombus/SEC and a low–intermediate CHA 2 DS 2 -VASc score. False-negative results were defined as the presence of LA thrombus/SEC and a low–intermediate CHA 2 DS 2 -VASc score. False-positive results were defined as no LA thrombus/SEC and a high CHA 2 DS 2 -VASc score. The institutional review board of Rush University Medical Center approved the present study.
Fisher’s exact test and Student’s unpaired t test were used to calculate statistical significance. The sensitivity and specificity were calculated using standard epidemiologic formulas. Threshold of significance for all statistical tests was set at p <0.05. All tests performed were 2-sided.
Results
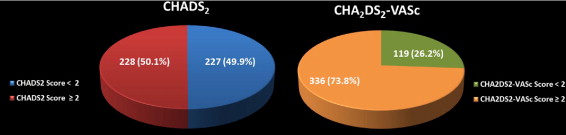
The risk stratification and distribution of risk factor prevalence within the CHADS 2 and CHA 2 DS 2 -VASc risk schemes are presented in Figure 1 . Overall, transesophageal echocardiography revealed LA thrombi in 24 (5.3%) and SEC in 118 (25.9%) of the 455 patient studies reviewed. For CHADS 2 , LA thrombus was found in 5 (2.2%) of 227 in the low–intermediate-risk group and 19 (8.3%) of 228 in the high-risk group (p = 0.005). SEC was found in 45 (19.8%) of 227 in the low–intermediate-risk group and 73 (32%) of 228 in the high-risk group (p = 0.004). For CHA 2 DS 2 -VASc, LA thrombus was identified in 2 (1.7%) of 119 in the low–intermediate-risk group and 22 (6.5%) of 336 in the high-risk group (p = 0.053). SEC was found in 14 (11.8%) of 119 in the low–intermediate-risk group and 104 (31%) of 336 in the high-risk group (p = 0.004). The stratification of LA thrombus and SEC patient-cases by CHADS 2 and CHA 2 DS 2 -VASc scores is listed in Table 2 .
| Score/Risk Category | TEEs (n = 455) | LA Thrombus (n = 24) | SEC (n = 118) |
|---|---|---|---|
| CHADS 2 score | |||
| 0 | 83 | 2 (2.4%) | 8 (9.6%) |
| 1 | 144 | 3 (2.1%) | 37 (25.7%) |
| 2 | 126 | 9 (7.1%) | 36 (28.6%) |
| 3 | 72 | 7 (9.7%) | 26 (36.1%) |
| 4 | 25 | 2 (8%) | 9 (36%) |
| 5 | 5 | 1 (20%) | 2 (40%) |
| 6 | 0 | 0 | 0 |
| CHA 2 DS 2 -VASc score | |||
| 0 | 30 | 2 (6.7%) | 3 (10%) |
| 1 | 89 | 0 (0%) | 11 (12.4%) |
| 2 | 97 | 3 (3.1%) | 24 (24.7%) |
| 3 | 99 | 12 (12.1%) | 39 (39.4%) |
| 4 | 84 | 2 (2.4%) | 20 (23.8%) |
| 5 | 38 | 3 (7.9%) | 15 (39.5%) |
| 6 | 16 | 2 (12.5%) | 6 (37.5%) |
| 7 | 2 | 0 (0%) | 0 (0%) |
| 8 | 0 | 0 | 0 |
| 9 | 0 | 0 | 0 |
The sensitivity of CHADS 2 and CHA 2 DS 2 -VASc for the presence of LA thrombus was 79.2% and 91.7%, respectively (p = 0.42). The specificity for the presence of LA thrombus was 51.5% for CHADS 2 and 27.1% for CHA 2 DS 2 -VASc (p = 0.0001). The sensitivity for the presence of SEC was 61.9% for CHADS 2 and 88.1% for CHA 2 DS 2 -VASc (p = 0.0001). The specificity for the presence of SEC was 54% for CHADS 2 and 31.2% for CHA 2 DS 2 -VASc (p = 0.0001).
The sensitivity for the combined end point of LA thrombus or SEC was 64.8% for CHADS 2 and 88.7% for CHA 2 DS 2 -VASc (p = 0.0001). The specificity for the combined end point of LA thrombus or SEC was 52.6% for CHADS 2 and 28.9% for CHA 2 DS 2 -VASc (p = 0.0001).
Comparing the transesophageal echocardiographic studies with and without LA thrombus, we noted the following in the transesophageal echocardiograms demonstrating thrombus ( Table 3 ): a greater mean CHADS 2 score, a greater proportion of patients with a CHADS 2 score ≥2, and a greater prevalence of SEC. Trends were seen toward a greater mean CHA 2 DS 2 -VASc score and a greater proportion of patients with a CHA 2 DS 2 -VASc score ≥2. No gender-based differences were detected between the 2 groups. Additional analysis of the specific risk factors revealed a greater likelihood of congestive heart failure and a history of stroke/transient ischemic attack in patients with LA thrombus. Anticoagulation data at transesophageal echocardiography was available for 90.3% of the patients. No difference was found between the use of anticoagulants in patients with or without thrombus (62.5% in the LA thrombus group vs 58.9% in the no thrombus group; p = 0.83). AF episodes were identified in 44.2% of patients. No differences were found in the likelihood of previous AF in the 2 groups (50% vs 43.9%; p = 0.67) or the likelihood of AFL as the immediate preprocedural rhythm at transesophageal echocardiography (90.9% vs 65.8%; p = 0.11). The immediate preprocedural rhythm was documented in 385 (84.6%) of 455 of our patients. AFL was present in 256 (66.5%), AF in 40 (10.4%), and sinus rhythm in 89 (23.1%) of these 385 patients. No postprocedural stroke or thromboembolic events were noted acutely in our study population.
| Variable | LA Thrombus (n = 24) | No LA Thrombus (n = 431) | p Value |
|---|---|---|---|
| CHADS 2 score | 2.29 ± 1.17 | 1.58 ± 1.16 | 0.004 ⁎ |
| CHADS 2 ≥2 | 79.2% (19/24) | 48.5% (209/431) | 0.005 ⁎ |
| CHA 2 DS 2 -VASc score | 3.21 ± 1.47 | 2.64 ± 1.55 | 0.08 |
| CHA 2 DS 2 -VASc ≥2 score | 91.7% (22/24) | 72.9% (314/431) | 0.053 |
| Prevalence of spontaneous echocardiographic contrast | 75% (18/24) | 23.2% (100/431) | 0.0001 ⁎ |
| Men | 79.2% (19/24) | 68.2% (294/431) | 0.37 |
| Age (years) | 61 ± 10.8 | 61.3 ± 13.3 | 0.9 |
| Congestive heart failure (left ventricular ejection fraction ≤40%) | 58.3% (14/24) | 32.5% (140/431) | 0.01 ⁎ |
| Hypertension | 75% (18/24) | 65.2% (281/431) | 0.38 |
| Diabetes mellitus | 25% (6/24) | 26% (112/431) | 1.00 |
| Stroke/transient ischemic attack | 25% (6/24) | 8.4% (36/431) | 0.02 ⁎ |
| Vascular disease (coronary artery disease or peripheral vascular disease) | 37.5% (9/24) | 36.4% (157/431) | 1.00 |
| Documented history of previous atrial fibrillation | 50% (12/24) | 43.9% (189/431) | 0.67 |
| Anticoagulation | 62.5% (15/24) | 58.9% (254/431) | 0.83 |
A subanalysis of “pure” AFL (patients with AFL only without any documented history of AF) revealed LA thrombi in 12 (4.7%) and SEC in 57 (22.4%) of the 254 patient cases reviewed. Comparing the pure AFL group to the study group as a whole, no overall difference was noted in the prevalence of LA thrombus (4.7% vs 5.3%; p = 0.86) or the prevalence of SEC (22.4% vs 25.9%; p = 0.32). Moreover, when comparing the pure AFL group and the AFL plus documented history of AF group, no overall difference was noted in prevalence of LA thrombus (4.7% vs 6.5%; p = 0.67) or prevalence of SEC (22.4% vs 30.3%; p = 0.13).
For CHADS 2 , LA thrombus was found in 1 (0.8%) of 118 in the low–intermediate-risk group and 11 (8.1%) of 136 in the high-risk group (p = 0.007). SEC was found in 16 (13.6%) of 118 in the low–intermediate-risk group and 41 (30.1%) of 136 in the high-risk group (p = 0.002). For CHA 2 DS 2 -VASc, LA thrombus was identified in 0 (0%) of 63 in the low–intermediate-risk group and 12 (6.3%) of 191 in the high-risk group (p = 0.04). SEC was found in 4 (6.3%) of 63 in the low–intermediate-risk group and 53 (27.7%) of 191 in the high-risk group (p = 0.0002).
The sensitivity for the presence of LA thrombus was 91.7% for CHADS 2 versus 100% for CHA 2 DS 2 -VASc (p = 1.0). The specificity for the presence of LA thrombus was 48.3% for CHADS 2 versus 26% for CHA 2 DS 2 -VASc (p = 0.0001). The sensitivity for the presence of SEC was 71.9% for the CHADS 2 score versus 93% for the CHA 2 DS 2 -VASc score (p = 0.006). The specificity for the presence of SEC was 51.8% for CHADS 2 versus 29.9% for CHA 2 DS 2 -VASc (p = 0.0001). The sensitivity for the combined end point of LA thrombus or SEC was 75.4% for CHADS 2 versus 94.2% for CHA 2 DS 2 -VASc (p = 0.004). The specificity for the combined end point of LA thrombus or SEC was 49.9% for CHADS 2 versus 27.8% for CHA 2 DS 2 -VASc (p = 0.0001).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


