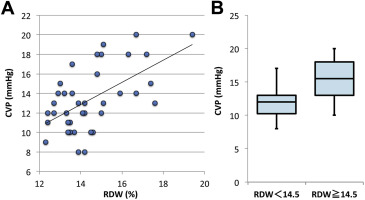
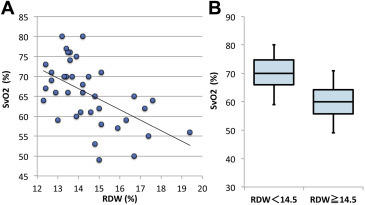
The red blood cell distribution width (RDW) is a quantitative measure of the variability in the size of circulating erythrocytes. We aimed to study whether higher levels of the RDW were associated with heart failure in a Fontan circulation and to analyze its clinical value compared to brain natriuretic peptide. This retrospective study included 38 consecutive pediatric patients with a Fontan circulation who underwent routine cardiac catheterization at the International Medical Center, Saitama Medical University from October 2010 to July 2014. We assessed the relation between the RDW and catheterization data such as the central venous pressure (CVP), mixed venous oxygen saturation (SvO 2 ), and cardiac index (CI). The RDW was positively correlated with the CVP (p = 0.0002). The elevated RDW group had a significantly greater CVP than the normal RDW group (p = 0.0003). Also, the RDW was negatively correlated with the SvO 2 (p = 0.0004). The elevated RDW group had a significantly less SvO 2 than the normal RDW group (p <0.0001). The CI in the elevated RDW group was lower than that in the normal RDW group (p = 0.0421). In the multivariate regression analysis, the RDW was a significant independent predictor of the CVP and SvO 2 . The BNP level did not have any significant relation with the CVP, SvO 2, or CI. The RDW is a convenient and powerful marker for detecting heart failure in a Fontan circulation.
The red blood cell distribution width (RDW) is a quantitative measure of the variability in the size of circulating erythrocytes, and this parameter is routinely reported as part of the complete blood count. An elevated RDW suggests a nutritional deficiency (such as a lack of vitamin B12 or folic acid) or a recent blood transfusion. Recent reports have reported a strong independent association between the RDW and heart failure, coronary disease, myocardial infarctions, and pulmonary hypertension. However, there is no information regarding the efficacy of the RDW in congenital heart diseases. At present, the brain natriuretic peptide (BNP) is regarded as a prognostic marker in patients with pediatric heart failure. However, in patients with a Fontan circulation, it is noted they have lower than expected BNP levels relative to their ventricular function and functional status because of their reduced preload and limited preload reserve.
Methods
This study was approved by the Institutional Review Board of Saitama Medical University (No 14-199, International Medical Center, Saitama Medical University). This retrospective study included 38 consecutive pediatric patients with a Fontan circulation who underwent a postoperative routine cardiac catheterization at the International Medical Center, Saitama Medical University from October 2010 to July 2014. These patients were divided into 2 groups according to their RDW levels as follows: RDW <14.5%, n = 22 (normal RDW group) and RDW ≥14.5%, n = 16 (elevated RDW group). We reviewed the demographic parameters including the age, gender, underlying disease, blood pressure, and medication use from their medical records. Also, we reviewed the hemodynamic data, chest x-rays, and echocardiographic data from the summary on those days.
Blood tests were performed in all patients at the time of admission. The complete blood cell count and biochemical laboratory parameters were measured by an XE-2100 (Sysmex Inc., Kobe, Japan) and TBA-c16000 (Toshiba medical systems Inc., Tochigi, Japan), respectively. The BNP level was measured by an AIA-360 (Tosoh Inc., Tokyo, Japan). The normal range of the RDW and BNP levels was 11.9% to 14.5 % and 0 to 18.4 pg/mL, respectively. As a noninvasive index, we assessed the ejection fraction and fractional shortening by reviewing the echocardiography at the time of admission.
All continuous data are expressed as the mean ± standard deviation. Categorical data were performed with a Pearson chi-square test or Fisher’s exact test. Comparisons between the 2 groups were performed using a Mann–Whitney U test. A Pearson correlation analysis was used to assess the relation between the RDW and catheterization parameters. An analysis of covariance and multivariate regression were also performed to determine the independent effect of the RDW. A p <0.05 was considered statistically significant. All statistical analyses were performed using JMP version 11.2.0 (SAS, Cary, North Carolina) and GraphPad PRISM version 5.01 (GraphPad Software, Inc., La Jolla, California) software in the department of Pediatric Cardiology, Saitama International Medical Center.
Results
Table 1 summarizes the basic characteristics. The age, gender, and systolic and diastolic blood pressures did not differ between the 2 groups. A greater RDW was associated with lower hemoglobin and mean corpuscular volume levels and higher C-reactive protein levels. Also, the elevated RDW group tended to have a right ventricle morphology consisting of a systemic ventricle and tended to have a lower ejection fraction and fractional shortening. In contrast, the BNP, serum creatinine and serum albumin levels, liver function, coagulation, and cardiothoracic ratios did not statistically differ between the 2 groups. There seemed to be a trend toward a greater drug usage in the elevated RDW group patients, but it was not statistically significant. During the study period, there was 1 death in the high RDW group because of sepsis.
| Variable | RDW<14.5 % (n=22) | RDW≧14.5 % (n=16) | p value |
|---|---|---|---|
| Demographic characteristics | |||
| Age (month) | 43.0 ± 3.7 | 55.1 ± 14.7 | 0.4945 |
| Male sex | 68% | 50% | 0.3235 |
| Systolic blood pressure (mm Hg) | 93.3 ± 3.7 | 94.8 ± 4.6 | 0.8074 |
| Diastolic blood pressure (mm Hg) | 57.6 ± 2.5 | 51.1 ± 3.1 | 0.1099 |
| Diagnosis (n) | |||
| Double outlet right ventricle | 1 | 3 | |
| Hypoplastic left heart syndrome | 1 | 4 | |
| Single ventricle | 9 | 8 | |
| Pulmonary atresia with intact ventricular septum | 6 | 1 | |
| Ebsteins’ anomaly | 2 | 0 | |
| Tricuspid valve atresia | 2 | 0 | |
| Transposition of the great arteries | 1 | 0 | |
| Morphology of systemic right ventricle (n) | 12 | 14 | 0.0403 |
| Laboratory parameters and imaging | |||
| Hemoglobin (g/dL) | 15.2 ± 0.5 | 13.7 ± 0.4 | 0.0366 |
| Mean Corpuscular Volume (fl) | 81.9 ± 1.3 | 77.4 ± 1.8 | 0.0398 |
| Aspartate aminotransferase (U/L) | 37.1 ± 2.0 | 39.4 ± 1.7 | 0.4141 |
| Alanine aminotransferase (U/L) | 22.1 ± 2.1 | 20.1 ± 1.5 | 0.4715 |
| C-reactive protein (mg/dL) | 0.09 ± 0.02 | 0.49 ± 0.22 | 0.0424 |
| BNP (pg/mL) | 24.6 ± 7.8 | 33.6 ± 6.8 | 0.4072 |
| Serum creatinine (mg/dL) | 0.35 ± 0.03 | 0.35 ± 0.02 | 0.9266 |
| Serum albumin (g/dL) | 4.7 ± 0.1 | 4.5 ± 0.1 | 0.1459 |
| Activated partial thromboplastin time (sec) | 42.4 ± 1.4 | 42.8 ± 2.0 | 0.8463 |
| Prothrombin time-international normalized ratio | 1.4 ± 0.1 | 1.6 ± 0.1 | 0.2573 |
| Cardiothoracic ratio (%) | 49.3 ± 1.2 | 51.1 ± 1.0 | 0.3214 |
| Ejection Fraction (%) | 60.8 ± 3.2 | 66.5 ± 2.4 | 0.1582 |
| Fractional Shortening (%) | 30.4 ± 2.5 | 37.6 ± 1.5 | 0.0145 |
| Medication use | |||
| Diuretics (%) | 59 | 75 | 0.4898 |
| β- adrenergic blocker (%) | 5 | 25 | 0.1409 |
| Angiotensin-converting enzyme inhibitor (%) | 27 | 25 | 0.8752 |
| Deceased (n) | 0 | 1 | 0.4211 |
The RDW was positively correlated with the CVP ( r 2 = 0.7747; p = 0.0002, Figure 1 ). The CVP in the elevated RDW group was significantly greater compared to that in the normal RDW group (15.5 ± 0.8 vs 11.9 ± 0.5, p = 0.0003, Figure 1 ). Also, the RDW was negatively correlated with the SvO 2 ( r 2 = 0.7102; p = 0.0004, Figure 2 ). The SvO 2 in the elevated RDW group was significantly lower than that in the normal RDW group (59.8 ± 1.6 vs 69.9 ± 1.3, p <0.0001, Figure 2 ). The CI in the elevated RDW group tended to be lower than that in the normal RDW group (3.3 ± 0.1 vs 3.8 ± 0.2, p = 0.0421).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


