The objective of this study was to evaluate the prognostic value of the myocardial performance index (MPI), assessed by color-coded tissue Doppler imaging (TDI) M-mode through the anterior mitral leaflet. Color TDI M-mode through the mitral leaflet is an easy, very fast, and precise method to estimate cardiac intervals and thus obtain the MPI, but the diagnostic and prognostic values of this parameter are unknown. In a large population study, cardiac function was evaluated in 1,100 participants by conventional echocardiography and TDI. MPI was calculated from pulse-wave Doppler analyses of left ventricular in- and outflow using standard procedures (MPI conv ) and by color-coded TDI M-mode through the mitral leaflet in the apical 4-chamber view (MPI TDI ). MPI TDI was increased in subjects with coronary heart disease (CHD) compared to controls, even after multivariable adjustment (p <0.002). During follow-up (median 5.3 years), 90 participants died. MPI TDI was significantly associated with overall mortality, and risk of dying increased by 31% per 0.1 increase in MPI TDI . In contrast to MPI conv , MPI TDI provided independent prognostic information in a multivariable Cox proportional hazard model (adjusting for age, gender, body mass index, heart rate, mean arterial blood pressure, and CHD), with a hazard ratio of 1.18 (p = 0.01) per 0.1 increase in MPI TDI . In conclusion, MPI TDI is a quick, simple, and reproducible measurement, which is increased in subjects with CHD and provides independent prognostic information in a low-risk population.
Cardiac intervals have been suggested and investigated as potential markers of cardiac dysfunction for a long time. Preservation of normal cardiac intervals is intimately related to normal cardiac physiology, hemodynamics, and mechanics. In the ailing myocardium cardiac intervals may change early in the disease process, thus providing early signs of subclinical disease. The myocardial performance index (MPI), also known as the Tei index, is an attempt to expand the use of such intervals to characterize systolic and diastolic performances by 1 single value derived from calculations of pulse-Doppler echocardiography of the left ventricular (LV) outflow tract and mitral valve inflow. MPI has been shown to correlate significantly with established indexes of LV systolic and diastolic functions by cardiac catheterization. Besides being a feasible noninvasive indicator of overall LV function, MPI has been shown to provide prognostic value in the general population and in patients with various cardiac conditions. As an alternative noninvasive approach to obtain MPI, tissue Doppler imaging (TDI) of the mitral annular myocardial segments (MPI regional ) have been demonstrated to correlate well with conventional MPI obtained by the pulse-Doppler method (MPI conv ), although the absolute value obtained by the 2 methods are different. TDI allows the intervals to be obtained in the same cardiac cycle in contrast to the conventional method, which probably makes MPI as assessed by TDI less susceptible to variation in heart rate. MPI regional is, however, limited by regional myocardial differences in intervals. This could be overcome by analyzing global intervals through evaluation of mitral valve motion by a simple M-mode analysis instead of focusing on regional myocardial movement. Thus, using color TDI M-mode through the mitral valve to estimate MPI (MPI TDI ) may be a better method reflecting global cardiac time intervals and eliminating beat-to-beat variation.
Methods
This study was performed as a substudy of the Fourth Copenhagen City Heart Study, a longitudinal cohort study of cardiovascular disease and risk factors. The present report includes 1,100 randomly selected men and women (20 to 93 years old) who underwent an echocardiographic examination including color TDI. Whether or not a participant underwent echocardiography was completely independent of his or her health status and other risk factors. Patients with atrial fibrillation, significant valvular stenosis, or regurgitation were excluded. All subjects gave written informed consent to participate, and the study was performed in accordance with the second Declaration of Helsinki and approved by the regional ethics committee.
Coronary heart disease (CHD) was defined as a history of hospital admission due to acute coronary artery occlusion, percutaneous coronary intervention, or coronary artery bypass grafting or major ischemic alterations on electrocardiogram as defined by Minnesota Codes 1.1 to 3. Participants without CHD were defined as controls.
Three experienced echocardiographic technicians using a Vingmed Ultrasound Vivid Five (GE Medical, Horten, Norway) with a 2.5-MHz probe recorded all echocardiograms for the Copenhagen City Heart Study. All subjects were examined in the left lateral decubitus position. All images were recorded using second harmonic imaging at the time of end-expiration. Collected data were stored on magneto-optical disks and an external hard drive (FireWire, LaCie, France) and analyzed off-line with commercially available software (EchoPac, GE Medical), with the investigator being blinded to other information.
Pulse-wave Doppler at the apical position was used to record mitral inflow between the tips of the mitral leaflets and LV outflow just below the aortic annulus. One observer performed conventional echocardiographic analyses. The interval from mitral valve closing to opening was determined as the period from the end to onset of mitral inflow. LV ejection time (ET) was determined as the period from onset to end of LV outflow. MPI conv was calculated as (interval from mitral valve closing to opening minus ejection time)/ejection time.
Intervals by the TDI method were measured in the apical 4-chamber view at the highest possible frame rate (median 133 frames/s, interquartile range 37) using a 2 to 4-cm straight M-mode line placed through the septal half of the mitral leaflet, perpendicular to the leaflet in end-systole in closed position ( Figure 1 ).
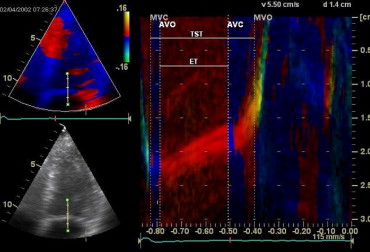
One observer performed TDI analyses. From the color M-mode diagram intervals were measured. TDI interval from mitral valve closing to opening was defined as the period from color shift from blue to red at end-diastole to the rapid opening of the mitral valve indicated by the color shift of red-orange to yellow at the beginning of diastole ( Figure 1 ). TDI ejection time was defined as the period from the color shift of blue to red color in systole ending at the color shift from red to blue at end-systole ( Figure 1 ). MPI TDI was calculated from measured cardiac intervals as (TDI interval from mitral valve closing to opening minus TDI ejection time)/TDI ejection time.
Participants were followed from the examination in 2002 through 2003 until August 2007 or time of death using the unique personal identification number in the Central Office of Civilian Registration. Follow-up was 100% complete.
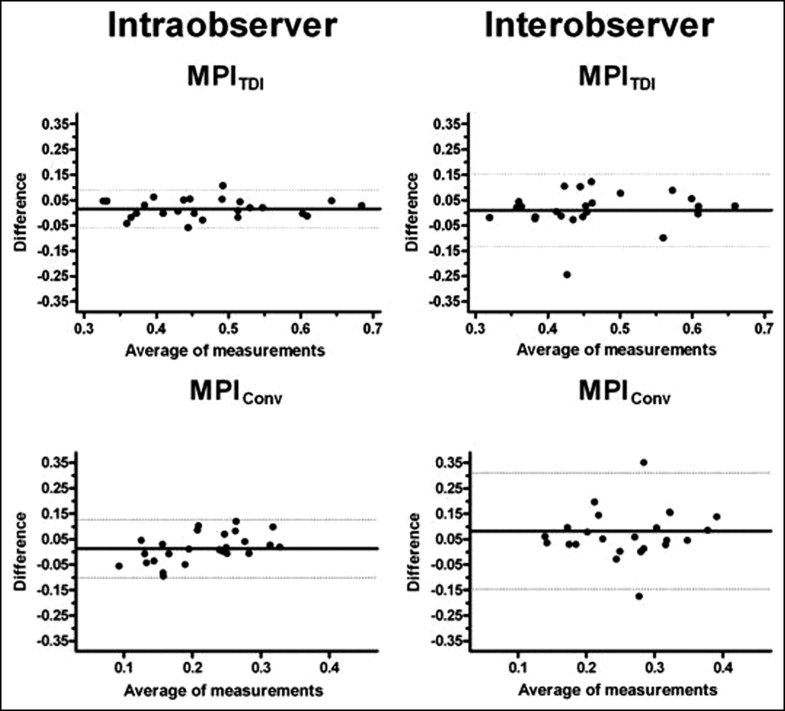
Table 1 presents comparisons between groups performed by Student’s t test or Fisher’s exact test. Values in parentheses are 95% confidence intervals unless otherwise stated. Intra- and interobserver variabilities were determined by Bland-Altman plots of repeated analyses of stored echocardiographic loops (n = 25). Association with MPI conv and MPI TDI was tested for the defined groups by univariable and multivariable regression analyses including the prespecified baseline variables age, gender, body mass index, heart rate, and mean arterial blood pressure.
| Variable | Controls | CHD | p Value |
|---|---|---|---|
| (n = 943) | (n = 93) | ||
| Age (years) | 59 ± 16 | 69 ± 12 | <0.001 |
| Men | 42% | 37% | 0.32 |
| Body mass index (kg/m 2 ) | 25.5 ± 3.9 | 26.7 ± 4.4 | <0.01 |
| Heart rate (beats/min) | 69 ± 11 | 69 ± 11 | 0.76 |
| Systolic blood pressure (mm Hg) | 136 ± 23 | 145 ± 26 | <0.001 |
| Diastolic blood pressure (mm Hg) | 78 ± 12 | 79 ± 15 | 0.47 |
| Mean arterial blood pressure (mm Hg) | 97 ± 14 | 101 ± 16 | <0.01 |
| Conventional myocardial performance index | 0.39 ± 0.14 | 0.45 ± 0.20 | <0.001 |
| Tissue Doppler imaging myocardial performance index | 0.51 ± 0.12 | 0.59 ± 0.22 | <0.001 |
| Dead at follow-up | 7.5% | 20.4% | <0.001 |
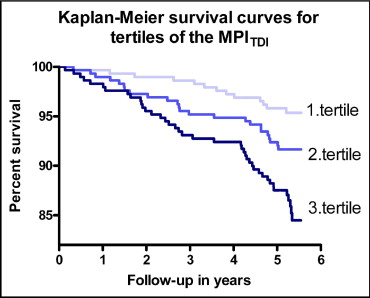
Tertiles of MPI TDI were constructed and cumulative survival curves were established by the Kaplan-Meier method. Univariable and multivariable Cox proportional hazards regression models were used to examine the association of each of the 2 methods used to obtain MPI and baseline variables to risk of death. Mis-specification of the functional form of covariates and the assumption of proportional hazards were evaluated by plots of cumulative martingale residuals.
A p value <5% in 2-sided tests was considered statistically significant. All analyses were performed with SAS 9.1.3 for Windows (SAS Institute, Cary, North Carolina).
Results
In total 1,100 subjects were examined with TDI and conventional echocardiography in this study. Forty-five were excluded due to inadequate quality of echocardiographic examination, and 19 were excluded due to atrial fibrillation or significant valvulopathy. Characteristics of the remaining subjects constituting the study population (n = 1,036) are listed in Table 1 . The study population was divided into groups with and without CHD at time of enrollment.
MPI conv remained significantly higher in the CHD group after multivariable adjustment for age, gender, body mass index, heart rate, and mean arterial blood pressure (0.44, 0.41 to 0.48, vs 0.39, 0.38 to 0.40, p <0.002). This pattern was the same for MPI TDI , which remained significantly higher in the CHD group after multivariable adjustment for the same variables (0.56, 0.53 to 0.59, vs 0.51, 0.50 to 0.52, p <0.002). Besides being associated with the presence of CHD, MPI TDI increased independently with increasing age and mean arterial blood pressure, whereas MPI conv increased independently with increasing age and mean arterial blood pressure and decreasing body mass index and heart rate ( Table 2 ).
| MPI conv | MPI TDI | |||
|---|---|---|---|---|
| Beta (95% CI) | p Value | Beta (95% CI) | p Value | |
| Age per 10 years | 0.010 (0.003 to 0.017) | 0.006 | 0.025 (0.019 to 0.031) | <0.0001 |
| Male gender | 0.019 (−0.001 to 0.040) | 0.06 | 0.004 (−0.013 to 0.021) | 0.64 |
| Body mass index per 5 kg/m 2 | −0.015 (−0.028 to −0.001) | 0.033 | 0.002 (−0.009 to 0.013) | 0.77 |
| Heart rate per 10 beats/min | −0.015 (−0.024 to −0.005) | 0.002 | 0.006 (−0.001 to 0.014) | 0.11 |
| Mean arterial blood pressure per 10 mm Hg | 0.013 (0.005 to 0.021) | 0.002 | 0.018 (0.011 to 0.025) | <0.0001 |
Risk of mortality increased with increasing tertiles of MPI TDI ( Figure 2 ), being >3 times as high in the third tertile compared to the first tertile (hazard ratio 3.3, 1.8 to 6.2, p <0.001).
MPI obtained from the 2 methods was significantly associated with overall mortality ( Table 3 ), and MPI TDI remained independently associated with overall mortality after multivariable adjustment for age, gender, body mass index, heart rate, mean arterial blood pressure, and CHD ( Table 3 ).
| Univariable | Multivariable Adjustment ⁎ | |||
|---|---|---|---|---|
| Hazard Ratio (95% CI) | p Value | Hazard Ratio (95% CI) | p Value | |
| Conventional myocardial performance index per 0.1 increase | 1.20 (1.04–1.38) | 0.010 | 1.11 (0.96–1.27) | 0.15 |
| Tissue Doppler imaging myocardial performance index per 0.1 increase | 1.31 (1.19–1.44) | <0.0001 | 1.18 (1.04–1.34) | 0.010 |
⁎ Adjustment for age, gender, body mass index, heart rate, mean arterial blood pressure, and ischemic heart disease.
Bland-Altman plots of intra- and interobserver differences of MPI TDI and MPI conv are shown in Figure 3 . For MPI TDI intraobserver variability analysis showed a mean difference ± SD of 0.016 ± 0.038 and interobserver variability analysis showed a mean difference of 0.010 ± 0.073. For MPI conv intraobserver variability analysis showed a mean difference of 0.013 ± 0.057 and interobserver variability analysis showed a mean difference of 0.082 ± 0.114.
Results
In total 1,100 subjects were examined with TDI and conventional echocardiography in this study. Forty-five were excluded due to inadequate quality of echocardiographic examination, and 19 were excluded due to atrial fibrillation or significant valvulopathy. Characteristics of the remaining subjects constituting the study population (n = 1,036) are listed in Table 1 . The study population was divided into groups with and without CHD at time of enrollment.
MPI conv remained significantly higher in the CHD group after multivariable adjustment for age, gender, body mass index, heart rate, and mean arterial blood pressure (0.44, 0.41 to 0.48, vs 0.39, 0.38 to 0.40, p <0.002). This pattern was the same for MPI TDI , which remained significantly higher in the CHD group after multivariable adjustment for the same variables (0.56, 0.53 to 0.59, vs 0.51, 0.50 to 0.52, p <0.002). Besides being associated with the presence of CHD, MPI TDI increased independently with increasing age and mean arterial blood pressure, whereas MPI conv increased independently with increasing age and mean arterial blood pressure and decreasing body mass index and heart rate ( Table 2 ).



