Inversion of the T waves (T−) in electrocardiographic leads with ST-segment elevation after the initiation of reperfusion therapy is considered a sign of reperfusion. However, the significance of T− on presentation before the initiation of reperfusion therapy is unclear. The aim of this study was to assess whether T− on presentation predicts patency of the infarct-related artery in patients with acute ST-segment elevation myocardial infarctions (STEMIs) who undergo primary percutaneous interventions. The medical records, electrocardiograms, and angiographic findings of 209 consecutive patients who underwent emergent coronary angiography as part of primary percutaneous coronary intervention protocol activation for STEMI were reviewed. A total of 179 patients (86%) had positive T waves (T+), 16 (8%) had biphasic T waves (T+/−), and 14 (7%) had T−. Patency of the infarct-related artery (Thrombolysis In Myocardial Infarction [TIMI] flow grades 2 and 3) was seen in 64.3% of the patients in the T− group compared with only 31.2% in the T+/− group and 19.0% in the T+ group (p <0.001). Among patients with anterior STEMI, patency of the infarct-related artery was seen in all 7 patients in the T− group, compared with 50% of the 4 patients in the T+/− group and 10.1% of the 79 patients in the T+ group (p <0.001). There were no significant differences in TIMI flow grade among the groups in patients with nonanterior STEMIs (p = 0.985). In conclusion, T− in the leads with maximal ST-segment elevation on the presenting electrocardiogram was associated with higher prevalence of patency of the infarct-related artery before intervention (64.3%), especially in patients with anterior STEMIs (100%).
In the present study, we assessed patency of the infarct-related artery before intervention in patients with ST-segment elevation myocardial infarctions (STEMIs) who underwent primary percutaneous coronary intervention (pPCI) at the Texas Heart Institute, St. Luke’s Episcopal Hospital (Houston, Texas), on the basis of T-wave morphology.
Methods
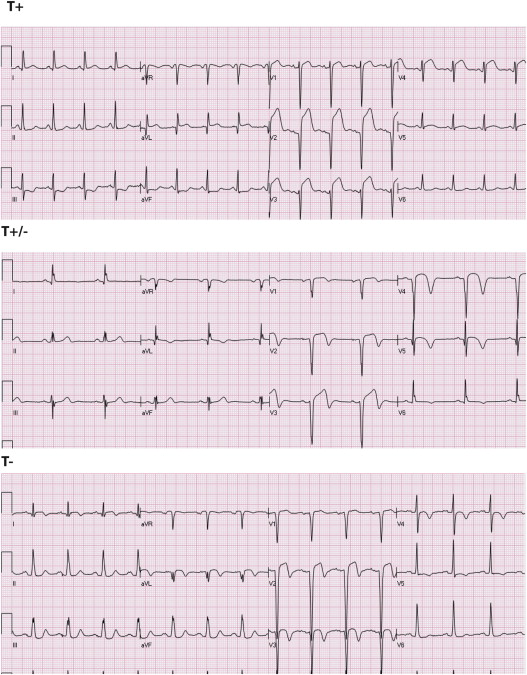
We reviewed the medical records of consecutive patients who presented to St. Luke’s Episcopal Hospital with suspected acute STEMI and for whom the pPCI protocol was activated and emergency coronary angiography was performed from November 3, 2010, through December 31, 2012. St. Luke’s Episcopal Hospital is a large, urban tertiary center located in Houston, Texas. Patients with left bundle branch block, ventricular rhythm, or electronic ventricular pacing were excluded. Patients who received thrombolytic therapy or underwent pPCI before arrival to St. Luke’s Episcopal Hospital and those who had postoperative infarctions were not included. We also excluded patients in whom culprit coronary artery lesions could not be identified and those with final diagnoses other than STEMI (takotsubo cardiomyopathy, myocarditis, etc). Demographic and clinical data were retrieved from the medical charts. Time from the onset of symptoms to presentation was retrieved from the pPCI quality assurance database. The presenting electrocardiograms of the patients were analyzed by 2 investigators (A.A. and Y.B.). The presence of ST-segment elevation, fulfilling the current guidelines for STEMI, was confirmed. The configuration of the T waves in the 2 leads with maximal ST-segment elevation was determined: (1) positive T waves (T+), (2) biphasic T waves (T+/−; initial positive deflection above the ST segment follows by negative deflection ≥0.5 mm below the isoelectric line), or (3) negative T waves (T−; negative T waves ≥0.5 mm below the isoelectric line without initial positive deflection) ( Figure 1 ). The readers were blinded to the angiographic data. The angiographic images were reviewed by 1 investigator (M.A.), who was blinded to the electrocardiographic data. The site of coronary artery occlusion and the initial Thrombolysis In Myocardial Infarction (TIMI) flow grade before intervention were determined.
The 3 groups were compared using chi-square analysis for categorical data and analysis of variance for continuous variables. A p value <0.05 was considered statistically significant.
Results
A total of 209 patients were included, of whom 179 (86%) had T+, 16 (8%) had T+/−, and 14 (7%) had T−. Baseline demographic and clinical data of the 3 groups are listed in Table 1 . There were no differences in gender among the groups. However, patients with T+ were younger. In contrast, there were fewer Caucasian patients and more African-American and Hispanic patients in the T− group. Fewer patients in the T+ group had histories of diabetes mellitus; however, there were no differences in the prevalence of hypertension, previous myocardial infarction, or previous coronary artery bypass graft surgery among the groups.
| Variable | T+ (n = 179) | T+/− (n = 16) | T− (n = 14) | p Value |
|---|---|---|---|---|
| Men | 126 (70%) | 11 (69%) | 8 (57%) | 0.584 |
| Age (yrs) | 61 ± 13 | 69 ± 12 | 65 ± 11 | 0.028 |
| Race/ethnicity | 0.008 | |||
| White | 117 (65%) | 10 (63%) | 2 (14%) | |
| Black | 34 (19%) | 2 (13%) | 7 (50%) | |
| Hispanic | 21 (12%) | 4 (25%) | 4 (29%) | |
| Asian | 7 (4%) | 0 | 1 (7%) | |
| Diabetes mellitus | 58 (33%) | 9 (56%) | 8 (57%) | 0.04 |
| Hypertension | 146 (82%) | 13 (81%) | 13 (93%) | 0.58 |
| No previous myocardial infarction | 168 (94%) | 14 (88%) | 13 (93%) | 0.547 |
| Previous coronary bypass | 15 (8%) | 4 (25%) | 1 (7%) | 0.093 |
| Infarct location | 0.009 | |||
| Anterior | 79 (44%) | 4 (25%) | 7 (50%) | |
| Inferior | 91 (51%) | 12 (75%) | 5 (36%) | |
| Anterior + inferior | 2 (1%) | 0 | 2 (14%) | |
| Lateral | 7 (4%) | 0 | 0 | |
| Time from symptom onset to pPCI (h) | 0.305 | |||
| <1 | 89 (50%) | 7 (44%) | 7 (50%) | |
| 1–3 | 29 (16%) | 5 (31%) | 1 (7%) | |
| 3–6 | 31 (17%) | 0 | 2 (14%) | |
| >6 | 30 (17%) | 4 (25%) | 4 (29%) | |
| Peak creatine kinase-MB (ng/ml) | 108 ± 138 | 69 ± 95 | 67 ± 104 | 0.266 |
| Peak troponin I (ng/ml) | 22.2 ± 22.4 | 23.8 ± 23.1 | 19.7 ± 20.4 | 0.877 |
| Revascularization procedures | ||||
| Primary percutaneous coronary intervention | 160 (90%) | 14 (88%) | 13 (93%) | 0.888 |
| Coronary artery bypass surgery | 8 (5%) | 4 (25%) | 1 (7%) | 0.004 |
| No revascularization | 16 (9%) | 0 | 1 (7%) | 0.093 |
In the T+/− group, there were more patients with inferior STEMIs and fewer patients with anterior STEMIs. Time from the onset of symptoms to pPCI was comparable among the 3 groups. Peak creatine kinase-MB and cardiac troponin I were comparable among the groups. There were no differences in the percentage of patients who were treated with pPCI among groups; however, more patients in the T+/− group underwent coronary artery bypass grafting and fewer were treated conservatively (without revascularization procedures).
Angiographic data are listed in Table 2 . The infarct-related artery was less often the left anterior descending coronary artery and more often the left circumflex coronary artery, left main coronary artery, or a graft in the T+/− group.
| Variable | T+ (n = 179) | T+/− (n = 16) | T− (n = 14) | p Value |
|---|---|---|---|---|
| Infarct-related coronary artery | 0.051 | |||
| Left anterior descending | 86 (48%) | 3 (19%) | 6 (43%) | |
| Left circumflex | 19 (11%) | 3 (19%) | 1 (7%) | |
| Right | 67 (37%) | 6 (38%) | 6 (43%) | |
| Left main | 1 (1%) | 1 (6%) | 0 | |
| Graft | 5 (3%) | 3 (19%) | 1 (7%) | |
| Other | 1 (1%) | 0 | 0 | |
| TIMI flow grade | <0.001 | |||
| 0 | 132 (74%) | 6 (38%) | 4 (29%) | |
| 1 | 14 (8%) | 5 (31%) | 1 (7%) | |
| 2 | 33 (18%) | 5 (31%) | 8 (57%) | |
| 3 | 0 | 0 | 1 (7%) |
TIMI flow grade 0 was seen more often in the T+ group (73.7%) than in the T+/− group (37.5%) or T− group (28.6%). Patency of the infarct-related artery (TIMI flow grade 2 or 3) was seen in 64.3% of the patients in the T− group and only 31.2% in the T+/− group and 18.0% in the T+ group (p <0.001).
In patients with anterior STEMIs, patency of the infarct-related artery was seen in all 7 patients in the T− group, compared with 50% of the 4 patients in the T+/− group and 10.1% of the 79 patients in the T+ group (p <0.001; Table 3 ). The sensitivity and specificity of T− for patency were 43.8% and 89.2%, respectively. In contrast, there were no significant differences in patency of the infarct related artery among the groups in patients with nonanterior STEMIs (p = 0.985; Table 3 ).
| TIMI Flow Grade | T+ (n = 79) | T+/− (n = 4) | T− (n = 7) | p Value |
|---|---|---|---|---|
| Anterior STEMI | <0.001 | |||
| 0 | 66 | 1 | 0 | |
| 1 | 6 | 1 | 0 | |
| 2 | 7 | 2 | 6 | |
| 3 | 0 | 0 | 1 | |
| Nonanterior STEMI | 0.114 | |||
| 0 | 66 | 5 | 4 | |
| 1 | 8 | 4 | 1 | |
| 2 | 26 | 3 | 2 | |
| 3 | 0 | 0 | 0 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


