Because right ventricular (RV) dysfunction predicts a poor outcome in patients with congenital heart disease (CHD), regular monitoring of RV function is indicated. To date, cardiac magnetic resonance (CMR) imaging has been the reference method. A more practical, more accessible, and accurate tool would be preferred. We defined normality regarding RV systolic function using healthy controls and tested the ability of real-time 3-dimensional echocardiographic (RT3DE) findings to identify patients with CHD with RV dysfunction. The cutoff values for the RV volumes and ejection fraction (EF) were derived from the CMR imaging findings from 41 healthy controls (mean age 27 ± 8 years, 56% men). In 100 patients with varying CHDs (mean age 27 ± 11 years, 65% men), both RT3DE data sets (iE33) and short-axis CMR imaging (1.5 T) were obtained within 2 hours. The RT3DE and CMR RV volumes and EF were calculated using commercially available software. Receiver operating characteristic curves were created to obtain the sensitivity and specificity of the RT3DE data to identify RV dysfunction. Applying the cutoff values derived from the healthy controls using the CMR data of patients with CHD, we identified 23 patients with an enlarged indexed end-diastolic volume, 29 patients with an enlarged indexed end-systolic volume, and 21 patients with an impaired RVEF. The best cutoff values predicting RV dysfunction using the RT3DE findings were identified (indexed end-diastolic volume >105 ml/m 2 , indexed end-systolic volume >54 ml/m 2 , and EF <43%). The RT3DE findings revealed 23 patients with impaired RVEF, with 95% sensitivity, 89% specificity, and a negative predictive value of 99%. In conclusion, real-time 3-dimensional echocardiography is a very sensitive tool to identify RV dysfunction in patients with CHD and could be applied clinically to rule out RV dysfunction or to indicate additional quantitative analysis of RV function.
The ideal index to assess right ventricular (RV) contractility—independent of the pre- and afterload, independent of heart size and mass, easy and safe to apply, and proven useful in the clinical setting—does not yet exist. Thus, determination of the ejection fraction (EF) is still the most commonly used method to assess systolic RV performance. Cardiac magnetic resonance (CMR) imaging has become the reference method for the assessment of RVEF but has a number of drawbacks, including limited availability, high costs, and time-consuming acquisition and analysis. Owing to the complex RV geometry and the presence of myocardial trabeculae, 2-dimensional echocardiography is considered inaccurate and a 3-dimensional imaging technology, such as real-time 3-dimensional echocardiography (RT3DE), is mandatory. Earlier studies have shown that RT3DE can assess RV volumes and EF in various patient groups. If proved to be a robust and reliable technique, RT3DE might replace CMR imaging for RV systolic functional assessment in a substantial proportion of patients. To be usable in clinical practice, a prerequisite is the reliability of RT3DE to detect RV dysfunction. This has not been previously studied. The purposes of the present study were to define normality regarding systolic RV function using CMR values derived from healthy controls and to test the ability of RT3DE to accurately identify RV dysfunction in patients with congenital heart disease (CHD), according to the reference method CMR imaging. For the purposes of the present study, the cutoff values for the RV volumes and EF were identified and applied to differentiate between normal and impaired RV function—to define RV dysfunction.
Methods
A total of 41 healthy controls underwent full-volume real-time 3-dimensional echocardiography and CMR imaging to establish the reference RV volume and EF values. The controls were employees of the university or hospital or their relatives who were willing to undergo a CMR scan. They were eligible for inclusion in the study if they had no medical history or current symptoms suggestive of cardiovascular disease, including hypertension or a systemic illness with a potential cardiovascular component such as diabetes or thyroid disease. Participants taking any cardiovascular medications were excluded from the present study.
In all included healthy controls the heart rate and blood pressure were measured (with the subject supine), and they underwent routine 2-dimensional echocardiography to exclude cardiac abnormalities.
A total of 100 consecutive patients, in sinus rhythm, with complex and/or surgically repaired CHD underwent full-volume RT3DE and CMR acquisition of the right ventricle. They were referred for CMR imaging for a quantitative analysis of their cardiac function for clinical reasons and underwent a RT3DE examination within 2 hours of CMR imaging to pursue comparable loading conditions.
The medical ethical committee approved the study, and all healthy controls, patients, and/or their parents (if required) provided written informed consent.
CMR images were acquired using a Signa 1.5 Tesla scanner (GE Medical Systems, Milwaukee, Wisconsin). The subjects were positioned supine with dedicated phased-array cardiac surface coils placed over the thorax. The CMR protocol included cine steady-state, free precision sequences in the short-axis planes to assess the RV volumes. Electrocardiographic gating and repeated breath holds were applied to minimize the influence of cardiac and respiratory motion.
The RV volumes were measured from a multisection image set of 8 to 12 contiguous slices parallel to the plane of the atrioventricular valves and covering the full-length of both ventricles. The imaging parameters were as follows: slice thickness 7 to 10 mm, interslice gap 0 mm, field of view 280 to 370 mm, phase field of view 0.75, matrix 160 × 128 mm, repetition time 3.5 ms, echo time 1.5 ms, and flip angle 45°.
One physician (HBZ) analyzed the CMR RV volumetric data set quantitatively on a commercially available Advanced Windows workstation (GE Medical Systems) using the Advanced Windows, version 5.1, of the MR Analytical Software System (Medis Medical Imaging Systems, Leiden, The Netherlands). The RV end-diastolic volume, end-systolic volume and EF were calculated using manual detection of the endocardial borders in end-systole and end-diastole with exclusion of trabeculae, as described by Robbers-Visser et al.
RT3DE harmonic imaging was performed using the iE33 ultrasound system (Philips Medical Systems, Best, The Netherlands) equipped with an X3-1 matrix array transducer with the patient in the left lateral decubitus position. To encompass the entire right ventricle into the RT3DE data set, a full-volume scan was acquired from a modified apical transducer position in harmonic mode from 7 R-wave–gated subvolumes during a single end-expiratory breath-hold. The output therefore was not truly real-time but was reconstructed from the 7 subvolumes. The depth and angle of the ultrasound sector were adjusted to a minimal level, still encompassing the entire right ventricle. Before each acquisition, the images were optimized for endocardial border visualization by modifying the time gain and compression and increasing the overall gain. An average of 3 data sets was acquired per patient to ensure optimal data sets without motion artifacts that might have occurred during the acquisition. The mean volume rate was 25 frames (range 14 to 38) per cardiac cycle. The data sets were digitally exported to a Tomtec server (Tomtec Imaging Systems, Unterschleißheim, Germany) connected to a terminal workstation for additional analyses.
The digital RT3DE RV data sets were analyzed off-line using the Tomtec 4-dimensional RV Function Program, version 4.0, by an investigator (HBZ) unaware of the results of the CMR measurements. This software performs 3-dimensional semiautomated border detection of the RV volumes over one cardiac cycle. It uses a physics-based modeling algorithm that makes no assumptions regarding RV geometry. The analysis of a RT3DE data set was judged accurate, when the apex and lateral wall were both visible in the 4-chamber view, allowing adequate tracing of the endocardial border.
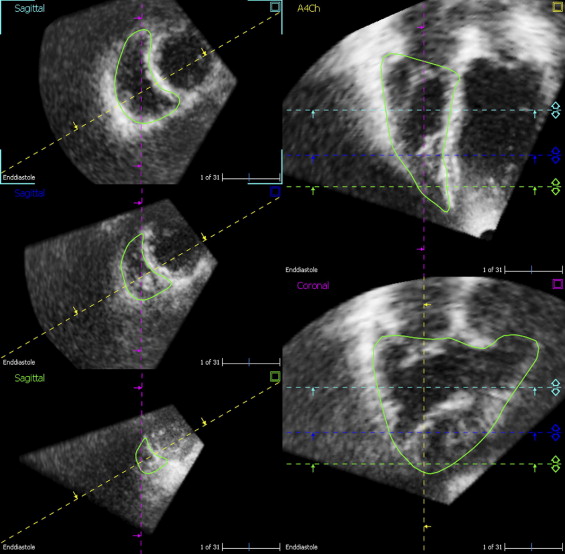
The functioning of the Tomtec analysis program ( Figure 1 ) has been previously reported in detail. In brief, the program starts with a screen displaying a short-axis view (top), an apical 4-chamber view (left), and a coronal view (right). The right ventricle must be outlined in the middle of the data set. Next, by movement of a horizontal axis, landmarks can be placed in the tricuspid and mitral valve orifices and apex. Subsequently the end-diastolic (largest RV volume) and end-systolic (smallest RV volume) phases are identified. The endocardial border contours are drawn onto the apical 4-chamber still frames in both end-diastole and end-systole. Using these contours, 2 reference markers are extrapolated onto the sagittal view in which the endocardial border contours are traced with care to include the 2 extrapolated reference markers. Next, the contours are drawn in the coronal view, again with attention to include the 3 reference markers extrapolated from the 4-chamber and sagittal views. After these steps, the software automatically delineates the RV endocardial border from the end-diastolic and end-systolic phases, and by sequential analysis the software creates an RV mathematic dynamic 3-dimensional model—referred to as “Beutel”—that represents changes in the RV cavity over the cardiac cycle. From this Beutel, the RV volumes and EF are calculated.
Statistical analysis was done using the Statistical Package for Social Sciences, version 15.0 (SPSS, Chicago, Illinois). The categorical data are summarized as numbers and percentages and the continuous data as the mean ± SD. Differences between patients and controls were analyzed using chi-square tests or Student’s t tests, as appropriate.
Both RT3DE and CMR volumes were indexed to the body surface area. The body surface area was calculated according to the formula by Dubois: body surface area (m 2 ) = weight (kg) 0.425 × height (cm) 0.725 × 71.84 × 10 −4 .
All statistical tests were 2-sided, and p <0.05 was considered statistically significant.
Because no standard on definition of RV dysfunction is available, we defined RV dysfunction as follows. Using the CMR volumetric data from the healthy controls, we identified a range of normal RV function using the mean ± 2 SDs. Next, we defined the indexes of RV dysfunction either as a diminished RVEF (less than the mean minus 2 SDs in healthy controls), an enlarged indexed end-diastolic volume or an enlarged indexed end-systolic volume (both greater than the mean plus 2 SDs in healthy controls).
Using these cutoff values, we dichotomized the CMR data derived from our CHD group. Receiver operating characteristic curves were created to predict RV dysfunction using the RT3DE data. From the receiver operating characteristic curves, the sensitivity and specificity of the RT3DE findings were derived, as well as the area under the curves. Next, 2 by 2 tables were created to calculate the positive and negative predictive values of the RT3DE findings to identify RV dysfunction using the CMR data. The cutoff RT3DE values to obtain the maximum sum of the sensitivity and specificity, the greatest sensitivity and specificity, were calculated.
Results
The baseline characteristics of the healthy controls (mean age 27 ± 8 years, 56% men) and the patients with CHD (mean age 27 ± 10 years, 65% men) are listed in Table 1 . The patients with CHD had a greater heart rate (p <0.001) and shorter stature (p = 0.04) than the healthy controls. Table 2 lists the types of CHD the patients had.
| Variable | Healthy Controls | Patients With CHD | p Value ⁎ | ||||
|---|---|---|---|---|---|---|---|
| All | Men | Women | All | Men | Women | ||
| Patients (n) | 41 | 23 | 18 | 100 | 65 | 35 | 0.33 |
| Age (years) | 27 ± 8 | 26 ± 9 | 28 ± 7 | 27 ± 10 | 26 ± 10 | 28 ± 11 | 0.89 |
| Age at initial repair (years) (n = 94) | — | — | — | 5 ± 10 | 6 ± 10 | 6 ± 12 | — |
| Age at reoperation (years) (n = 51) | — | — | — | 11 ± 10 | 11 ± 10 | 10 ± 10 | — |
| Heart rate (beats/min) | 64 ± 13 | 64 ± 14 | 63 ± 14 | 72 ± 12 | 70 ± 13 | 75 ± 11 | <0.001 |
| Systolic blood pressure (mm Hg) | 121 ± 14 | 128 ± 13 | 114 ± 12 | 125 ± 18 | 126 ± 17 | 123 ± 20 | 0.29 |
| Diastolic blood pressure (mm Hg) | 73 ± 8 | 74 ± 7 | 71 ± 9 | 72 ± 10 | 71 ± 10 | 73 ± 11 | 0.58 |
| Height (cm) | 177 ± 8 | 181 ± 6 | 171 ± 5 | 172 ± 13 | 176 ± 13 | 165 ± 7 | 0.04 |
| Weight (kg) | 70 ± 11 | 73 ± 10 | 66 ± 11 | 68 ± 15 | 70 ± 17 | 63 ± 12 | 0.36 |
| Body mass index (kg/m 2 ) | 22 ± 3 | 22 ± 3 | 23 ± 3 | 22 ± 4 | 22 ± 5 | 23 ± 4 | 0.80 |
| Body surface area (m 2 ) | 1.9 ± 0.2 | 1.9 ± 0.1 | 1.8 ± 0.1 | 1.8 ± 0.3 | 1.8 ± 0.4 | 1.7 ± 0.2 | 0.04 |
⁎ Difference between healthy controls and patients with CHD.
| Pathologic Finding | Patients (n) |
|---|---|
| Tetralogy of Fallot | 38 |
| Aortic valve abnormality | 17 |
| Pulmonary stenosis with or without ventricular septal defect | 12 |
| Pulmonary atresia with or without ventricular septal defect | 4 |
| Transposition of great arteries, atrial switch | 10 |
| Transposition of great arteries, arterial switch | 9 |
| Coarctation of aorta | 2 |
| Ebstein’s anomaly | 2 |
| Double outlet right ventricle | 1 |
| Double inlet left ventricle | 1 |
| Ventricular septal defect | 1 |
| Anomalous pulmonary venous connection | 1 |
| Perinatal tricuspid insufficiency | 1 |
| Congenital hypertrophic cardiomyopathy | 1 |
Table 3 lists the absolute and indexed RV volumes and EF obtained using CMR imaging The patients with CHD had a greater indexed end-diastolic volume and end-systolic volume and lower EF (all p <0.001). Similar outcomes were measured using RT3DE. The end-diastolic volume and end-systolic volume were greater in the patients with CHD (p <0.001) and their EF was lower (p <0.001; Table 4 ).
| Variable | Healthy Controls | Patients With CHD | p Value ⁎ | ||||
|---|---|---|---|---|---|---|---|
| All | Men | Women | All | Men | Women | ||
| Absolute values | |||||||
| End-diastolic volume (ml) | 158 ± 32 | 172 ± 29 | 139 ± 27 | 193 ± 72 | 195 ± 72 | 190 ± 75 | <0.001 |
| End-systolic volume (ml) | 65 ± 18 | 70 ± 17 | 58 ± 17 | 94 ± 47 | 96 ± 49 | 91 ± 46 | <0.001 |
| Stroke volume (ml) | 93 ± 19 | 107 ± 18 | 82 ± 15 | 100 ± 34 | 101 ± 34 | 99 ± 36 | 0.15 |
| Ejection fraction (%) | 60 ± 6 | 60 ± 6 | 59 ± 6 | 53 ± 9 | 52 ± 10 | 53 ± 8 | <0.001 |
| Normalized to body surface area | |||||||
| Indexed end-diastolic volume (ml/m 2 ) | 86 ± 21 | 90 ± 15 | 79 ± 13 | 109 ± 37 | 108 ± 36 | 112 ± 39 | <0.001 |
| Indexed end-systolic volume (ml/m 2 ) | 35 ± 11 | 37 ± 9 | 33 ± 9 | 54 ± 25 | 53 ± 26 | 54 ± 24 | <0.001 |
| Indexed stroke volume (ml/m 2 ) | 51 ± 12 | 53 ± 9 | 46 ± 6 | 56 ± 18 | 55 ± 17 | 59 ± 20 | 0.04 |
⁎ Difference between healthy controls and patients with CHD.
| Variable | Healthy Controls | Patients With CHD | p Value ⁎ | ||||
|---|---|---|---|---|---|---|---|
| All | Men | Women | All | Men | Women | ||
| Absolute values | |||||||
| End-diastolic volume (ml) | 127 ± 32 | 144 ± 31 | 108 ± 22 | 170 ± 61 | 175 ± 60 | 160 ± 61 | <0.001 |
| End-systolic volume (ml) | 58 ± 16 | 66 ± 14 | 48 ± 10 | 96 ± 44 | 98 ± 44 | 79 ± 35 | <0.001 |
| Stroke volume (ml) | 69 ± 19 | 78 ± 20 | 60 ± 14 | 80 ± 26 | 80 ± 24 | 80 ± 30 | 0.001 |
| Ejection fraction (%) | 55 ± 5 | 54 ± 5 | 56 ± 5 | 48 ± 9 | 46 ± 9 | 52 ± 7 | <0.001 |
| Normalized to body surface area | |||||||
| Indexed end-diastolic volume (ml/m 2 ) | 68 ± 18 | 73 ± 14 | 66 ± 10 | 96 ± 31 | 97 ± 30 | 94 ± 32 | <0.001 |
| Indexed end-systolic volume (ml/m 2 ) | 31 ± 9 | 34 ± 6 | 27 ± 5 | 51 ± 22 | 53 ± 23 | 46 ± 19 | <0.001 |
| Indexed stroke volume (ml/m 2 ) | 37 ± 11 | 39 ± 9 | 33 ± 6 | 45 ± 14 | 44 ± 12 | 47 ± 16 | 0.005 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


