After emergency orthopedic–geriatric surgery, cardiac complications are an important cause of morbidity and mortality. The utility of N-terminal pro–brain natriuretic peptide (NT–pro-BNP) for the prediction of cardiac complications and mortality was evaluated. NT–pro-BNP was tested pre- and postoperatively in 89 patients >60 years of age. They were followed for 2 years for cardiac complications (defined as acute myocardial infarction, congestive cardiac failure, atrial fibrillation or major arrhythmia) or death. Receiver operating characteristic curves were constructed to determine the optimal discriminatory level for cardiac events and death using NT–pro-BNP. Twenty-three patients (25.8%) sustained an in-hospital postoperative cardiac complication. Total all-cause mortality was 3 of 89 (3.4%) in hospital, 21 of 89 (23.6%) at 1 year, and 27 of 89 (30.3%) at 2 years. Median preoperative and postoperative NT–pro-BNP levels were higher in patients who had an in-hospital cardiac event compared to those without (387 vs 1,969 pg/ml, p <0.001; and 676 vs 7,052 pg/ml, p <0.001 respectively). The optimal discriminatory level for preoperative NT–pro-BNP was 842 pg/ml and that for postoperative NT–pro-BNP was 1,401 pg/ml for the prediction of in-hospital cardiac events and 1- and 2-year mortality. Preoperative NT–pro-BNP ≥842 pg/ml (odds ratio 11.6, 95% confidence interval 2.1 to 65.0, p = 0.005) was an independent predictor of in-hospital cardiac complications using multivariate analysis and pre- and postoperative NT–pro-BNP levels were independent predictors of 2-year cardiovascular events. Patients who had preoperative NT–pro-BNP ≥842 pg/ml or postoperative NT–pro-BNP ≥1,401 pg/ml had significantly worse survival using log-rank testing (p <0.001) and these variables independently predicted 2-year mortality. In conclusion, increase pre- and postoperative NT–pro-BNP levels are independent predictors of in-hospital cardiac events and 1- and 2-year mortality in older patients undergoing emergency orthopedic surgery.
The value of cardiac biomarkers to predict cardiac complications after orthopedic surgery is not well studied. Troponin has been more recently evaluated in orthopedic populations and predicts cardiac complications and mortality at 1 year, even in asymptomatic patients. There is growing interest in new cardiac biomarkers such as brain natriuretic peptide (BNP) and N-terminal pro-BNP (NT–pro-BNP). BNP and its inactive cleavage product NT–pro-BNP are released in response to cardiac stretch and ischemia, with plasma levels correlating to extent of myocardial ischemia. Furthermore, these markers can identify patients at high risk of further cardiovascular events, hospital admission, and death in patients with stable coronary artery disease or acute coronary syndromes. To date, the utility of NT–pro-BNP as a prognostic marker after orthopedic surgery has been limited to small studies, mainly in elective surgical patients. Previous noncardiac surgical studies have focused on patients with vascular disease, a population that has the traditional risk factors for ischemic heart disease or elective surgical patients. Meta-analyses have demonstrated that increased NT–pro-BNP levels predict short- and longer-term cardiac complications. The aim of this study was to determine whether pre- and postoperative NT–pro-BNP levels in an emergency orthopedic population are associated with in-hospital postoperative cardiac events, mortality, and long-term cardiovascular outcomes.
Methods
This prospective observational study recruited 119 consecutive patients from the orthopedic–geriatric unit from the Northern Hospital (Epping, Victoria, Australia) from April to December 2006. Ethics approval was given by the institutions human research and ethics committee and written informed consent was obtained for each patient. Patients were included if they were >60 years of age and underwent emergency orthopedic surgery for fractures or acute orthopedic conditions such as septic arthritis affecting the lower limb. Patients underwent standard surgery with routine perioperative care including continuation of cardiac medications and prophylactic anticoagulation to prevent deep venous thrombosis, where appropriate. All patients were provided with routine care by the orthopedic–geriatric unit. The attending unit ordered serum troponin I levels if clinically indicated, but NT–pro-BNP is not routinely tested in this center.
Venous blood was sampled before surgery and on postoperative days 1, 2, and 3 for measurement of troponin I and NT–pro-BNP. Blood was collected in a standard manner by pathology nurses on the ward and then centrifuged on arrival at the laboratory. Serum was then separated in aliquots and stored at −80°C until testing for NT–pro-BNP and troponin I, which occurred ≥30 days after collection for troponin I so that patients would continue to receive usual care during the postoperative period and at the conclusion of the study for NT–pro-BNP. Therefore, these results were not known in real time and investigators and patients were blinded to these results. Testing for troponin I has been described elsewhere, and the Architect STAT troponin I assay (Abbott Diagnostics) was used. Levels >0.03 μg/L (99th percentile of a healthy reference population) were considered abnormal and indicative of myocardial injury. NT–pro-BNP levels were tested using the Elecsys electrochemiluminescence immunoassay ECLIA proBNP II assay on a Roche Cobas E170 analyzer. The first available postoperative blood sample was tested for each patient. This assay used 2 polyclonal antibodies that recognized epitopes located on the N-terminal part of pro-BNP. The lower limit of the detection range (sensitivity) was 5 pg/ml. Within-run coefficients of variation are 1.9% at a concentration of 64 pg/ml and 1.3% at 14,142 pg/ml. Total precision coefficients of variation are 3.1% at a concentration of 36 pg/ml and 2.7% at 125 pg/ml. Assays for this study were performed by an experienced laboratory scientist blinded to a patient’s clinical data and troponin levels.
Patient characteristics and medical and demographic details were obtained by a physician independent of the treating unit by reviewing medical documentation. Cardiac complications and outcomes were determined if documented in medical records by the treating orthopedic–geriatric unit. A cardiac event was defined as acute myocardial infarction (diagnosed using standard criteria ), congestive cardiac failure (diagnosed by clinical signs and confirmatory investigations e.g., chest x-ray), atrial fibrillation (new-onset or destabilization of pre-existing atrial fibrillation), or major arrhythmia (defined as ventricular tachycardia or fibrillation).
Patients or carers were contacted by telephone at 1 year and 2 years after admission using a semistructured interview. In addition, medical records were examined and primary care physicians contacted if additional information was required. The primary end point was death and secondary data collected included cardiac events.
Normally distributed continuous data were expressed as mean ± SD and compared using Student’s t test. Non-normally distributed continuous data (e.g., NT–pro-BNP levels) were expressed as medians with ranges and compared using Mann-Whitney U statistic. NT–pro-BNP levels were dichotomized according to the optimal cut-off value established from receiver operating characteristic (ROC) curve analysis. Linear regression was used for continuous variables. Univariate logistic regression was performed to evaluate the association between baseline patient characteristics and in-hospital cardiac events. Predictors with p values <0.05 in univariate analysis were candidates for the multivariate logistical regression model using the enter or simultaneous method of variable entry using a maximum of 6 variables at a time to ensure stability. Important variables retained in all multivariate models included age, creatinine, and premorbid cardiac disease. For predictors of longer-term 2 year cardiac events and mortality, because the time to event was known, the multivariate cox proportional hazards model was used. Kaplan-Meier curves were constructed to determine survival after orthopedic surgery. Survival between groups was compared using log-rank testing. A p value <0.05 (2-tailed) was considered statistically significant for all analyses. Statistical analysis was conducted using SPSS 17.0 (SPSS, Inc., Chicago, Illinois) and Excel 11 (Microsoft, Redmond, Washington).
Results
Eighty-nine patients (mean ± SD 79 ± 10 years of age) were included in this study, and 27 of 102 (26%) studied were men. Table 1 lists patient characteristics. Twenty-seven patients were excluded because 10 had operations affecting the upper limb, 7 did not have stored blood, 2 did not have surgery, 5 declined participation, 1 died preoperatively, and 2 withdrew. Main forms of surgery were internal fixation of fractures, hemiarthroplasties, and general anesthetic and manipulation of plaster. Mean length of stay was 12 ± 8 days. Inpatient mortality rate for this study was 3 of 89 (3.4%). These patients died on days 12, 49, and 53 from (1) fat embolism, (2) myocardial infarction, heart failure, and pneumonia, and (3) sepsis.
| Variable | All Patients (n = 89) | In-Hospital Postoperative Cardiovascular Event | OR (95% CI) | p Value ⁎ | |
|---|---|---|---|---|---|
| Yes (n = 23) | No (n = 66) | ||||
| Age (years), mean ± SD | 79.9 ± 9.6 | 84.3 ± 7.9 | 78.4 ± 9.9 | 1.1 (1.0–1.1) | 0.015 |
| Men | 25 (28.1%) | 10 (43%) | 15 (23%) | 2.6 (1.0–7.1) | 0.061 |
| Number of co-morbidities, mean ± SD | 2.8 ± 1.8 | 4.0 ± 1.9 | 2.4 ± 1.5 | 1.8 (1.3–2.4) | <0.001 |
| Type of co-morbidity | |||||
| Ischemic heart disease | 29 (33%) | 12 (52%) | 17 (26%) | 3.1 (1.2–8.4) | 0.023 |
| Congestive cardiac failure | 14 (16%) | 11 (48%) | 3 (5%) | 19.3 (4.7–79.5) | <0.001 |
| Hypertension | 60 (67%) | 17 (74%) | 43 (65%) | 1.5 (0.5–4.4) | 0.442 |
| Atrial fibrillation | 14 (16%) | 5 (22%) | 9 (14%) | 1.8 (0.5–5.9) | 0.362 |
| Renal failure | 17 (19%) | 12 (52%) | 5 (8%) | 13.1 (3.8–44.6) | <0.001 |
| Dementia | 24 (27%) | 9 (39%) | 15 (23%) | 2.2 (0.7–6.0) | 0.132 |
| Diabetes mellitus | 18 (20%) | 6 (26%) | 12 (18%) | 1.6 (0.5–4.9) | 0.419 |
| Chronic obstructive pulmonary disease | 8 (9%) | 4 (17%) | 4 (6%) | 3.3 (0.7–14.3) | 0.117 |
| Stroke | 12 (14%) | 4 (17%) | 8 (12%) | 1.5 (0.4–5.6) | 0.526 |
| Smoker | 18 (20%) | 5 (22%) | 13 (20%) | 1.1 (0.4–3.6) | 0.834 |
| Malignancy | 11 (12%) | 3 (13%) | 8 (12%) | 1.1 (0.3–4.5) | 0.908 |
| Type of medication | |||||
| β blocker | 29 (33%) | 10 (44%) | 19 (29%) | 1.9 (0.7–5.1) | 0.199 |
| Antiplatelet agent | 36 (40%) | 13 (57%) | 23 (35%) | 2.4 (0.9–6.4) | 0.072 |
| Warfarin | 8 (9%) | 2 (9%) | 6 (9%) | 1.0 (0.2–5.1) | 0.954 |
| Angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker | 45 (51%) | 12 (52%) | 33 (50%) | 1.1 (0.4–2.8) | 0.858 |
| Calcium channel blocker | 18 (20%) | 3 (13%) | 15 (23%) | 0.5 (0.1–1.9) | 0.326 |
| Nitrate | 10 (11%) | 7 (30%) | 3 (5%) | 9.1 (2.1–39.5) | 0.003 |
| Diuretic | 32 (36%) | 12 (52%) | 20 (30%) | 2.5 (0.9–6.6) | 0.064 |
| Statin | 29 (33%) | 8 (35%) | 21 (32%) | 1.1 (0.4–3.1) | 0.794 |
| Nonsteroidal anti-inflammatory drug | 7 (8%) | 2 (9%) | 5 (8%) | 1.2 (0.2–6.4) | 0.864 |
| Fracture type | 0.4 (0.1–1.4) | 0.155 | |||
| Neck of femur | 63 (71%) | 19 (83%) | 44 (67%) | ||
| Lower limb | 26 (29%) | 4 (17%) | 22 (33%) | ||
| Time to surgery (days), mean ± SD | 2.0 ± 2.0 | 2.5 ± 2.2 | 1.7 ± 1.8 | 1.2 (1.0–1.5) | 0.101 |
| Anesthetic type | 1.4 (0.5–3.6) | 0.496 | |||
| General | 48 (54%) | 11 (48%) | 37 (56%) | ||
| Spinal or regional | 41 (46%) | 12 (52%) | 29 (44%) | ||
| Length of surgery (hours), mean ± SD | 1.4 ± 0.5 | 1.4 ± 0.5 | 1.4 ± 0.5 | 0.9 (0.3–2.4) | 0.752 |
⁎ Unadjusted p value for predictors of postoperative cardiovascular complications.
Median preoperative NT–pro-BNP level was 543 pg/ml (range 15 to 32,562; Table 2 ). Median postoperative NT–pro-BNP was 1,051 pg/ml (range 69 to 47,671). Of the 89 patients, 81 patients had preoperative NT–pro-BNP tested and 87 had a postoperative NT–pro-BNP test performed within the first 3 postoperative days. Reasons why blood was not tested in all 89 patients include not enough serum being stored for testing and blood samples not available (8 samples) or not stored in a timely manner (2 samples). Of the 87 patients with postoperative NT–pro-BNP levels, levels were obtained in 81 on postoperative day 1, 4 on day 2, and 2 on day 3.
| All Patients (n = 89) | In-Hospital Postoperative Cardiovascular Event | OR (95% CI) | p Value ⁎ | ||
|---|---|---|---|---|---|
| Yes (n = 23) | No (n = 66) | ||||
| Preoperative N-terminal pro–brain natriuretic peptide (pg/ml), median (range) | 543 (15–32,562) | 1,969 (104–32,562) | 387 (15–18,502) | 24.4 (5.1–117.7) | <0.001 |
| Postoperative N-terminal pro–brain natriuretic peptide (pg/ml), median (range) | 1,051 (69–47,671) | 7,052 (580–47,671) | 676 (69–19,045) | 7.9 (2.5–24.7) | <0.001 |
| Preoperative troponin increase | 24 (27%) | 14 (61%) | 10 (15%) | 8.7 (3.0–25.5) | <0.001 |
| Postoperative troponin increase | 48 (54%) | 20 (87%) | 28 (42%) | 9.0 (2.4–33.5) | 0.001 |
| Preoperative hemoglobin (g/L), mean ± SD | 116.3 ± 18.3 | 109.3 ± 19.0 | 118.7 ± 17.5 | 0.97 (0.94–1.0) | 0.038 |
| Postoperative hemoglobin (g/L), mean ± SD | 99.9 ± 18.5 | 99.1 ± 15.1 | 100.2 ± 19.6 | 1.0 (0.97–1.0) | 0.823 |
| Preoperative creatinine (μmol/L), mean ± SD | 98.8 ± 50.2 | 120.6 ± 60.7 | 90.8 ± 43.6 | 1.01 (1.001–1.02) | 0.024 |
| Postoperative creatinine (μmol/L), mean ± SD | 95.6 ± 52.0 | 126.7 ± 76.9 | 84.8 ± 34.6 | 1.02 (1.00–1.03) | 0.004 |
⁎ Unadjusted p value for predictors of postoperative cardiovascular complications.
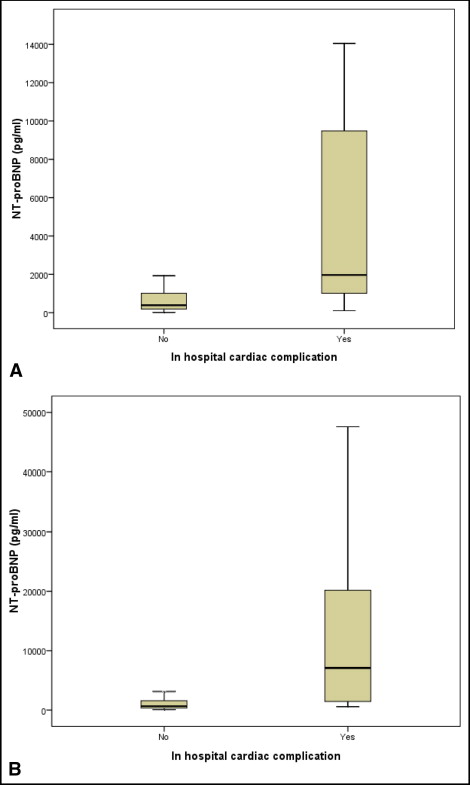
There were 23 of 89 patients (25.8%) who sustained an in-hospital cardiac complication. Table 1 presents baseline patient characteristics and association with in-hospital postoperative cardiovascular complications. There were 10 in-hospital non–ST-segment elevation myocardial infarctions, 8 episodes of atrial fibrillation, and 13 patients had congestive cardiac failure diagnosed by the treating unit. Of the 3 inpatient deaths, 2 patients sustained a myocardial infarction before death. Preoperative median NT–pro-BNP was significantly higher in patients who had an in-hospital cardiac event compared to those without (median 387 vs 1,969 pg/ml, p <0.001; Figure 1 ). Postoperative median NT–pro-BNP was significantly higher in patients who sustained an in-hospital cardiac event compared to those who did not (676 vs 7,052 pg/ml, p <0.001; Figure 1 ).
A ROC curve was constructed to predict in-hospital postoperative cardiovascular events using preoperative NT–pro-BNP levels ( Figure 2 ). A cut-off value of 842 pg/ml was identified as the optimal predictor of postoperative in-hospital complications representing the optimal tradeoff between sensitivity and specificity. The area under the curve was 0.82 (95% confidence interval [CI] 0.70 to 0.93, p <0.001), sensitivity 90%, specificity 74%, positive predictive value 54%, and negative predictive value 96%. Similarly, a ROC curve was drawn using postoperative NT–pro-BNP levels to predict in-hospital postoperative cardiovascular events ( Figure 2 ). The threshold for postoperative NT–pro-BNP was determined to be 1,401 pg/ml, and area under the curve was 0.85 (95% CI 0.76 to 0.94, p <0.001), yielding a sensitivity of 71%, specificity 71%, positive predictive value 46%, and negative predictive value 88%. In fact, a preoperative NT–pro-BNP cut-off value of 842 pg/ml and a postoperative level of 1,401 pg/ml were also identified as optimal predictor levels for 1- and 2-year mortality.




