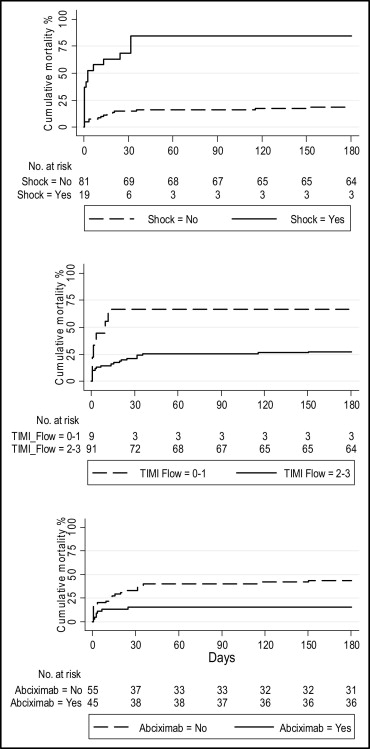
The optimal reperfusion strategy in very elderly patients with ST-segment elevation myocardial infarction is still a subject of debate. The aim of this multicenter study was to determine the medium-term outcomes of nonagenarians after primary percutaneous intervention for ST-segment elevation myocardial infarction. A systematic review of the databases of 7 Italian centers showed that these had performed 5,023 primary angioplasties over the previous 5 years, 100 of which (2%) involved patients ≥90 years old. Thirty-five subjects were in Killip class III or IV at time of presentation, 78 had multivessel coronary artery disease, and mean ejection fraction was 0.40 ± 0.12%. In-hospital mortality was 19% and was significantly higher in patients with shock (58% vs 10%, p <0.001). Survival rate after 6 months was 68%: 16% in those with Killip class IV at admission and 81% in the remaining patients (p <0.001). Cox regression analysis identified 3 independent predictors of 6-month mortality: cardiogenic shock at presentation (hazard ratio [HR] 10.82, 95% confidence interval [CI] 4.51 to 25.93, p <0.001), Thrombolysis In Myocardial Infarction myocardial flow after percutaneous coronary intervention (HR 0.19, 95% CI 0.07 to 0.50, p = 0.001), and abciximab administration (HR 0.32, 95% CI 0.13 to 0.78, p = 0.01). In conclusion, the results of this multicenter study suggest that selected nonagenarians with acute myocardial infarction benefit from successful primary angioplasty. The treatment does not affect the poor prognosis of patients presenting with cardiogenic shock, but the administration of abciximab seems to have a positive effect on 6-month mortality.
The aim of this multicenter study was to evaluate the short- and medium-term outcomes of nonagenarians with ST-segment elevation myocardial infarction (STEMI) systematically treated with primary angioplasty.
Methods
The study involved 7 Italian centers that systematically use primary percutaneous coronary intervention (PCI) in patients with STEMI regardless of their age. A systematic review of their databases showed that they had performed 5,023 primary PCIs over the previous 5 years, 100 of which (2%) involved subjects ≥90 years old and formed the subject of this analysis. Inclusion criteria for direct PCI were chest pain persisting for >30 minutes with electrocardiographic ST-segment elevation ≥0.1 mV in ≥2 contiguous leads and admission within 6 hours of symptom onset (from 6 to 24 hours for patients with evidence of continuing ischemia). Exclusion criteria were severe cognitive impairment, an inability to obtain informed consent, and a history of bleeding diathesis. Cardiac catheterization and PCI were performed using the standards of each center. All patients received aspirin (325 to 500 mg) before the procedure and clopidogrel (300 to 600 mg). The choice of anticoagulation or the use of glycoprotein IIb/IIIa inhibitor (abciximab) was left to the physician’s judgment.
Cardiogenic shock was determined by conventional clinical criteria of hypotension and signs of peripheral hypoperfusion in the presence of pulmonary congestion that did not resolve with inotropic agents or possibly mechanical support.
A successful procedure was defined as (1) achievement of Thrombolysis In Myocardial Infarction (TIMI) grade 2 or 3 flow, (2) <50% residual stenosis, and (3) absence of any major clinical adverse cardiac events within 24 hours. A failed procedure was defined as resulting in TIMI grade 0 to 1 flow regardless of residual stenosis, with the absence of any major clinical adverse cardiac events within 24 hours. A complicated procedure was defined as resulting in death, reinfarction, emergent revascularization, or cerebrovascular accident within 24 hours. Reinfarction was defined as an increase in creatinine kinase to >2 times the initial value, associated with a creatinine kinase-MB fraction >10% of total creatinine kinase.
Major and minor bleeding events were defined using the criteria of the TIMI trial group, and acute renal failure as an increase in serum creatinine ≥25% within 72 hours of angioplasty, with a peak creatinine level ≥2.0 mg/dl.
Severe clinical events, such as death, cardiac death, cerebrovascular accident, reinfarction, new revascularization (with PCI or coronary artery bypass surgery), and severe bleeding were evaluated during hospitalization and at follow-up.
At least 6 months’ follow-up data were available for all surviving patients; these data were obtained during a patient visit to outpatient clinics or by a telephone interview.
Continuous variables are expressed as mean ± 1 SD, and discrete variables as absolute values and percentages. Six-month survival/mortality was first evaluated with Kaplan-Meier estimators and log-rank tests and then with a multiple Cox proportional hazard model that included the covariates center and gender and the variables associated with mortality at univariate analysis. Data were statistically analyzed using STATA 11 (STATA Corp. LP, College Station, Texas).
Results
Patients’ mean age was 92.1 ± 2.1 years (range 90 to 98); their clinical and procedural characteristics are presented in Tables 1 and 2 . Forty-three of the 100 patients had an anterior wall acute MI (AMI), 19 presented with cardiogenic shock, and 16 were in Killip class III. Mean left ventricular ejection fraction recorded during echocardiographic examination in the emergency department was 0.40 ± 0.12%. Seventy-eight percent of patients had multivessel coronary artery disease. Mean time from symptom onset to PCI was 248 ± 122 minutes, and door-to-balloon time was 148 ± 137 minutes.
| Variable | |
|---|---|
| Age (years) | 92.1 ± 2.1 |
| Men | 44 |
| Body/mass index (kg/m 2 ) | 24.3 ± 5.2 |
| Hypertension | 58 |
| Hyperlipidemia | 68 |
| Diabetes mellitus | 19 |
| Previous myocardial infarction | 18 |
| Previous coronary bypass | 9 |
| Previous percutaneous coronary intervention | 16 |
| Left ventricular ejection fraction on admission (%) | 0.40 ± 0.12 |
| ST-segment elevation myocardial infarction location | |
| Anterior | 43 |
| Nonanterior | 57 |
| Killip class before percutaneous coronary intervention | |
| I | 51 |
| II | 14 |
| III | 16 |
| IV | 19 |
| Time from symptoms to percutaneous coronary intervention (minutes) | 248 ± 122 |
| Hemoglobin at admission (g/L) | 10.8 ± 1.1 |
| Creatinine at admission (mg/dl) | 1.4 ± 0.4 |
| Infarct-related artery stenting | 94 |
| Variable | |
|---|---|
| Door-to-balloon time (minutes) | 148 ± 137 |
| Single-vessel coronary artery disease | 22 |
| Multivessel coronary artery disease | 78 |
| Single-lesion percutaneous coronary intervention | 73 |
| Multilesion percutaneous coronary intervention | 18 |
| Infarct-related coronary artery | |
| Left anterior descending | 40 |
| Left circumflex | 24 |
| Right | 30 |
| Left main | 6 |
| Thrombolysis In Myocardial Infarction grade flow after procedure | |
| 0 | 7 |
| 1 | 2 |
| 2 | 9 |
| 3 | 82 |
| Successful percutaneous coronary intervention | 85 |
| Failed percutaneous coronary intervention | 4 |
| Complicated percutaneous coronary intervention | 11 |
| Use of protection device | 10 |
| Intra-aortic balloon pumping | 7 |
| Creatinine kinase peak (mg/dl) | 1,782 ± 1,455 |
| Abciximab administration | 45 |
The procedure was successful in 85 patients, complicated in 11, and failed in 4; abciximab was administered in 45% of cases. Preprocedural minimal lumen diameter of the stenotic segment was 0.13 ± 0.02 mm and increased to 2.98 ± 0.47 mm after angioplasty. Mean lesion length was 14.9 ± 8.2 mm.
In-hospital mortality rate was 19%; 11 of 19 patients presented with cardiogenic shock (58%) and 8 of 81 (10%) without shock (p <0.001). Major bleeding complications occurred in 3 patients who developed groin hematoma with a decrease in hemoglobin levels to ≥4.0 g/L and received blood transfusions; none of these patients had received a glycoprotein IIb/IIIa receptor inhibitor. Reversible acute renal failure also occurred in 3 patients. Mean length of hospitalization was 7 ± 5 days.
Six-month survival rate was 68%. One patient died from pneumonia 1 month after discharge, and 31 had cardiac death; mortality rates were 84% in patients in Killip class IV at admission and 19% in the other patients (p >0.001; Figure 1 ). Two subjects were rehospitalized because of congestive heart failure, and 1 developed a new episode of AMI.