Older patients with aortic stenosis cannot always be offered conventional surgical aortic valve replacement at an acceptable risk. Transcatheter aortic valve implantation (TAVI) is currently considered an alternative treatment option with lower periprocedural risks. However, its effect on post-TAVI quality of life and clinical improvement has not been systematically and prospectively evaluated in those of advanced age. Thus, the aim of the present study was to assess the clinical improvement in geriatric patients after TAVI, with a special emphasis on quality of life. In the present study, we assessed the quality of life and brain natriuretic peptide in patients aged >80 years, before and 6 months after transfemoral CoreValve implantation. Of 87 prospectively studied patients with severe, symptomatic aortic stenosis at an age of ≥81 years, 80 survived for 6 months and were able to attend the follow-up visit with a quality of life assessment, using the Medical Outcomes Trust Short Form 36-Item Health Survey (average age 86 ± 2.9 years). The average scores of all 8 health components had improved significantly after TAVI. The greatest gain was seen in physical functioning (improvement from 23.4 ± 6.0 to 67.8 ± 13.7; p <0.001). The lowest gain was seen in bodily pain (improved from 37.5 ± 9.4 to 51.3 ± 11.5; p <0.05). Similarly, both the physical and the mental component summary scores improved significantly. This was consistent with significant improvement in brain natriuretic peptide levels (5,770 ± 8,016 to 1,641 ± 3,650 ng/L; p <0.0001). In conclusion, the results of the present study have shown a significant clinical benefit from TAVI in a patient population aged ≥81 years.
In high-risk patients with severe aortic stenosis, transcatheter aortic valve implantation (TAVI) offers a good alternative to medical therapy. Many eligible patients for this procedure are of advanced age and require a more specific characterization of postprocedural success. In the present study, we assessed, for the first time, the quality of life of patients aged >80 years, before and 6 months after transfemoral CoreValve implantation, using the Medical Outcomes Trust Short Form 36-Item Health Survey. In addition, we measured the N-terminal pro-brain natriuretic peptide levels.
Methods
From July 2008 to January 2010, 108 consecutive patients were treated with transfemoral CoreValve implantation at our institution. All patients had symptomatic aortic stenosis with an orifice area of <1 cm 2 and were considered high-risk surgical patients with either a logistic European System for Cardiac Operative Risk Evaluation (EuroSCORE) of ≥20% or specific co-morbidities that would exclude surgical therapy, such as porcelain aorta, chest radiotherapy, or a severely reduced lung capacity. In addition, the risk score of the Society of Thoracic Surgeons was calculated for each patient. Before TAVI, all patients underwent heart catheterization to identify relevant coronary artery disease that would be treated by stenting. Furthermore, the patients underwent transthoracic echocardiography, and electrocardiographic-gated 256-slice cardiac computed tomography (Brilliance iCT, Philips Medical Systems, Best, The Netherlands) of the heart and computed tomographic angiography of the abdominal aorta and pelvic and femoral arteries. The main exclusion criteria for percutaneous aortic valve implantation were an aortic annulus diameter of <19 or >27 mm and access artery diameters of <6 mm. Of these 108 patients, 87 were >80 years old (85 ± 2.7 years). All patients were informed of the specific risks and alternatives of TAVI and gave informed written consent for TAVI and pre- and postinterventional monitoring (data collection). The study protocol was in accordance with the local ethics committee guidelines.
All transfemoral aortic valve implantations were performed using the 18Fr CoreValve device (Medtronic, Minneapolis, Minnesota), as previously described. In brief, first an 18Fr delivery sheath was placed into the femoral artery, a transjugular pacemaker was placed into the right ventricle, and balloon valvuloplasty was performed under rapid pacing. Afterward, either a 26- or 29-mm CoreValve prothesis was implanted. The access site was closed using the Prostar XL 10-French system (Abbott Vascular, Abbott Park, Illinois). All procedures were performed with the patient under local anesthesia and analgosedation. The patients were transferred to our intensive care unit after the procedure for ≥48 hours. All patients developing new grade III atrioventricular block received a permanent pacemaker within 3 days after CoreValve implantation.
The Short Form 36-Item Health Survey was used for the quality of life assessment. This questionnaire has been previously used in geriatric populations and includes 36 items. It is grouped into 8 multi-item domains: physical functioning, role limitation due to physical health problems, bodily pain, general health, vitality as a measure of energy and fatigue, social functioning, role limitations due to emotional problems, and mental health related to psychological distress and psychological well-being. In addition, a mental component summary (MCS) and physical component summary (PCS) can be calculated as 2 metascores combining all multi-item domains and representing the overall physical and mental functioning. All patients were instructed to complete the questionnaire at a visit before admission and at the 6-month follow-up visit. The patients were able to complete the form either in the hospital or at home. The New York Heart Association (NYHA) class was assessed before TAVI and at the 6-month follow-up visit. Similarly, the blood samples were analyzed for N-terminal pro-brain natriuretic peptide levels before and 6 months after valve implantation.
All statistical analyses were performed using the Statistical Package for Social Sciences, version 12 (SPSS, Chicago, Illinois). The data are presented as the mean ± SD. Comparisons were performed using a paired t test or Fisher’s exact test (as appropriate). p Values <0.05 were considered statistically significant.
Results
Of the 108 patients, 87 (aged 85 ± 2.7 years) were successfully implanted without any procedural deaths. Of these 87 patients 6 died within 30 days after implantation. Patient 1 (EuroSCORE 26%; Society of Thoracic Surgeons score 52%) died at day 2 from mesenteric ischemia. Patient 2 (EuroSCORE 28%; Society of Thoracic Surgeons score 37%) died at day 17 from acute respiratory failure. Patient 3 (EuroSCORE 61%; Society of Thoracic Surgeons score 33%) died at day 16 from stroke and aspiration pneumonia. Patient 4 (EuroSCORE 76%; Society of Thoracic Surgeons score 20%) died at Day 2 from cardiogenic shock. Patient 5 (EuroSCORE 26%; Society of Thoracic Surgeons score 64%) died at day 4 from excitation-contraction uncoupling. Patient 6 (EuroSCORE 34%; Society of Thoracic Surgeons score 30%) died at day 3 from pneumonia and septicemia. Thus, the 30-day mortality rate was 6.9%, within the expected range reported in published studies. One patient (EuroSCORE 22%; Society of Thoracic Surgeons score 30%) died within the 6-month follow-up on day 125 from pneumonia and septicemia. Finally, 28 patients (35%) required pacemaker implantation; this rate was also within the published range of pacemaker dependency after CoreValve implantation.
The remaining 80 patients had an average age of 86 ± 2.9 years and all attended the 6-month follow-up visit and completed the Short Form 36-Item Health Survey questionnaire. Table 1 lists the main clinical baseline data of those patients who were able to complete the 6-month follow-up assessment.
| Characteristic | Value |
|---|---|
| Age (years) | 86 ± 2.9 |
| Women | 47 (59%) |
| Logistic European System for Cardiac Operative Risk Evaluation (%) | 24 ± 15.1 |
| Society of Thoracic Surgeons score (%) | 18.1 ± 10.2 |
| New York Heart Association class | |
| I | 0 |
| II | 11 (14%) |
| III | 50 (63%) |
| IV | 19 (24%) |
| Dyspnea | 78 (98%) |
| Syncope | 11 (14%) |
| Body mass index (kg/m 2 ) | 25.0 ± 3.6 |
| Diabetes mellitus | 61 (76%) |
| Hypertension | 71 (89%) |
| Coronary artery disease | 38 (48%) |
| Previous percutaneous coronary intervention | 22 (28%) |
| Previous coronary bypass surgery | 7 (9%) |
| Previous pacemaker implantation | 21 (26%) |
| Previous myocardial infarction within 90 days of procedure | 0 |
| Previous stroke | 11 (14%) |
| Left ventricular ejection fraction | |
| >50% | 44 (55%) |
| 30–50% | 25 (31%) |
| <30% | 11 (14%) |
| Atrial fibrillation | 27 (34%) |
| Peripheral vascular disease | 5 (8%) |
| Chronic obstructive pulmonary disease | 23 (29%) |
| Pulmonary hypertension >60 mm Hg | 18 (23%) |
| Creatinine >200 μmol/L | 9 (11%) |
The immediate procedural success was confirmed by invasive measurement of the transvalvular peak-to-peak gradient and was <5 mm Hg in all patients. This was confirmed by the echocardiographic results, showing a significant reduction in the peak aortic valve gradient (before 68.3 ± 21.3 mm Hg; after 10.5 ± 5.6 mm Hg; p <0.0001) and mean aortic valve gradient (before 42.1 ± 14.5 mm Hg; after 4.6 ± 3.2 mm Hg; p <0.0001).
The average scores of all 8 health components improved significantly after TAVI. Physical functioning improved from 23.4 ± 6.0 to 67.8 ± 13.7 (p <0.001), role functioning from 32.1 ± 8.7 to 64.1 ± 10.7 (p <0.001), bodily pain from 37.5 ± 9.4 to 51.3 ± 11.5 (p <0.05), general health from 31.4 ± 10.1 to 62.7 ± 11.3 (p <0.001), vitality from 33.1 ± 9.8 to 64.1 ± 13.2 (p <0.001), social functioning from 40.3 ± 9.1 to 81.1 ± 9.6 (p <0.001), role emotional from 36.2 ± 8.2 to 67.1 ± 9.5 (p <0.001), and mental health scores from 40.3 ± 9.4 to 64.2 ± 10.6 (p <0.01; Figure 1 ).

The greatest improvement in the physical components was seen with physical functioning (190% increase) and the lowest with bodily pain (37% increase). The greatest improvement in the mental components was seen with vitality (94% increase) and the lowest with mental health (59% increase).
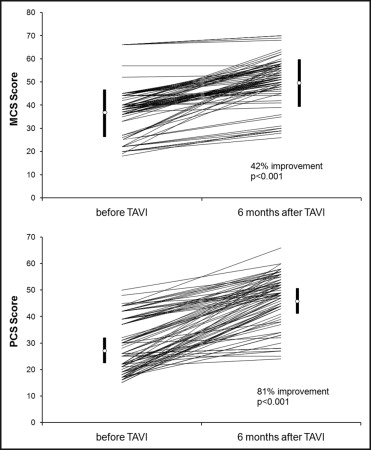
The metascores confirmed the significant improvements, with the PCS increasing from 28.4 ± 10 to 46.8 ± 9.2 (p <0.001) and the MCS increasing from 37.3 ± 10.8 to 50.6 ± 10.1 (p <0.001). Figure 2 shows all individual patients and their PCS and MCS scores. No patient had a decrease in any score. However, 6 patients had an increased PCS score of <10% and 12 patients had an increased MCS score of <10%. These patients were analyzed further. These patients had the same average age as the whole study population but a higher EuroSCORE (34 ± 14%) and Society of Thoracic Surgeons score (30 ± 14%; p <0.05), indicating more advanced morbidity. This was even more pronounced when considering those patients with a <10% improvement in PCS (average EuroSCORE of 54 ± 7%; Society of Thoracic Surgeons score 34 ± 8%; p <0.05 vs the responder group). The incidence of chronic obstructive pulmonary disease was significantly greater in both nonresponder groups (p <0.05). In contrast, the incidence of previous stroke and an ejection fraction <35% was only significantly greater in the PCS nonresponder group (both p <0.001). The baseline MCS and PCS scores in the nonresponder group were similar to the overall baseline average.