A substantial proportion of patients who meet the current guidelines for cardiac resynchronization therapy (CRT) fail to respond to this pacing modality. Although appropriate patient selection and left ventricular (LV) lead location have been ascribed as determinants of CRT response, the interaction among contractile reserve, dynamics of dyssynchrony, and lead location is not well understood. The present study prospectively evaluated the effect of contractile reserve and dobutamine-induced changes in LV synchrony, in relation to the LV lead location, as predictors of the response to CRT. In the present study, 31 patients were prospectively evaluated and underwent low-dose dobutamine echocardiography. The dobutamine-induced increase in ejection fraction (contractile reserve [CR]) was measured, and the most mechanically delayed segment was identified to classify patients into 2 groups. Group 1 had a CR of >20% and a LV lead position concordant with the mechanically delayed segment. Group 2 included the remaining patients (i.e., low CR, discordant LV lead position, or both). Patients in group 1 were significantly more likely to have an echocardiographic response at 6 months (80% of group 1 vs 29% of group 2, p = 0.018) and had an improved 2-year heart failure hospitalization-free survival rate (90% in group 1 vs 33% in group 2, p = 0.006). In conclusion, low-dose dobutamine echocardiography provides information that can help to predict responders to CRT. The response rates and heart failure hospitalization-free survival were improved in those patients with a CR >20% and an LV lead tip concordant with the most delayed mechanical segment.
Cardiac resynchronization therapy (CRT) has been shown to improve the quality of life, decrease heart failure hospitalizations, and improve mortality in an expanding subset of patients with heart failure by improving the mechanical function of the heart, reducing arrhythmia, and promoting electrical and mechanical remodeling. However, a substantial proportion of patients who meet the current guidelines for CRT fail to respond to this therapeutic modality. Appropriate patient selection and left ventricular (LV) lead location have been ascribed as determinants of CRT response. Multiple studies have independently evaluated the roles of contractile reserve (CR) measured using dobutamine stress echocardiography, intraventricular dyssynchrony measured by tissue Doppler imaging (TDI), and LV lead location to predict the CRT response. However, little information is available regarding their combined role. In the present study, we prospectively evaluated whether the presence of CR, and a LV lead position concordant with the most mechanically delayed segment (MDS) during low-dose dobutamine infusion could help to identify responders to CRT.
Methods
Patients with ischemic or nonischemic cardiomyopathy who met clinical criteria for CRT were enrolled. The exclusion criteria included severe chronic obstructive lung disease (patients requiring oral steroids and bronchodilators), co-morbidities that would result in a limited lifespan of <6 months, a high burden of premature ventricular beats (>10/hour), contraindications to dobutamine (i.e., unstable angina), and severe aortic stenosis (aortic valve area < 1.0 cm 2 ). The institutional review board at Massachusetts General Hospital reviewed the study protocol and consent forms, and all patients provided written informed consent.
Each patient underwent baseline dobutamine echocardiography within 2 weeks (mean 2.2 ± 2.1 days) of device implantation with the device turned off in those in whom the echocardiographic assessment occurred after implantation (n = 19). Dobutamine was intravenously infused initially at a rate of 5 μg/kg/min for 3 minutes and titrated upward to a maximum of 10 μg/kg/min for 2 minutes before the start of image acquisition. Dobutamine was maintained at an infusion rate to increase the heart rate up to 50% over baseline but not >120 beats/min. An infusion rate of 10 μg/kg/min was never exceeded.
The images were acquired, and analysis was performed with the patient both at rest and with dobutamine infusion with the GE Vivid 7 (GE Medical Systems, Wauwatosa, Wisconsin) and on a computer workstation (EchoPAC, GE Medical Systems). Two-dimensional and TDI (frame rate >140 frames/s) were performed in the standard views. The LV ejection fraction was calculated from the LV volumes obtained by the biplane method of disks in the apical 2- and 4-chamber views. The interval to the peak systolic velocities was assessed for 12 segments in the basal and mid-locations of the septum, lateral, anteroseptal, posterior, anterior, and inferior walls. The measurements were averaged from 3 cardiac cycles (5 if atrial fibrillation were present). The MDSs were defined from TDI as the segments with the longest interval between QRS onset and peak systolic longitudinal velocity both at rest and with dobutamine infusion. To account for beat to beat variability and for the limits in temporal resolution of TDI, the segments within 5 ms of the most delayed segment were also counted as the MDSs. Thus, a given patient could have >1 MDS. The echocardiographic response to CRT was defined as a reduction in end-systolic volume of ≥15%. All patients had standard (fixed) out-of-the box CRT device settings of the atrioventricular timing and for the offset between the LV and right ventricular leads (VV offset) for the first 6 months, following which all patients underwent echocardiographic optimization.
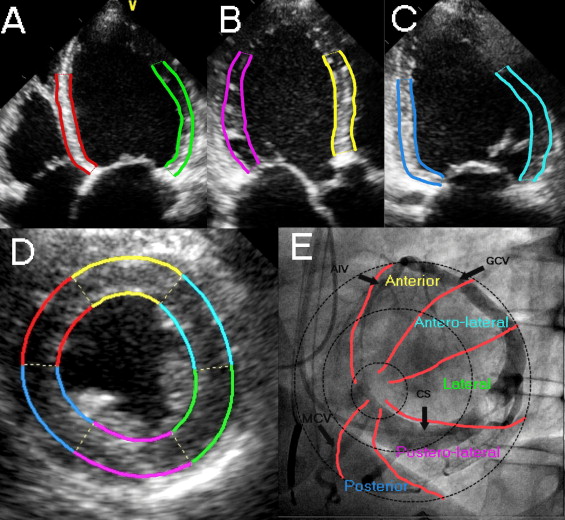
Each patient underwent de novo placement of a CRT device or an upgrade from an existing pacemaker or defibrillator. The LV lead was placed by way of the coronary sinus with the intention of placement in a lateral or posterolateral site, when possible. The operator had no knowledge of the MDS during lead implantation. Classification of the LV lead position was determined by analysis of the intraprocedural venograms and postprocedural chest radiograph. The lead position was characterized as being in 1 of 5 segments: anterior, anterolateral, lateral, posterolateral, or posterior, as previously described. To determine lead concordance, the basal and mid-segments analyzed during TDI were grouped together for a 6-segment model of septal, lateral, anteroseptal, posterior, anterior, and inferior. Each of the 5 lead position segments corresponded anatomically to a TDI segment: the anterior lead position to the anteroseptal segment; the anterolateral lead position to the anterior segment; the lateral lead position to the lateral segment; the posterolateral lead position to the posterior segment; and the posterior lead position to the inferior segment. The septal segment on TDI had no corresponding lead position segment ( Figure 1 ). The lead was considered concordant if the lead position segment corresponded to the MDS determined during dobutamine infusion or was within 1 adjacent segment.
The patients were divided into 2 groups for analysis. The patients in group 1 had both a significant CR and a concordant LV lead position with a MDS during dobutamine infusion. Group 2 included all other patients (i.e., discordant lead position, no significant CR, or both). Follow-up echocardiography was performed at 6 months. For those patients who died before that point, the latest available echocardiogram was used for follow-up analysis. Echocardiographic responders were defined as those patients with a reduction in the LV end-systolic volume of ≥15%. Hospitalizations for heart failure and all-cause mortality within 2 years were determined by review of the hospital and public records. Heart failure hospitalization was defined as inpatient admission with signs and/or symptoms of heart failure, including shortness of breath, peripheral edema, and/or congestion on the chest radiograph and improvement of these signs and/or symptoms with medical therapy.
Continuous variables are expressed as the mean ± SD and were compared using the unpaired 2-tailed Student’s t test. Categorical variables are expressed as a percentage and were compared using Pearson’s chi-square test or Fisher’s exact probability test, as appropriate. Survival curves were constructed using the Kaplan-Meier method and compared using the log-rank test for significance. p Values <0.05 were considered statistically significant. Statistical analysis was performed using JMP, version 8.0.2 (SAS Institute, Cary, North Carolina) and Microsoft Excel (Microsoft, Redmond, Washington).
Results
A total of 31 patients were enrolled in the present study, of whom 10 were in group 1 (presence of both CR and an LV lead position concordant with an MDS during low-dose dobutamine infusion) and 21 were in group 2. The baseline characteristics of all enrolled patients and stratified by group are summarized in Table 1 . Groups 1 and 2 had similar baseline characteristics.
| Variable | All Patients (n = 31) | Group 1 (n = 10) | Group 2 (n = 21) | p Value |
|---|---|---|---|---|
| Men | 23 (74%) | 6 (60%) | 17 (81%) | 0.38 |
| Age (years) | 68 ± 12 | 66 ± 9 | 69 ± 13 | 0.54 |
| Ischemic etiology | 20 (65%) | 4 (40%) | 16 (76%) | 0.10 |
| Medications | 1.0 | |||
| β Blocker | 30 (97%) | 10 (100%) | 20 (95%) | |
| Angiotensin-converting enzyme inhibitor/angiotensin receptor blocker | 21 (68%) | 7 (70%) | 14 (67%) | |
| Diuretic | 28 (90%) | 9 (90%) | 19 (90%) | |
| Left ventricular ejection fraction (%) | 28 ± 6 | 27 ± 6 | 28 ± 6 | 0.73 |
| Left ventricular end-systolic volume (cm 3 ) | 116 ± 40 | 121 ± 55 | 114 ± 31 | 0.73 |
| Left ventricular end-diastolic dimension (mm) | 61 ± 7 | 62 ± 8 | 61 ± 6 | 0.79 |
| QRS duration (ms) | 158 ± 22 | 153 ± 16 | 161 ± 24 | 0.33 |
| Change in mechanically delayed segment with dobutamine stress echocardiography | 19 (61%) | 5 (50%) | 14 (67%) | 0.44 |
| New York Heart Association functional class | 0.53 | |||
| III | 28 (90%) | 10 (100%) | 18 (86%) | |
| IV | 3 (10%) | 0 (0%) | 3 (14%) | |
| Contractile reserve present | 20 (65%) | 10 (100%) | 10 (41%) | |
| Concordant lead with mechanically delayed segment during dobutamine echocardiography | 17 (55%) | 10 (100%) | 7 (33%) |
All patients completed the dobutamine infusion protocol successfully with no significant adverse events, including ventricular arrhythmia. For the entire population, during dobutamine infusion, the mean heart rate increased by 17 ± 14 beats/min. The mean systolic blood pressure increased by 11 ± 20 mm Hg, and the mean diastolic blood pressure decreased by 3 ± 17 mm Hg. No difference was found between groups 1 and 2 in the changes in heart rate, systolic blood pressure, or diastolic blood pressure with dobutamine infusion (p = 0.58, p = 0.92, and p = 0.65, respectively).
For the entire population, the mean relative increase in the LV ejection fraction with dobutamine was 28 ± 31%. Group 1 had a significantly greater relative increase in the LV ejection fraction with dobutamine (29 ± 8% vs 10 ± 27%, p = 0.006); 12 patients (36%) at rest and 6 patients (18%) with dobutamine had ≥1 segment that had an interval to peak systolic velocity within 5 ms of the MDS and thus had >1 segment characterized as an MDS.
The results of follow-up are summarized in Table 2 . Patients in group 1 were significantly more likely to have an echocardiographic response than patients in group 2 and had significantly greater improvement in the end-systolic volume compared to group 2. Kaplan-Meier analysis showed that patients in group 1 had significantly improved heart failure hospitalization-free survival compared to group 2 ( Figure 2 ). At the end of 2 years of follow-up, a greater proportion of patients in group 1 had survived free of heart failure hospitalization than in group 2. The patients in group 1 also had improved 2-year all-cause mortality.



