Described is a 41-year-old man who at age 6 had partial resection of an obstructed right ventricular outflow tract with insertion of a patch and closure of a ventricular septal defect (tetralogy of Fallot). At age 41, cardiac transplantation was performed because of right ventricular outflow patch aneurysm, numerous episodes of ventricular tachycardia, and chronic heart failure, all features of the familial form of arrhythmogenic right ventricular cardiomyopathy (ARVC). Additionally, the patient had bundle branch block and epsilon waves on electrocardiogram, other features of ARVC. The case is described to introduce the concept of acquired ARVC, because the patient had many of the clinically recognized features of familial ARVC.
Arrhythmogenic right ventricular cardiomyopathy (ARVC) is characterized by localized thinning of the right ventricular (RV) wall with the localized portion consisting mainly of fibrofatty tissue. The thinning of the RV wall commonly leads to aneurysm formation. ARVC also is characterized by the presence of epsilon waves, bundle branch block, late potentials, and ventricular tachyarrhythmias on the electrocardiogram. ARVC has been recognized exclusively as a familial disease with autosomal dominant inheritance. In this report, we introduce the concept of acquired ARVC in a patient who was operatively treated for tetralogy of Fallot and later developed features of ARVC.
Case Description
A 41-year-old man, born on October 10, 1969, had a right Blalock-Taussig shunt placed in 1974, at 4 years of age, for tetralogy of Fallot. In 1976, at age 6, he underwent widening of the RV outflow tract using a Dacron patch (4.5 × 3 cm) and closure of a large (2 × 3 cm) subaortic ventricular septal defect. Preoperatively, the peak systolic pressure gradient between the right ventricle and pulmonary trunk had been 85 mm Hg. The patch extended through the nonobstructive pulmonary valve, and 2 of its 3 cusps were excised. The Blalock-Taussig shunt was ligated. Immediately after operation, the peak systolic RV pressure was 70 mm Hg and that in the pulmonary trunk 35 mm Hg. The peak systolic left ventricular pressure was 100 mm Hg.
The patient thereafter was asymptomatic until 26 years of age, when he had his first episode of ventricular tachycardia (VT). Transthoracic echocardiogram performed at age 26 revealed a peak systolic pressure gradient between the right ventricle and pulmonary trunk of 25 mm Hg, marked RV dilatation, a mildly dilated left ventricular cavity, severely depressed right and left ventricular ejection fractions, and severe pulmonary regurgitation. An electrophysiologic study at the time disclosed sustained monomorphic VT with left bundle branch block morphology and superior axis. Mapping disclosed the VT to involve the RV infundibulum (that myocardium between the residual pulmonary valve and tricuspid valve) in a counterclockwise activation pattern. Radiofrequency ablation failed to terminate the VT, and it resulted in acute lengthening of the cycle length from 375 to 420 ms. The VT was then terminated with ventricular burst pacing. Repeat stimulation did not induce further VT. The patient was placed on atenolol and propafenone.
At 27 years of age, 8 months later, the patient had runs of VT again, and a second electrophysiologic study was done. Again, the inducible VT was mapped to involve the RV infundibulum but this time in a bidirectional activation pattern. A total of 23 linear and point radiofrequency ablations were made, and on several occasions the VT was terminated. Nevertheless, the VT was still inducible. Ablation prolonged the cycle length from 380 to 450 ms.
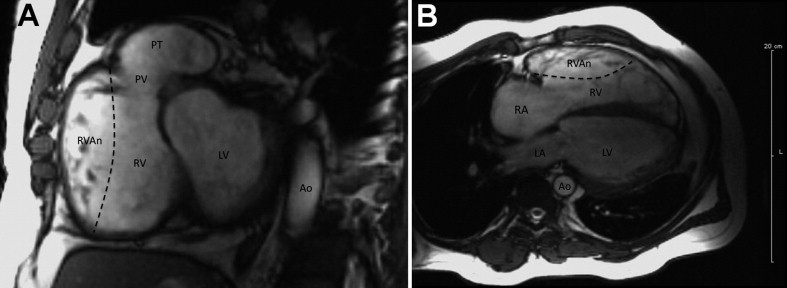
For several years thereafter, the patient was lost to follow-up. He started using alcohol and marijuana heavily. He quit taking all medications. At 36 years of age, he presented again to the hospital with chest pain, which was preceded by a viral gastroenteritis. His troponin level was 25 ng/ml. An electrocardiogram showed sinus tachycardia, a QRS duration of 200 ms, right bundle branch block, and nonspecific ST-T changes. Cardiac catheterization disclosed normal coronary arteries, normal mean pulmonary arterial pressures, no RV outflow obstruction, and no shunts. Transthoracic echocardiogram showed severely depressed RV and left ventricular function. Magnetic resonance imaging disclosed marked dilatation of the RV outflow tract ( Figure 1 ). An automated internal cardiac defibrillator with a biventricular pacing device was implanted.
At 40 years of age, the patient began experiencing multiple episodes of automated internal cardiac defibrillator firings and symptoms of severe heart failure ( Table 1 ). Cardiac computed tomography disclosed again severe dilatation of the RV outflow tract and heavy calcific deposits in its wall ( Figure 2 ). Electrocardiogram now showed epsilon waves in the right precordial leads, T-wave inversions, and complete right bundle branch block ( Figure 3 ). In February 2010, chronic inotropic therapy was initiated. The patient stopped using alcohol and marijuana completely. Six months later, when hospitalized for severe heart failure, runs of monomorphic nonsustained VT were demonstrated ( Figure 4 ). On November 7, 2010, heart transplantation was performed.



